Abstract
Background
Although the bortezomib-based triple-drug therapy is considered as a front-line therapy for multiple myeloma (MM) in Chinese patients, increased level of toxicity leads to treatment dissatisfaction. Treatment with ixazomib, an oral proteasome inhibitor, has demonstrated better efficacy and safety profile without increasing the toxicity. In this study, we investigate the safety and clinical outcomes of Chinese patients with newly diagnosed MM (NDMM) who transitioned from a bortezomib-based triple-drug therapy to an ixazomib-based triple-drug therapy in a real-world clinical setting.
Methods
This will be an open-label, single-arm, multicenter, prospective, observational study will recruit Chinese patients (aged ≥ 18 years) diagnosed with NDMM using International Myeloma Working Group (IMWG) criteria and who have received a bortezomib-based triple-drug therapy for more than two cycles as initial therapy. The previous bortezomib-based triple-drug therapy may include bortezomib, cyclophosphamide, and dexamethasone or lenalidomide, bortezomib, and dexamethasone or bortezomib, doxorubicin, and dexamethasone or bortezomib, thalidomide, and dexamethasone. At the time of enrollment, patients must have achieved at least partial response as defined by IMWG criteria. Approximately 320 eligible patients at 15 top MM hospitals in China will be treated with ixazomib triple-drug therapy and followed up once every 3 months for 24 months, unless specified. The primary endpoint is to assess progression-free survival at 2 years for Chinese patients with NDMM who have transitioned from a bortezomib-based triple-drug therapy to ixazomib-based triple-drug therapy. The clinical effectiveness, safety and tolerability, patient-reported outcomes, and health economic/resource utilization will be evaluated as secondary endpoints.
Planned Outcomes
The results from this study may provide evidence to verify the benefits of transitioning from bortezomib-based triple-drug therapy to ixazomib-based triple-drug therapy in Chinese patients with NDMM in a real-world clinical setting.
Trial Registration
The study has been registered at clinicalTrials.gov (NCT05013190).
Similar content being viewed by others
Long-term, parenteral administration, bortezomib-based triple-drug therapy is first-line treatment of Chinese patients with MM associated with higher incidence of adverse events. |
Oral administration of the drug over parenteral administration is convenient, with ixazomib-based therapy providing beneficial results in previous trials. |
This study will assess the effectiveness and safety of ixazomib in patients who transitioned from a bortezomib-based triple-drug therapy to an ixazomib-based triple-drug therapy in a real-world clinical setting. |
This study findings may indicate potential for a reduced economic and disease burden among Chinese patients with MM. |
Introduction
Background
Multiple myeloma (MM) accounts for 1% of all malignant cancers and nearly 13% of hematological malignancies [1, 2]. In the USA alone, it is estimated that there will be 34,920 new cases and 12,410 deaths in 2021 [3]. Most frequently, myeloma is diagnosed among people aged 65–74 years with a median age of 69 years [4]. The incidence of MM in China, although lower than in Western countries, has been increasing in recent years. According to the latest statistics, the incidence of MM in China is 1.6/10,00,00 per person-years [5], with an estimated 21,116 new cases and 16,182 deaths per year [6]. In addition, the mean age of patients diagnosed in China is 58 years, which is 10 years younger than that of Caucasian population [5].
With the advent of autologous stem-cell transplantation and with the introduction of novel targeted drugs such as the proteasome inhibitor (PI) bortezomib and immunomodulatory drug thalidomide, the median overall survival (OS) in patients with MM has been improving significantly in recent years [1, 7, 8]. More recently, the treatment landscape has been further expanded with the use of newer-generation PIs, including ixazomib and carfilzomib, histone deacetylase inhibitors, monoclonal antibodies such as daratumumab and elotuzumab [9], chimeric antigen receptor T-cell therapy [10], and bispecific T-cell engagers [11]. Despite improvements from these treatment strategies, the disease remains incurable with signs of relapse and need for multiple lines of therapy.
Ixazomib is an orally bioavailable, reversible PI. Ixazomib in combination with lenalidomide and dexamethasone (IRd) is indicated for the treatment of patients with MM who have received at least one prior therapy. In an early phase I/II study, IRd regimen showed promising efficacy and manageable adverse events in patients with newly diagnosed MM (NDMM) [12]. A further phase 3 randomized trial confirmed the efficacy of this combination in patients with refractory or relapsed MM [13].
Bortezomib-containing triplets are the standard of care for the first-line treatment of patients with MM in China. Unfortunately, long-term treatment with this regimen was associated with higher incidence of adverse events such as peripheral neuropathy (PN) (5–11%) [14,15,16,17] and frequent need to visit the clinic due to parenteral administration [18, 19]. As a result, there is an increasing impact on economy and health due to bortezomib-based triple-drug therapy in China. In contrast to bortezomib-based triple-drug therapy, the phase 3 TOURMALINE-MM1 trial with ixazomib-based triple-drug therapy showed evidence of better safety profile without evidence of accumulating toxicity [13]. Oral regimens offer convenience to the patients, especially in China, because of the scarcity of top-tier MM centers and lack of well-established community healthcare service systems. Hence, frequent commuting between home and hospital is a burden for patients and their family. The feasibility of the in-class transition from a bortezomib-based induction to an all-oral ixazomib regimen has previously been demonstrated [20]. Overall good partial response (PR) rates and a tolerable safety profile make it possible to transition from a bortezomib-based induction regimen to an ixazomib-based triple-drug therapy in Chinese patients with MM. Post-marketing studies and clinical trials assessing the relative effectiveness of transitioning from bortezomib-based triple-drug therapy to ixazomib-based triple-drug therapy from a real-world clinical practice are lacking in China. There remains an unmet need to investigate and assess the safety and clinical outcomes of transitioning from bortezomib-based triple-drug therapy to ixazomib-based triple-drug therapy among Chinese patients with NDMM. Herein, we report the study design and protocol for assessing the effectiveness and safety of ixazomib in patients who transitioned from a bortezomib-based triple-drug therapy to an ixazomib-based triple-drug therapy in a real-world clinical setting.
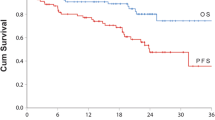
Study Objectives
The primary objective of the study is to determine the progression-free survival (PFS) at 2 years in Chinese patients with NDMM who had transitioned from a bortezomib-based triple-drug therapy to an ixazomib-based triple-drug therapy. Secondary objectives of the study are to evaluate the clinical effectiveness of the drug as denoted by the rates and duration of complete response (CR), time to next therapy, duration of therapy and overall survival (OS), safety and tolerability, and patient-reported outcomes (PRO), as well as to understand health economic/resource utilization in Chinese patients with NDMM when transitioning from bortezomib triple-drug therapy to ixazomib triple-drug therapy. Exploratory objectives will also be attempted to explore minimal residual disease (MRD) negative rate and sustain MRD negativity of Chinese patients with NDMM who switch from a bortezomib-based triple-drug therapy to ixazomib-based triple-drug therapy. It will also explore influence on medication adherence and the impact factors for clinical outcome along with response rate, PFS, and safety in a defined subgroup among Chinese patients with NDMM who switch from a bortezomib-based triple-drug therapy to ixazomib-based triple-drug therapy. The study endpoints for each objective are described in detail in Fig. 1.
Study endpoints for MODIFY. Abbreviations: AE adverse events; CR complete response, DOT duration of ixazomib therapy, IMWG International Myeloma Working Group, MRD minimal residual disease, OS overall survival, PD partial disease, PFS progression-free survival, RDI relative dose intensity, sCR stringent complete response, SPM secondary primary malignancies, TTNT time to next treatment, VGPR very good partial response
Methods
Trial Design
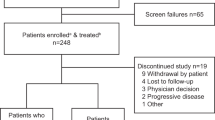
This is a national, multicenter, single-arm, open-label, prospective, pragmatic study among Chinese patients with MM. Patients (aged ≥ 18 years), first diagnosed with multiple myeloma (newly diagnosed multiple myeloma, NDMM) using International Myeloma Working Group (IMWG) criteria (please refer to the Supplementary Material for definition) and who received a bortezomib-based triple-drug regimen for more than two cycles as initial therapy, including bortezomib + cyclophosphamide + dexamethasone (VCD) or bortezomib + lenalidomide + dexamethasone (VRD) or bortezomib + doxorubicin + dexamethasone (PAD) or bortezomib + thalidomide + dexamethasone (VTD). Considering the risk of PN with increasing cumulative doses of bortezomib, the patients received fewer than four to six cycles of bortezomib-based triple-drug regimen as initial therapy. At the time of enrollment, patients must have achieved a minimum of a PR as defined by IMWG criteria. Patients who are transplant ineligible, and those who are eligible but are not expected to undergo transplantation for a minimum of 24 months, will be included. The estimated enrollment period will be 24 months. Approximately 320 patients from 15 top-tier hospitals in China will be recruited. Patient enrollment in the participating centers will be based on the physicians’ judgment of eligibility for treatment with ixazomib-based triple therapy. Institutional ethical approval and written informed consent will be obtained from all the patients before participation. Consecutive patients who fulfill the inclusion criteria and are willing to participate will be considered (Table 1). All patients will be followed up once every 3 months for 24 months except in cases of withdrawal of their informed consent or death or loss to follow-up or termination of the study by the sponsor, whichever occurs first. The selected patients need to strictly follow the medication label for the dosage, route, frequency, and duration of treatment. This study will be conducted in accordance with the protocol, the current version of the Declaration of Helsinki, Good Pharmacoepidemiology Practices (GPP), ISPE GPP guideline, and any local regulations. The study has been registered at clinicalTrials.gov (NCT05013190).
Data Collection
For all the included patients, specific data will be collected at baseline, every 3 months for 24 months and at end of follow-up. Baseline data and disease characteristics, relevant medical history, and all initial and subsequent treatments for MM will be collected from patients after signing the informed consent form. Apart from routine demographic data, Charlson comorbidity index, the simplified frailty score [21], post-progression therapeutic management, and reasons for discontinuation of the study regimens will also be collected. Treatment discontinuation will include the date and reason for discontinuation of each agent in the study regimen. All agents in the treatment regimen may not be discontinued at the same time. The physician will make this decision on the basis of patient response to treatment. All these data will be recorded in an electronic case report form (eCRF), with each study site able to access data only from their own center.
Eligible patients will be evaluated for demographic information and medical history along with physical examinations including height, weight, body mass index (BMI), and vital signs (BP and heart rate) (Table 2). Further, ECOG performance status, 12-lead electrocardiogram (ECG), hematological, and biochemical evaluation, urine analysis, thyroid testing, radiographic disease assessment, β2-microglobulin, M-protein measurements by serum or urine protein electrophoresis, Ig quantification, serum-free light chain assay, immunofixation of serum and urine, bone marrow aspiration, biopsy for disease assessment, and MRD assessment will also be assessed. Cytogenetic data will also be collected, depending on availability. Hematology and biochemistry samples will be collected up to 3 days before day 1 dosing and 24 h before days 8, 15, and 22 of cycle 1, as required. PRO will be assessed every month through ePRO system through the EORTC QLQ-C30 (version 3), EORTC QLQ-MY20, EQ5D-5L, and TSQM-9 questionnaires. All the patients will be trained in filling up the ePRO system at baseline. If the electronic system is inoperative or the patient finds it difficult to understand how to use the ePRO system, the principal investigator or sub-principal investigator will contact the patients by telephone or ask them to visit the hospital to collect PRO data, which will be then entered by the staff into the system. Patient-reported medication adherence will be collected daily by patient-self management application during the ixazomib-based triple-drug therapy phase and until disease progression. Healthcare resource utilization and safety will also be assessed (Table 2).
Follow-up data for PFS will be collected during the routine care visits every 3 months until progression is documented, and then follow-up data for OS will be collected every 6 months for 24 months post-enrollment. The data collected will include patient status, disease management assessments, response to treatment with ixazomib, quality of life, and any other medications and safety assessments. Reporting of adverse events and concomitant medications will be monitored throughout the study period and at follow-up visits. The current Standard Coding Instructions for coding of medical history, concomitant illness (MedDRA), concomitant medication (WHO-Drug), and adverse events/reactions (MedDRA) will be followed. The ADR monitoring will follow six levels, that is, related, possibly related, suspected to be related, possibly not related, not related, and unevaluable. The detailed data to be collected during each visit are provided in Table 2.
Ixazomib-Based Triple-Drug Therapy
Patients will be treated with ixazomib triple-drug therapy [ixazomib, 4 mg; lenalidomide, 25 mg; dexamethasone, 40 mg (20 mg if over 75 years of age)] where the treatment schedule, dosage, route, frequency, and duration will be strictly followed through the ixazomib label (Fig. 2). According to ixazomib label, patients should be treated with ixazomib-based triple-drug therapy until progression or unacceptable toxicity leading to a discontinuation or change in therapy, for a maximum of 26 cycles (24 months). If a patient discontinues treatment with ixazomib before disease progression, they will enter the PFS follow-up period of the study until they experience disease progression, are lost to follow-up, or die, whichever occurs first. However, patients may continue to receive their ixazomib-based triple-drug therapy after their end of follow-up assessment at the treating physician’s discretion. Ixazomib will be administered on days 1, 8, and 15 of each 28-day cycle, while lenalidomide will be administered from days 1 to 21 and dexamethasone on days 1, 8, 15, and 22 of each cycle, respectively.
Treatment flowchart. Abbreviations: CR complete response, DOT duration of ixazomib therapy, IMWG International Myeloma Working Group, HRU healthcare resource utilization, MM multiple myeloma, MRD minimal residual disease, ORR objective response rate, OS overall survival, PAD bortezomib + doxorubicin + dexamethasone, PFS progression-free survival, PR partial response, PRO patient-reported outcomes, RDI relative dose intensity, VGPR very good partial response, VCD/CyBorD bortezomib + cyclophosphamide + dexamethasone, VRD bortezomib + lenalidomide + dexamethasone
Statistical Analysis
All data obtained in this study and recorded in the eCRF will be listed and summarized with statistics or frequency tables as appropriate. Continuous variables will be summarized by descriptive statistics, while categorical variables will be summarized using frequency and percentages. Descriptive analysis will be presented for the whole sample and for subgroup of patients after stratification of demographic and clinicopathological factors (i.e., stage of disease, gender, age, etc.). PR, very good partial response (VGPR), complete response (CR), stringent complete response (sCR), objective response rate (ORR), PFS, and OS will be calculated. Survival analysis will be assessed using the Kaplan–Meier (KM) method, and the median survival with corresponding 95% confidence intervals will be derived from respective KM curves. Safety will be evaluated by the incidence of adverse events (AEs), severity, and type of AEs, and through change from baseline in the patient’s vital signs, weight, and clinical laboratory results in the safety population. Exposure to ixazomib and reasons for discontinuation will be tabulated. Treatment-emergent adverse events that occur after administration of the first dose of ixazomib and through 30 days after the last dose of ixazomib will be tabulated. Data that are potentially spurious or erroneous will be examined according to standard data management operating procedures. AEs will be tabulated according to the MedDRA. For assessing healthcare resource utilization, outpatient visits to the study site, overnight hospital admissions, and emergency department visits will be analyzed. Healthcare resource utilization data will be entered via ePRO system. If for any reason ePRO is not used, then the data related to PROs will be administered either via telephone interview or the patients will visit the hospital to complete a paper version of the PROs. The principal investigator or sub-principal investigator and their staff will then capture this information into the electronic system.
Sample Size
Since this is a descriptive study, no statistical hypothesis will be generated. The sample size has been determined on the basis of practical considerations including the typical volume of patients with MM treated with ixazomib-based triple-drug therapy at participating investigative sites and cost. On the basis of the collected information and an assumed dropout rate of 10–15%, the expected sample size is approximately 320 for this study.
Interim Analysis
Three interim analyses will be performed as follows. The first interim analysis will be carried out when 100% of patients have been enrolled and will aim to describe the baseline characteristics to guide further study conduct. A second interim analysis will be conducted to describe clinical efficacy and safety after the completion of study drug regimen by the last patient. A third analysis will be performed to describe clinical efficacy and safety after 50% of the patients will complete a minimum of 12 months of follow up. Both the second and third interim analysis will also describe the outcomes related to PRO and health resource utilization.
Discussion
Despite availability of therapeutic options for the treatment of MM, the effectiveness and patient outcomes are not similar for different treatment options in the real-world setting compared with a controlled clinical trial. Although clinical trials are essential for determining the efficacy and safety of treatment for MM, real-world studies are becoming an absolute necessity that can help clinicians make informed decisions in improving patient care and quality of life [22, 23]. The reason for such discrepancies are several, including rigorous selection of patients excluding those with comorbidities and elderly [22], limitations in routine clinical practice due to toxicity and comorbidity burden, cost, patient and physician motivation, and differences in clinical care between treatment centers [23]. These differences might contribute to the gaps of efficacy and effectiveness between clinical trial and real-world outcomes.
Given that most patients become refractory to the existing standard therapies, ixazomib provides an opportunity to further explore the value of PIs in the treatment of NDMM. Although Asians, including Chinese, show a relatively lower incidence of MM than Caucasians, the actual incidence of MM in Asia is still higher because of the huge population [5]. A real-world study with 85 patients with NDMM in China, treated with first-line ixazomib triple-drug therapy showed high effectiveness in patients with MM with well-acceptable toxicity [24]. Similarly, other recently published studies demonstrated the efficacy of IRd regimen in Chinese patients with NDMM [25, 26]. However, since ixazomib was introduced in China only in 2018, real-world studies in China are limited. Furthermore, these studies are restricted by the limited sample size, shorter duration of follow-up, and absence of comprehensive evaluation of treatment outcomes by incorporating the patient’s perspective. This trial has been designed with an approach to systematically and prospectively collect integrative data including detailed clinical, biochemical, and laboratory data, imaging, treatment, quality of life, patient adherence to medication, and health utilization. The intended follow-up of this cohort for 2 years will give us a unique opportunity to integrate this large variety of data in the context of real-life myeloma care. Considering the inclusion of patients who are transplant ineligible and eligible, but who are not receiving stem cell transplant (SCT) in the front-line setting, we aim to recruit a broad and well-characterized patient cohort to meet our study objectives.
This is the first, large, real-world, cohort-based study in China that reflects the situation of transitioning from a bortezomib-based triple-drug therapy to ixazomib based triple-drug therapy. The results of this study may provide evidence to support the benefits of transitioning from bortezomib-based induction therapy to ixazomib-based therapy in Chinese patients with NDMM in a real-world clinical setting. We believe that the study could provide treatment information to help make informed decisions in clinical practice to ensure clinical effectiveness while reducing the burden of the disease and toxicity, which will ultimately guide in achieving the goals of maximal benefit with long-term treatment in patients with MM.
Limitations
This study may be limited by the nature of the design as an observational study, in comparison with randomized controlled trials, which can commonly provide stronger evidence on the efficacy of therapies.
Conclusion
The new study findings may provide comprehensive insights into patient and disease characteristics, outcomes, treatment patterns, patients’ health-related quality of life, and safety of treatment transition from bortezomib- to ixazomib-based treatment of Chinese patients with NDMM. These data will be of substantial importance to the MM community as well as to the patients who frequently relapse to standard treatments. We hope this will eventually reduce the economic and disease burden among the Chinese population who have this disease.
References
Palumbo A, Anderson K. Multiple myeloma. N Engl J Med. 2011;364:1046–60.
Raab MS, Podar K, Breitkreutz I, Richardson PG, Anderson KC. Multiple myeloma. Lancet. 2009;374:324–39.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA. 2021;71:7–33.
Myeloma—Cancer Stat Facts [Internet]. SEER. [cited 21 Apr 2021]. Available from: https://seer.cancer.gov/statfacts/html/mulmy.html
Wang S, Xu L, Feng J, Liu Y, Liu L, Wang J, et al. Prevalence and incidence of multiple myeloma in urban area in China: a national population-based analysis. Front Oncol [Internet]. 2020 [cited 21 Apr 2021];9. Available from: https://www.frontiersin.org/articles/https://doi.org/10.3389/fonc.2019.01513/full#B1
WHO. Globocan 2020 World Fact Sheet: China. [Internet]. [cited 21 Apr 2021]. Available from: https://gco.iarc.fr/today/data/factsheets/populations/160-china-fact-sheets.pdf
Kumar SK, Dispenzieri A, Lacy MQ, Gertz MA, Buadi FK, Pandey S, et al. Continued improvement in survival in multiple myeloma: changes in early mortality and outcomes in older patients. Leukemia. 2014;28:1122–8.
Röllig C, Knop S, Bornhäuser M. Multiple myeloma. Lancet. 2015;385:2197–208.
Larocca A, Mina R, Gay F, Bringhen S, Boccadoro M. Emerging drugs and combinations to treat multiple myeloma. Oncotarget. 2017;8:60656–72.
Wu C, Zhang L, Brockman QR, Zhan F, Chen L. Chimeric antigen receptor T cell therapies for multiple myeloma. J Hematol Oncol. 2019;12:120.
Topp MS, Duell J, Zugmaier G, Attal M, Moreau P, Langer C, et al. Anti-B-cell maturation antigen BiTE molecule AMG 420 induces responses in multiple myeloma. J Clin Oncol. 2020;38:775–83.
Kumar SK, Berdeja JG, Niesvizky R, Lonial S, Laubach JP, Hamadani M, et al. Safety and tolerability of ixazomib, an oral proteasome inhibitor, in combination with lenalidomide and dexamethasone in patients with previously untreated multiple myeloma: an open-label phase 1/2 study. Lancet Oncol. 2014;15:1503–12.
Moreau P, Masszi T, Grzasko N, Bahlis NJ, Hansson M, Pour L, et al. Oral ixazomib, lenalidomide, and dexamethasone for multiple myeloma. N Engl J Med. 2016;374:1621–34.
Durie BGM, Hoering A, Abidi MH, Rajkumar SV, Epstein J, Kahanic SP, et al. Bortezomib with lenalidomide and dexamethasone versus lenalidomide and dexamethasone alone in patients with newly diagnosed myeloma without intent for immediate autologous stem-cell transplant (SWOG S0777): a randomised, open-label, phase 3 trial. Lancet. 2017;389:519–27.
Sonneveld P, Goldschmidt H, Rosiñol L, Bladé J, Lahuerta JJ, Cavo M, et al. Bortezomib-based versus nonbortezomib-based induction treatment before autologous stem-cell transplantation in patients with previously untreated multiple myeloma: a meta-analysis of phase III randomized, controlled trials. J Clin Oncol. 2013;31:3279–87.
Cavo M, Tacchetti P, Patriarca F, Petrucci MT, Pantani L, Galli M, et al. Bortezomib with thalidomide plus dexamethasone compared with thalidomide plus dexamethasone as induction therapy before, and consolidation therapy after, double autologous stem-cell transplantation in newly diagnosed multiple myeloma: a randomised phase 3 study. Lancet. 2010;376:2075–85.
Moreau P, Avet-Loiseau H, Facon T, Attal M, Tiab M, Hulin C, et al. Bortezomib plus dexamethasone versus reduced-dose bortezomib, thalidomide plus dexamethasone as induction treatment before autologous stem cell transplantation in newly diagnosed multiple myeloma. Blood. 2011;118:5752–8 (quiz 5982).
Baz R, Lin HM, Hui A-M, Harvey RD, Colson K, Gallop K, et al. Development of a conceptual model to illustrate the impact of multiple myeloma and its treatment on health-related quality of life. Support Care Cancer. 2015;23:2789–97.
Osborne TR, Ramsenthaler C, de Wolf-Linder S, Schey SA, Siegert RJ, Edmonds PM, et al. Understanding what matters most to people with multiple myeloma: a qualitative study of views on quality of life. BMC Cancer. 2014;14:496.
Manda S, Yimer HA, Noga SJ, Girnius S, Yasenchak CA, Charu V, et al. Feasibility of long-term proteasome inhibition in multiple myeloma by in-class transition from bortezomib to ixazomib. Clin Lymphoma Myeloma Leuk. 2020;20:e910–25.
Facon T, Dimopoulos MA, Meuleman N, Belch A, Mohty M, Chen W-M, et al. A simplified frailty scale predicts outcomes in transplant-ineligible patients with newly diagnosed multiple myeloma treated in the FIRST (MM-020) trial. Leukemia. 2020;34:224–33.
Chari A, Romanus D, Palumbo A, Blazer M, Farrelly E, Raju A, et al. Randomized clinical trial representativeness and outcomes in real-world patients: comparison of 6 hallmark randomized clinical trials of relapsed/refractory multiple myeloma. Clin Lymphoma Myeloma Leuk. 2020;20:8-17.e16.
Richardson PG, San Miguel JF, Moreau P, Hajek R, Dimopoulos MA, Laubach JP, et al. Interpreting clinical trial data in multiple myeloma: translating findings to the real-world setting. Blood Cancer J [Internet]. 2018 [cited 23 Apr 2021];8. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6226527/
Li J, Bao L, Xia Z, Wang S, Zhou X, Ding K, et al. Ixazomib-based frontline therapy in patients with newly diagnosed multiple myeloma in real-life practice showed comparable efficacy and safety profile with those reported in clinical trial: a multi-center study. Ann Hematol. 2020;99:2589–98.
Ding K, Yu H, Shao Y-Y, Li L-Y, Wang C-M, Song J, et al. Real-world data on the efficacy and safety of ixazomib-based therapy in multiple myeloma: a single-center study in China. Cancer Manag Res. 2020;12:8935–41.
He Y, Zhang K, Zou L, Chen S, Jiang D, Hu J, et al. Clinical study on ixazomib in the treatment of multiple myeloma. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2020;45:322–7.
Acknowledgements
Funding
This study and the journal’s Rapid Service Fee and Open Access Fee is being funded by Takeda (China) International Trading Co., Ltd., an affiliation of Takeda Pharmaceutical company.
Medical Writing and Editorial Assistance
Medical writing was supported by Anwesha Mandal and Dr Amit Bhat from Indegene, Pvt Ltd and funded by Takeda (China) International Trading Co., Ltd.
Author Contributions
Drs Chen and Liu, and Lin Li, contributed to the concept design of the study. Drs Chen and Liu participated in execution, acquisition, analysis and interpretation of the data. All authors revised and commented on the submitted manuscript, read and approved the final version.
Disclosures
Dr. Wenming Chen received lecture fees and served on the advisory board of Takeda (China) International Trading Co., Ltd. Dr. Aijun Liu received lecture fees and served on advisory board of Takeda (China) International Trading Co., Ltd. Lin Li is the employee of Takeda (China) International Trading Co., Ltd.
Compliance with Ethics Guidelines
Approval will be obtained from all ethics committees before the study commences, and written informed consent will be obtained from all the patients before participation. This study will be conducted in accordance with the protocol, the current version of the Declaration of Helsinki, Good Pharmacoepidemiology Practices (GPP), ISPE GPP guideline and any local regulations. The study protocol itself was approved by the ethics review boards and committees of Beijing Chao-Yang Hospital, Tianjin Medical University General Hospital, The First Affiliated Hospital of Soochow University, the First Affiliated Hospital of Zhengzhou University, the Anhui oncology hospital, Beijing Jishuitan Hospital, the West China Hospital of Sichuan University, the Shengjing Hospital of China Medical University, Qingdao Municipal Hospital, Henan Provincial People’s Hospital, the First Affiliated Hospital of Nanchang University, and the Affiliated Hospital of Inner Mongolia Medical University.
Data Availability
The datasets, including the redacted study protocol, redacted statistical analysis plan, and individual participants’ data supporting the results reported in this article, will be made available within three months from initial request, to researchers who provide a methodologically sound proposal. The data will be provided after its de-identification, in compliance with applicable privacy laws, data protection and requirements for consent and anonymization.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Chen, W., Liu, A. & Li, L. The MODIFY Study Protocol: An Open-Label, Single-Arm, Multicenter, Prospective Pragmatic Study of Ixazomib-Based Triple-Drug Therapy in Chinese Patients with Multiple Myeloma. Adv Ther 40, 705–717 (2023). https://doi.org/10.1007/s12325-022-02355-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02355-3