Abstract
Introduction
Essential tremor (ET) affects approximately 7 million people in the USA, yet public recognition of the disease and its impact remain low.
Methods
A retrospective observational study examined US claims data from 2015 to 2019 using the Compile database. ET diagnoses were captured using longitudinal data from 2015 to 2019 and for the year 2019, with diagnosis estimates extrapolated to the general US population. Confirmed ET was identified by an ET diagnosis code with at least two relevant prescriptions or by two diagnosis codes for ET and unspecified tremor at least 90 days apart. Comorbidity and treatment use data were extracted, and medication compliance and 2-year treatment persistence were assessed as measures of treatment adherence.
Results
A total of 1,336,183 patients with ET diagnoses codes were identified from 2015 through 2019, corresponding to 2,226,971 projected US diagnoses. In 2019, 128,263 patients had a confirmed ET diagnosis, corresponding to 213,772 projected US confirmed diagnoses. Of these, 96% had at least one comorbidity, and 64% received at least one pharmacologic treatment. Propranolol (24%) and primidone (20%) comprised the most common ET prescriptions. Two-year medication discontinuation rates were approximately 40%.
Conclusion
Our findings revealed that 1 million people were diagnosed and sought treatment for ET in the USA from 2015 to 2019. Projected population estimates of approximately 2 million people diagnosed suggest a further 1 million remain untreated. Our findings highlight the complexity of patient care in ET, complicated by delayed diagnoses, multiple comorbidities, and lack of effective and tolerable therapies that can mitigate treatment adherence limitations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Despite being one of the most common movement disorders, essential tremor (ET) is frequently undiagnosed or misdiagnosed, undertreated, or untreated, with only one pharmacologic option approved by the US Food and Drug Administration. |
The undesirable side-effect profiles, high discontinuation rates, and limited efficacy associated with available pharmacological and surgical options further highlight the need for additional treatment options and greater understanding of ET and its impact on patients in a real-world setting. |
The objective of this study was to describe diagnosis patterns, associated comorbidities, as well as treatment usage and adherence in patients with ET using administrative claims data from a large US insurance database spanning a 5-year period from 2015 to 2019. |
What was learned from the study? |
Our findings from a large US insurance database revealed that approximately 1 million people were diagnosed and actively sought pharmacologic treatment for ET from 2015 through 2019; however, projected US population estimates of approximately 2 million diagnosed and current treatment rates suggest that a further 1 million patients remain untreated. |
While two in three patients receive pharmacological treatment for ET, primarily propranolol or primidone, discontinuation rates are high. Notably, prescribing patterns vary between neurologists and non-neurologists; the latter are more likely to prescribe beta-blockers. |
Patient care in ET is complex, and complicated by delayed diagnoses, multiple comorbidities, and lack of effective and tolerable therapies that can mitigate treatment adherence limitations. This complexity underscores the hidden patient impact in ET and highlights the urgent unmet need for more efficient diagnosis and treatment options. |
Introduction
Essential tremor (ET) is one of the most common movement disorders. It is typically marked by tremor in the upper limbs, but may also involve the head, voice, lower limbs, and trunk [1,2,3]. In the USA, it is projected that approximately 7 million people have ET, representing more than 2% of the total population [4, 5]. ET prevalence increases with age, affecting 0.8% of people aged 18–30 years, and slightly more than 8% of people aged 85 years or older [5]. Importantly, increasing evidence suggests patient impact extends beyond tremor symptomatology. In a case–control study of 89 patients with ET, about 85% reported functional disability on at least one of the 31 items included in the Tremor Disability Questionnaire [6]. In the same study, the presence of depression or anxiety increased the rates of self-reported functional disability, highlighting the implications of comorbid conditions in ET.
Despite its high prevalence, ET is still frequently undiagnosed or misdiagnosed [7,8,9,10,11,12], and public recognition of the disease and its impact remain low. In a survey of patients and accompanying caregivers attending vascular, neurology, or movement disorders clinics, only about 10–30% of participants reported awareness of the condition [13]. Furthermore, many patients with ET, particularly those with mild tremors, do not seek medical care, remain undiagnosed, and do not receive treatment [14]. Delay in diagnosis was also observed in a random-digit dialing-based screening study of 419 enrollees in the New York metropolitan area, where four out of five patients who received an ET diagnosis during the study were previously undiagnosed [15]. Another, albeit smaller, screening study found that 91% (n = 89) of patients identified to have ET had not been previously diagnosed, and 97% had not received any treatment for their tremor, despite experiencing tremor-related disabilities [16]. Other studies have revealed the frequent misdiagnosis of ET, mainly due to symptom heterogeneity and ambiguity [7,8,9,10,11].
ET often remains undertreated or untreated, in part because of the limited number of available treatments, with only one pharmacologic option approved by the US Food and Drug Administration in 1967—propranolol [17]. Additional pharmacologic options used for off-label treatment for ET include primidone, gabapentin, topiramate, botulinum toxin type A, and benzodiazepines [1]. However, the undesirable side-effect profiles, limited efficacy, and associated high discontinuation rate for many of these agents suggest the need for additional treatment options [1, 18, 19]. Previous work has shown that, of those patients who receive pharmacologic treatment, approximately one in three eventually discontinue their prescribed medications, typically because of poor tolerability or limited efficacy [20]. Unilateral ventralis intermedius (VIM)–thalamic deep brain stimulation (DBS), radiofrequency thalamotomy, and unilateral magnetic resonance imaging-guided focused ultrasound thalamotomy represent surgical interventions for ET, although few patients resort to these as a last-line option because of their invasiveness and associated risk for irreversible side effects [1, 12, 21, 22].
The challenges associated with the diagnosis and treatment of ET underscore the need for a more comprehensive understanding of its impact on patients in a real-world setting. Importantly, greater insights into current practices surrounding the management of ET, including the difficulties faced by patients, may identify current care gaps. The objective of this study was, therefore, to further the understanding of the patient experience in ET through analysis of diagnosis patterns, associated comorbidities, and treatment usage and adherence using administrative claims data from a large insurance database spanning a 5-year period from 2015 to 2019.
Methods
Study Design and Data Source
This was a retrospective observational claims analysis utilizing the Compile database (https://www.compile.com/data), which captures over 27 billion insurance claims (both medical and pharmacy) for about 300 million unique patients since 2015 [23]. Overall, claims data in the database are sourced from clearinghouses, clearing switches, and claims data processors, and they represent about 65% of medical and 45% of pharmacy claims in the USA. Medical claims encompass about 30% of adjudicated and preadjudicated medical claims submitted to a payer, while pharmacy claims include data from retail and specialty pharmacies. The database captures data from a range of payer systems, including commercial plans, Medicare, Medicaid, Veterans Affairs, among others. Analyses in the current study included only deidentified data; thus, institutional review board approval was not required. Data were used with permission and under license from Compile Health.
Patient Identification and Study Cohorts
Total ET diagnoses were captured and included all diagnoses with at least one International Classification of Diseases, Tenth Revision (ICD-10) code for G25.0 (the diagnosis of ET). For a more conservative estimate, confirmed ET diagnoses were defined based on
-
The presence of an ICD-10 code of G25.0 denoting the diagnosis of ET, plus at least two relevant prescriptions for ET (e.g., propranolol, primidone, or other beta-blockers) or
-
The presence of an ICD-10 code of R25.1 for unspecified tremor and an ICD-10 code of G25.0 for ET, with diagnosis dates at least 90 days apart.
The requirements for at least two relevant prescriptions or an ICD-10 code for unspecified tremor in addition to an ET diagnosis ensured that identified patients were those truly diagnosed with ET and that they had other characteristics indicative of ET diagnosis, therefore increasing confidence of diagnosis.
ET Diagnoses in the Primary Study and Total Database Cohorts
The primary study cohort comprised patient data from January 1, 2019 to December 31, 2019. The total database cohort included unique patients with ET claims from 2015 to 2019 (index identification period comprising 2015–2016, 2017–2018, and 2019 time periods). In addition, estimates of ET diagnoses for the period before 2015 (2013–2014) were back projected on the basis of the decay ratio for the number of patients from the 2017–2018 period to the 2015–2016 period. To account for the transition in the ICD codes from the ninth edition (ICD-9) to the tenth edition (ICD-10) during the study period, adjusted estimates for the number of patients in the 2015–2016 period were calculated using the fraction of patients presenting with a diagnosis code for ET or similar during the transition; estimates were calibrated up using the observed delta increase in patient numbers from the most recent time period through 2017 (i.e., 2017–2019).
US Population Diagnosis Estimates
The number of ET diagnoses was also estimated for the general US population. Based on an assumption that the Compile database captures approximately 60% of the US population [23] and that captured data are representative of the wider population, projected estimates for confirmed ET diagnoses were calculated for the total US population for the year 2019, and longitudinally from 2015 through 2019.
Pre-diagnosis and Post-diagnosis Subsets
Pre-diagnosis and post-diagnosis subsets were defined using data spanning the period from January 1, 2015 to December 31, 2019, to allow exploration of longitudinal patterns of confirmed ET diagnosis, comorbidities, and treatments.
The pre-diagnosis subset comprised patients who had claims data for at least 46 months prior to the first confirmed ET diagnosis in the database. The post-diagnosis subset comprised patients who had claims data for at least 36 months after the initial ET diagnosis.
In both subsets, eligible patients were those who met the criteria, i.e., those who had a claim for an ET diagnosis, prescription, or procedure in at least one quarter of each year. Inclusion in each subset required full enrollment for at least 36 or 46 months, depending on the subset, and thus represented continuous patterns for treatment and comorbidities.
The time to initial ET diagnosis was explored in the pre-diagnosis subset. Data were examined for the presence of the following initial movement disorders prior to diagnosis with ET: cerebral palsy (G80.x), dystonia (G24.02, G24.09, G24.1, G24.2, G24.3, G24.5, G24.8, G24.9), other tremor (G25.1, G25.2, R25.3, R25.8, R25.9), Parkinson’s disease (G20, G21.11, G21.19, G21.2, G21.3, G21.4, G21.8, G21.9), and unspecified tremor (R25.1). These codes represent other tremor-related diagnoses and potential misdiagnoses before the actual diagnosis of ET.
Outcome Measures
Demographic characteristics (age, sex, and primary payer), comorbidities, and treatments were extracted for the primary study cohort with confirmed ET using claims during 2019. For both pre-diagnosis and post-diagnosis subsets, demographic data were extracted relative to the date of the first ET diagnosis claim, while comorbidity and treatment data were extracted in 6-month intervals for at least 46 months before, or 36 months after, the date of initial ET diagnosis, respectively.
Comorbidities
Previous literature and expert opinion informed the selection of comorbidities of interest in patients with ET. The ICD-9 and ICD-10 codes for comorbidities of interest were used for data selection. Movement disorders classified as “other” were defined as a diagnosis for dystonia, other tremor, Parkinson’s disease, and/or unspecified tremor.
Treatment Patterns, Compliance, and Persistence
Previous literature and expert opinion informed search criteria for typical treatments (pharmacologic treatments and procedures) in patients with ET and drug classes used in ET treatment, while national drug codes identified prescribed medications (available upon request). Prescription claims submitted for reimbursement, excluding any reversed or rejected claims (if available), represented data for pharmacologic treatments. The specialties of prescribers were identified using National Provider Identifiers in the Centers for Medicare and Medicaid Services National Plan and Provider Enumeration System [24]. ET-related visits were identified manually by reviewing and classifying relevant events (e.g., tests, diagnoses, visits) for patients with an established diagnosis of ET.
Medication compliance was assessed using the proportion of days (PDC) covered, which represents the ratio of days covered by a dispensed medication to total days in the claim period. Healthcare Common Procedure Coding System and Current Procedural Terminology codes identified specific procedures.
Persistency analysis was applied to prescriptions for ET that were started within 6 months after ET diagnosis. Treatment persistence was defined as the duration between treatment initiation and discontinuation. For each patient, refills were tracked after initiation to determine when medication was discontinued. The numbers of patients who discontinued treatment and who remained on treatment were calculated for each month from treatment initiation. Persistency curves were created for the percentage of patients remaining on their prescribed medication from the time of prescription initiation to discontinuation. Persistency analysis was performed using the SAS Lifetest procedure with censored patients defined [25, 26]; projected mean and median persistency were computed for ET prescription usage among patients who had at least two prescription claims for the same prescription.
Statistical Analyses
Descriptive statistics were used to summarize patient demographics, comorbidities, and treatments. Counts and percentages were calculated for categorical variables, and means and medians were calculated for continuous variables. Projected estimates of ET diagnoses in the US population were calculated assuming the Compile claims database, which has a capture rate of more than 60% [23]. Diagnosis data were projected to 100% (i.e., projected total US ET diagnoses = database-derived ET diagnoses/0.6) for both the 2019 cohort (primary study cohort) and the pre-2015 through 2019 cohort (total database cohort). All patient and claim level analyses were performed using SAS 9.4 (SAS Institute, Cary, NC).
Results
Patient Characteristics
The primary study cohort identified 353,822 patients diagnosed with ET for the year 2019, corresponding to 589,704 projected US diagnoses. Of the 353,822 patients, 128,263 had confirmed ET, corresponding to 213,772 projected US confirmed diagnoses in 2019.
An analysis spanning the period from pre-2015 through 2019 identified a total of 1,336,183 patients with ET, corresponding to 2,226,971 projected US diagnoses. Of the 1,336,183 patients, 459,588 had confirmed ET, corresponding to 765,980 projected US confirmed diagnoses (Table 1).
Of the 128,263 patients in the database with confirmed ET in 2019, approximately 25% received their first ET diagnosis that year, 57% were female, and 75% were aged 65 years or older (Table 2). Medicare provided payer coverage to 78% of patients with confirmed ET in 2019, followed by commercial health plans covering 19% of patients.
Pre-diagnosis and post-diagnosis subsets included 25,039 and 46,169 patients, respectively (Table 2). In the pre-diagnosis subset, the median time to ET diagnosis from initial diagnosis of other movement disorder was 477 days, that from initial diagnosis of other tremor was 441 days, and that from unspecified tremor was 406 days (Table 3).
Comorbidities
In the 2019 cohort of 128,263 patients with confirmed ET, at least one comorbidity of interest was present in 123,161 (96%) patients (Fig. 1). Most comorbidities belonged to cardiometabolic, psychiatric, or movement-related categories. The most common comorbidities consisted of hypertension (73%), hyperlipidemia (68%), depression (44%), diabetes (31%), and anxiety (29%).
In the pre-diagnosis subset (n = 25,039), the number of claims for common cardiometabolic, psychiatric, and movement-related comorbidities continued to increase until ET diagnosis (Fig. 2). Over time, cardiometabolic comorbidities increased by about 10% when assessed from 42 to 48 months before ET diagnosis when compared to the 6 months before diagnosis, with obesity rates more than doubling over this period (8–19%) (Fig. 2A). The percentage of patients with anxiety doubled (10–20%) leading up to ET diagnosis (Fig. 2B). The rate of depression also increased from 31% to 42%, and the percentage of patients with dementia increased from 1% to 5% during the same period. Claims for unspecified tremor were observed in 1% of patients 48 to 42 months before ET diagnosis, increasing to 16% within 6 months of ET diagnosis (Fig. 2C). Similarly, claims for other movement disorders increased markedly, from 6% to 25% over this period.
In the post-diagnosis subset (n = 46,169), the number of claims for movement-related comorbidities decreased, while the number of claims for cardiometabolic and psychiatric comorbidities remained stable from within 6 months before ET diagnosis to 30–36 months after ET diagnosis (Fig. 3A). Claims for depression were present in 34% and 36% of patients during the respective time periods (Fig. 3B). Similarly, claims for anxiety were present in 14% and 17% of patients, respectively, during these periods. The percentage of patients with dementia remained consistent before and after ET diagnosis, increasing from 2% to 5%. Claims for unspecified tremor decreased from 10% to 6% (Fig. 3C), while claims for any other movement disorder remained consistent at about 18% across both periods.
Treatments
From the 2019 cohort with confirmed ET, 4139 (3%) patients underwent a procedural intervention for ET, which primarily comprised botulinum toxin injections (n = 1731; 42%), DBS (n = 2480; 60%), and thalamotomy (n = 350; 8%) (Fig. 4A). Exploration of procedural intervention use in relation to disease course within the post-diagnosis cohort (Fig. 4B) demonstrated low usage (0–1%) in the 12 months before initial diagnosis, followed by a marked increase in the first 6 months after initial ET diagnosis, then remaining relatively stable up to 36 months post diagnosis. The increase in procedural use in the first 6 months post-diagnosis was largely driven by DBS. Notably, thalamotomy use did not appear to change throughout the assessed period; with the percentage of patients opting for this procedure remaining consistently low before and after initial ET diagnosis.
Procedural intervention use in patients with essential tremor (ET). A Percentage of patients with confirmed ET in 2019 with at least 1 procedural intervention by procedure (n = 4139). The sum of percentages is greater than 100% indicating some patients had multiple treatments. B Procedural intervention use over the disease course in the post-diagnosis cohort (n = 46,169) demonstrating the percentage of patients with procedures over the period from 12 months before, and up to 36 months after, initial ET diagnosis (Dx). Procedures included botulinum toxin, deep brain stimulation (DBS), and thalamotomy.
Within the 2019 cohort, 82,323 (64%) patients received at least one prescription, with a total of 1,014,884 prescription claims submitted during this period. The most commonly prescribed agents across all patients with ET (n = 128,263) were propranolol (n = 30,714; 24%), primidone (n = 26,211; 20%), and gabapentin (n = 24,501; 19%) (Fig. 5A, B). About 44,102 (34%) patients received no prescription or procedural intervention for ET. About 97,012 (76%) patients with confirmed ET used concomitant pharmacologic therapies, with 62,521 (49%) patients taking antihypertensives, 53,206 (41%) taking antihyperlipidemics, and 47,121 (37%) taking antidepressants (Fig. 6).
Pharmacologic treatments prescribed to patients with confirmed essential tremor (ET) in 2019. A Percentage of all patients with ET by treatment (n = 128,263). B Percentage of patients with ET who had at least one prescription by treatment (n = 82,323). The sum of percentages is greater than 100% indicating multiple treatment use per patient
Top specialties for prescribing ET medications in 2019 were primary care providers (PCPs) (25%), neurologists (24%), and internal medicine specialists (19%) (Fig. 7A). Non-neurologists, including PCPs and internal medicine specialists, were more likely to prescribe propranolol and other beta-blockers, while neurologists were more likely to prescribe primidone (Fig. 7B). Propranolol comprised 23% of all ET agents prescribed by neurologists and 26% of those prescribed by PCPs, while primidone represented 36% of ET agents prescribed by neurologists and 16% of those prescribed by PCPs. Prescribing patterns were similar among PCPs and internal medicine specialists. Cardiologists were the most likely to prescribe metoprolol, with neurologists the least likely to do so.
In the pre-diagnosis subset (n = 25,039), 8–13% of patients with confirmed ET received propranolol and 6–10% received primidone from 48 months to within 6 months of ET diagnosis, with a slight increase in prescription utilization as the timeline approached ET diagnosis (Fig. 8A, B). In the pre-diagnosis subset, 65% of patients (n = 14,761) visited PCPs or internal medicine specialists in the 6 months before ET diagnosis. Only 11% of patients (n = 2602) visited a neurologist within the same timeframe, while the rest of the patients visited a nurse practitioner, physician assistant, another specialist, or had missing data. On average, an ET diagnosis was established following three visits with a neurologist or 3.2 visits with a PCP or internal medicine specialist. In the post-diagnosis subset (n = 46,169), 17–22% of patients with ET received propranolol and 15–21% received primidone, with a slight decline in prescription utilization as the timeline progressed through 36 months after ET diagnosis (Fig. 8C, D).
Treatment use before and after essential tremor (ET) diagnosis. Percentage of patients with ET using A propranolol and other beta blockers, and B primidone and other anticonvulsants, in the pre-diagnosis subset (n = 25,039). Percentage of patients with ET using C propranolol and other beta blockers, and D primidone and other anticonvulsants in the post-diagnosis subset
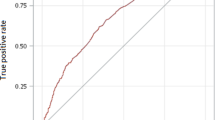
Medication compliance assessed via mean PDC was similar for propranolol (79%) and primidone (80%) (Fig. 9). For both medications, approximately 80% of patients had more than 60% coverage and 44% had coverage between 90% and 100%. For the persistency analysis, eligible patients included 2667 patients receiving propranolol and 2650 patients receiving primidone. The median prescription persistence was 32 months for propranolol and 27 months for primidone. By 2 years of treatment, the discontinuation rate was 40% for propranolol, 47% for primidone, and approximately 40% for all treatments (Fig. 10).
Medication compliance assessed via proportion of days covered (PDC) for propranolol and primidone in the post-diagnosis cohort. Percentages of patients by PDC range and mean PDC are presented. PDC was defined as the ratio of days covered by a dispensed medication to total days in the claim period. ET essential tremor
Discussion
The extent of disease impact on patients with ET remains underappreciated, largely because of a paucity of burden-of-illness data and limited public recognition of the condition. To the best of our knowledge, this is the first published claims-based data examining diagnosis rates, comorbidities, and treatment patterns in patients diagnosed with ET. Our findings from a large US insurance database revealed that approximately 1 million people were diagnosed and actively sought pharmacologic treatment for ET from 2015 through 2019; however, projected US population estimates of approximately 2 million diagnosed and current treatment rates suggest that a further 1 million patients remain untreated. Importantly, these findings signify that ET is underrecognized, underdiagnosed, and misdiagnosed, and that ET diagnosis is complicated by a range of factors, including delayed diagnoses, multiple comorbidities, and treatment adherence limitations, including high discontinuation rates.
Results from our claims-based analysis indicated that a greater percentage of patients diagnosed with ET during the study period were female (approx. 60%) and most were 65 years of age and older (75%). While our sex-related findings may reflect differential care-seeking behaviors, with female patients more likely to seek care for their ET, data pertaining to sex differences in ET have been inconsistent to date. A recent meta-analysis concluded that ET prevalence was higher among men, while another meta-analysis found that prevalence was independent of sex [14, 27]. Our age-related findings are consistent with established reports of ET primarily being diagnosed in older patients and of age-related increases in global and US prevalence estimates [5, 14, 27]. Of note, these relationships may reflect delayed diagnoses rather than underlying age-related pathology or circuit disturbances. In our study, a confirmed diagnosis for ET was reached 18 months, on average, after the initial diagnosis of a different movement disorder. In 2018, the Task Force on Tremor of the International Parkinson and Movement Disorder Society (MDS) updated the definitions of ET and proposed establishing an ET diagnosis only after a 3-year history of tremor [3], with tremor symptoms lasting less than 3 years to be classified as indeterminate tremor. Given the inherent difficulty in obtaining claims-based data at the first signs of tremor, the amount of time patients experienced tremor symptoms remains unknown. Nonetheless, our findings indicate that many patients are frequently diagnosed with another movement disorder before being diagnosed as having ET (31% with unspecified tremor, 8% with other tremor, 7% with Parkinson’s disease, and 1% with dystonia), with ET diagnosis established approximately 1.4–1.8 years after the earlier diagnosis.
Almost all patients with ET had at least one comorbidity, with cardiovascular (e.g., hypertension, hyperlipidemia), metabolic (e.g., diabetes, obesity), and psychiatric-related (e.g., depression, anxiety) conditions comprising the most common comorbidities, consistent with other claims analyses [28]. Although this analysis found similar rates of cardiovascular and metabolic comorbidities in patients with ET as in the general population over the age of 60, rates of depression and anxiety were double those in the general population over the age of 65 [29,30,31,32,33]. Other studies have postulated that ET has a substantial psychological component, with several reporting higher levels of depression and anxiety in affected patients [34,35,36,37]. For example, a recent cross-sectional study from investigators in China reported that 63% of patients with ET had at least mild anxiety, and 54% had at least mild depression [33]. Moreover, more severe depressive symptoms have been found to contribute to medication nonadherence in patients with ET [36]. The importance of the psychosocial impact on patients with ET is further highlighted by previous reports of almost one in three patients with ET expressing a desire for access to psychological services and support, as a result of concomitant depression and/or anxiety [37]. Dementia is another comorbidity that has been previously explored in studies of patients with ET. While the rate of dementia in the current claims analysis remained around 5% after ET diagnosis, previous studies report rates of up to 25% [38, 39]. In one study, the prevalence of dementia was elevated in patients with ET who were 65 years and older compared with the general population in the same age range [39]. Moreover, findings from a longitudinal perspective analysis have demonstrated an association between higher severity of both dementia and depression, and increased risk of mortality among older patients with ET [40]. Together with previous reports, our findings, therefore, highlight both the frequency and complexity of comorbidities and their associated impact on patients with ET.
Our data revealed that approximately two in three patients diagnosed with ET received a prescription for ET treatment in 2019. The two most commonly prescribed medications included propranolol and primidone, consistent with reports of their use as first-line medications for ET [41]. Studies report that anywhere between 29% and 53% of patients use propranolol, and 18–46% use primidone [28, 42, 43]. In line with these ranges, findings from the current claims analysis indicate that one in four patients used propranolol and one in five used primidone after ET diagnosis. Our findings are also consistent with current treatment recommendations, with the Task Force on Tremor and Evidence Based Medicine Committee at the MDS recommending propranolol and primidone as efficacious treatments for ET, especially for managing upper limb tremor [1]. In the current study, approximately three in four patients with ET were using at least two pharmacologic treatments in 2019. Notably, about half of all patients were taking antihypertensives. The use of concomitant medications may be especially problematic in patients taking propranolol for ET because the medication has multiple potential drug interactions [17]. Furthermore, MDS recommendations state that some adverse events of primidone (e.g., malaise, dizziness, unsteadiness) may lead to treatment discontinuation [1]. Our finding of 3% of patients with ET receiving a procedural intervention is consistent with recent reports [28, 43]. Additionally, the most common interventions—botulinum toxin injections, DBS, and thalamotomy—are also in line with MDS guidance regarding their potential usefulness for ET [1]. Notably, our findings indicated that procedural intervention use was relatively low prior to initial ET diagnosis. On the basis of demographic data demonstrating that 75% of patients were at least 65 years of age, it is reasonable to infer that for most patients who opt for procedural interventions, usage occurs around age 65 years or older, consistent with published work reporting mean ages of approximately 60–70 years for patients undergoing DBS [44,45,46,47].
With respect to treatment adherence, the current study revealed 2-year discontinuation rates of 40% and 47% for propranolol and primidone, respectively, with approximately 40% of patients discontinuing all treatments at 2 years, approximating to 200,000 discontinuations per year based on current treatment rates. Among patients taking primidone or propranolol, about 40% used it daily as prescribed. On average, patients adhered to prescribed primidone or propranolol about 4 out of 5 days, or they missed treatment for about 6 days in a month. These findings are consistent with those from a medication adherence study [42] in which 33% of patients with ET reported they sometimes forgot to take their medications, 21% reported missing doses within the past week, and about 25% did not take their medication for whole days in the previous 2 weeks. In that study, younger age, depressive symptoms, and less severe tremor were contributing factors to nonadherence. While we were unable to assess factors associated with treatment discontinuations in our study, future analyses will be important to determine the relative contributions of age, comorbidities, and disease severity to treatment compliance. Our longitudinal findings are further in line with previous reports of decreasing adherence in ET with time. In a large retrospective analysis of specialist outpatient clinic visits from 2001 to 2018, 22% of patients with a prescription record for ET treatment reported a lack of response, with 12% eventually discontinuing treatment—primarily propranolol or primidone—because of side effects [43]. In another study capturing treatment patterns over a 5-year period, anywhere from one half to two thirds of patients taking primidone or propranolol eventually discontinued the treatment because of lack of efficacy, negative side effects, or both, with a median discontinuation rate of 63% [48]. In further corroboration, a systematic review and meta-analysis of 31 studies and a small, prospective study involving 50 participants found that 30–50% of patients did not respond to propranolol or primidone as first-line agents, with some tolerance to drug effect observed with chronic use [41, 49]. Importantly, treatment adherence in ET depends on various factors, with medication side effects and lack of efficacy remaining the key reasons for treatment discontinuation [43, 48].
In the current study, prescribing patterns varied markedly by specialty. PCPs, neurologists, and internal medicine specialists were the top three specialties prescribing ET medications. Two thirds of patients seen by a PCP or internal medicine specialist were referred to another specialist before diagnosis, with 46% of patients eventually receiving a diagnosis from a PCP. Notably, neurologists diagnosed three out of ten ET cases, with only 11% of neurologist visits occurring in the 6 months prior to a confirmed ET diagnosis. In line with this, PCPs and internal medicine specialists were more likely to prescribe propranolol as first-line therapy for ET. In contrast, neurologists prescribed primidone more frequently than propranolol, likely corresponding to the increased likelihood of patients with severe ET symptoms to receive care from neurologists and to the consequent use of primidone as a second-line therapy after initial prescription by the PCP. The observed frequent prescribing of metoprolol by cardiologists likely reflects prescribing patterns for cardiovascular comorbidities associated with ET rather than ET itself and is further supported by the finding that neurologists were least likely to prescribe metoprolol. More generally, our findings revealed distinct prescribing patterns among neurologists and non-neurologists, with the latter more often prescribing beta-blockers despite limited efficacy and poor tolerability in some patients [1, 18, 50]. The observed differences in prescribing patterns among specialists may also suggest a need for increased awareness among providers about management pathways in ET. Indeed, patient survey data previously revealed that almost one in three patients expressed concern that their physician was not moderately well educated about ETs [37]. Moreover, 91% of surveyed patients considered access to neurologists specializing in movement disorders as essential to their care. Of note, a survey of medication usage patterns revealed that neurologists specializing in movement disorders were almost twice as likely to prescribe primidone or propranolol for ET compared with general neurologists [48]. Finally, our findings highlight the need to improve treatment adherence and ultimately minimize patient burden in ET. Given that treatment adherence is typically related to poor tolerability and limited efficacy [20], our findings point to the need for targeted therapies with novel mechanisms of action capable of mitigating concerns of existing treatments for ET.
Limitations
Despite our study’s strengths, including a large sample size and the analysis of real-world patterns for ET diagnoses, comorbidities, and treatments, it is important to note its limitations, including those inherent to claims-based analyses. The study was retrospective and relied on claims data, which may contain coding errors and have missing data. Administrative delays (e.g., delays in submitting claims) may have impacted observed times to ET diagnosis, and incorrect diagnosis coding could have led to data misclassifications. Eligibility criteria for confirmed ET required ET diagnosis with two relevant prescriptions or an additional diagnosis for unspecified tremor, which may have limited the number of identified patients with ET. Although stricter eligibility criteria attempted to ensure the presence of ET diagnosis and avoid potential misclassifications, the criteria most likely resulted in an underestimation of the number of patients with ET compared to established prevalence estimates [4, 5]. Additionally, because the database only captured data from 2015 to 2019, it is possible that some patients in the post-diagnosis subset received their initial ET diagnosis outside the study period. The database also only captured patients who were actively seeking a diagnosis or treatment for their tremor, which may have excluded patients with mild tremor or those who discontinued all treatments prior to the study period as a result of poor efficacy or tolerability. These factors, alongside low disease awareness, potentially further contributed to projected diagnosis estimates being lower than previously reported figures. Other limitations specific to claims analyses include the inability to capture all patients in a population and all claims for a given patient, limited insights into adjudicated claims, as well as the possible presence of nonunique patients in cases where patients switch coverage plans which may have also contributed to overrepresentation of treatment discontinuation rates. In addition, prescription claims did not include associated ICD-10 codes, thus medications may have been prescribed for other conditions outside ET. Prescription utilization rates could have been overrepresented because of the requirement for two relevant ET prescriptions as part of identifying confirmed ET diagnoses. Finally, medications for ET could have been started before the official diagnosis of ET and may have been prescribed for comorbid conditions and not necessarily for ET.
Conclusions
This large study based on comprehensive claims analysis highlights the complexity of ET diagnoses and the high number of untreated patients, alongside disease comorbidity and medication adherence challenges among treated patients. Consistent with prior reports, our findings indicate an age-related increase in ET diagnoses, with a large portion of patients diagnosed after the age of 65 years. Notably, confirmed ET diagnosis was established about 1.5 years after the diagnosis of an initial movement disorder. Almost all patients suffered from at least one comorbid condition, with cardiometabolic and psychiatric-related comorbidities increasing until ET diagnosis. Additionally, our findings revealed that, in general, older patients with ET suffer from anxiety or depression at double the rate compared with the older general population. About two in three patients received pharmacologic treatment for ET, primarily propranolol or primidone, but 2-year discontinuation rates were over 40% for both medications. Additionally, concomitant medication use was high, with likely implications for ET medication drug-interaction risks. In addition to providing novel insights into the complexity of care for patients with ET, this study highlights an opportunity to redefine early disease characteristics to aid in more effective diagnoses. This is critical to facilitate the development of targeted treatments that exhibit better efficacy and tolerability, and a favorable profile with respect to drug–drug interactions while maximizing treatment adherence potential for patients with ET.
References
Ferreira JJ, Mestre TA, Lyons KE, et al. MDS evidence-based review of treatments for essential tremor. Mov Disord. 2019;34:950–8. https://doi.org/10.1002/mds.27700.
Zesiewicz TA, Elble RJ, Louis ED, et al. Evidence-based guideline update: treatment of essential tremor: report of the quality standards subcommittee of the American Academy of Neurology. Neurology. 2011;77:1752–5. https://doi.org/10.1212/WNL.0b013e318236f0fd.
Bhatia KP, Bain P, Bajaj N, et al. Consensus statement on the classification of tremors. From the task force on tremor of the International Parkinson and Movement Disorder Society. Mov Disord. 2018;33:75–87. https://doi.org/10.1002/mds.27121.
Louis ED, Ottman R. How many people in the USA have essential tremor? Deriving a population estimate based on epidemiological data. Tremor Other Hyperkinet Mov (N Y). 2014;4:259. https://doi.org/10.7916/d8tt4p4b.
Crawford S, Lally C, Petrillo J, Paskavitz J, Louis E. How many adults in the US have essential tremor? Using data from epidemiological studies to derive age-specific estimates of prevalence (4458). Neurology. 2020;94:4458.
Louis ED, Barnes L, Albert SM, et al. Correlates of functional disability in essential tremor. Mov Disord. 2001;16:914–20. https://doi.org/10.1002/mds.1184.
Amlang CJ, Trujillo Diaz D, Louis ED. Essential tremor as a “waste basket” diagnosis: diagnosing essential tremor remains a challenge. Front Neurol. 2020;11:172. https://doi.org/10.3389/fneur.2020.00172.
Jain S, Lo SE, Louis ED. Common misdiagnosis of a common neurological disorder: how are we misdiagnosing essential tremor? Arch Neurol. 2006;63:1100–4. https://doi.org/10.1001/archneur.63.8.1100.
Elble RJ. What is essential tremor? Curr Neurol Neurosci Rep. 2013;13:353. https://doi.org/10.1007/s11910-013-0353-4.
Elble RJ. Essential tremor is a useful concept? No. Mov Disord Clin Pract. 2017;4:663–5. https://doi.org/10.1002/mdc3.12514.
Deuschl G. Essential tremor is a useful concept: yes. Mov Disord Clin Pract. 2017;4:666–8. https://doi.org/10.1002/mdc3.12515.
Thanvi B, Lo N, Robinson T. Essential tremor—the most common movement disorder in older people. Age Ageing. 2006;35:344–9. https://doi.org/10.1093/ageing/afj072.
Shalaby S, Indes J, Keung B, et al. Public knowledge and attitude toward essential tremor: a questionnaire survey. Front Neurol. 2016;7:60. https://doi.org/10.3389/fneur.2016.00060.
Louis ED, McCreary M. How common is essential tremor? Update on the worldwide prevalence of essential tremor. Tremor Other Hyperkinet Mov (N Y). 2021;11:28. https://doi.org/10.5334/tohm.632.
Louis ED, Factor-Litvak P. Screening for and estimating the prevalence of essential tremor: a random-digit dialing-based study in the New York metropolitan area. Neuroepidemiology. 2016;46:51–6. https://doi.org/10.1159/000442576.
Dogu O, Louis ED, Sevim S, Kaleagasi H, Aral M. Clinical characteristics of essential tremor in Mersin, Turkey—a population-based door-to-door study. J Neurol. 2005;252:570–4. https://doi.org/10.1007/s00415-005-0700-8.
Inderal. Package Insert. Wyeth Pharmaceuticals. 2010.
Sepúlveda Soto MC, Fasano A. Essential tremor: new advances. Clin Park Relat Disord. 2020;3: 100031. https://doi.org/10.1016/j.prdoa.2019.100031.
Alonso-Navarro H, García-Martín E, Agúndez JAG, Jiménez-Jiménez FJ. Current and future neuropharmacological options for the treatment of essential tremor. Curr Neuropharmacol. 2020;18(6):518–37. https://doi.org/10.2174/1570159X18666200124145743.
Louis ED, Rios E, Henchcliffe C. How are we doing with the treatment of essential tremor (ET)? Persistence of patients with ET on medication: data from 528 patients in three settings. Eur J Neurol. 2010;17:882–4. https://doi.org/10.1111/j.1468-1331.2009.02926.x.
Sharma S, Pandey S. Treatment of essential tremor: current status. Postgrad Med J. 2020;96:84–93. https://doi.org/10.1136/postgradmedj-2019-136647.
Haubenberger D, Hallett M. Essential tremor. N Engl J Med. 2018;378:1802–10. https://doi.org/10.1056/NEJMcp1707928.
Database. Compile Health. https://www.compile.com/data/smart-data. Accessed 8 July 2022.
National Plan and Provider Enumeration System NPPES National Provider Identifier NPI Registry. U.S. Centers for Medicare and Medicaid Services. https://npiregistry.cms.hhs.gov/. Accessed 8 July 2022.
Kohfeld WF, Ying S. Creating and customizing the Kaplan–Meier survival plot in PROC LIFETEST. Paper presented at the SAS Global Forum 2013, San Francisco, CA, 28 April–1 May 2013. https://support.sas.com/resources/papers/proceedings13/427-2013.pdf. Accessed 5 July 2022.
The LIFETEST Procedure. SAS Help Center. SAS Institute. https://documentation.sas.com/doc/en/statug/15.2/statug_lifetest_toc.htm. Updated 28 October 2020. Accessed 8 July 2022.
Song P, Zhang Y, Zha M, et al. The global prevalence of essential tremor, with emphasis on age and sex: a meta-analysis. J Glob Health. 2021;11:04028. https://doi.org/10.7189/jogh.11.04028.
Broderick K, Gerbasi M, Petrillo Billet J, et al. PND74 the high burden of comorbidities and treatment changes among adults with essential tremor in a real-world setting. Value Health. 2020;23:S273. https://doi.org/10.1016/j.jval.2020.04.966.
Ostchega Y, Fryar CD, Nwankwo T, Nguyen DT. Hypertension prevalence among adults aged 18 and over: United States, 2017–2018. NCHS Data Brief 2020;1–8.
Cho SMJ, Lee HJ, Shim JS, Song BM, Kim HC. Associations between age and dyslipidemia are differed by education level: the Cardiovascular and Metabolic Diseases Etiology Research Center (CMERC) cohort. Lipids Health Dis. 2020;19:12. https://doi.org/10.1186/s12944-020-1189-y.
Villarroel MA, Terlizzi EP. Symptoms of depression among adults: United States, 2019. NCHS Data Brief 2020;1–8.
Terlizzi EP, Villarroel MA. Symptoms of generalized anxiety disorder among adults: United States, 2019. NCHS Data Brief 2020;1–8.
National Diabetes Statistics Report 2020: estimates of diabetes and its burden in the United States. U.S. Department of Health and Human Services Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf. Accessed 6 October 2021.
Sengul Y, Sengul HS, Yucekaya SK, et al. Cognitive functions, fatigue, depression, anxiety, and sleep disturbances: assessment of nonmotor features in young patients with essential tremor. Acta Neurol Belg. 2015;115:281–7. https://doi.org/10.1007/s13760-014-0396-6.
Huang H, Yang X, Zhao Q, et al. Prevalence and risk factors of depression and anxiety in essential tremor patients: a cross-sectional study in Southwest China. Front Neurol. 2019;10:1194. https://doi.org/10.3389/fneur.2019.01194.
Louis ED, Huey ED, Gerbin M, Viner AS. Depressive traits in essential tremor: impact on disability, quality of life, and medication adherence. Eur J Neurol. 2012;19:1349–54. https://doi.org/10.1111/j.1468-1331.2012.03774.x.
Louis ED, Rohl B, Rice C. Defining the treatment gap: what essential tremor patients want that they are not getting. Tremor Other Hyperkinet Mov (N Y). 2015;5:331. https://doi.org/10.7916/d87080m9.
Thawani SP, Schupf N, Louis ED. Essential tremor is associated with dementia: prospective population-based study in New York. Neurology. 2009;73:621–5. https://doi.org/10.1212/WNL.0b013e3181b389f1.
Benito-León J, Louis ED, Bermejo-Pareja F. Elderly-onset essential tremor is associated with dementia. Neurology. 2006;66:1500–5. https://doi.org/10.1212/01.wnl.0000216134.88617.de.
Zubair A, Cersonsky TEK, Kellner S, Huey ED, Cosentino S, Louis ED. What predicts mortality in essential tremor? A prospective, longitudinal study of elders. Front Neurol. 2018;9:1077. https://doi.org/10.3389/fneur.2018.01077.
Yunusa I, Abraham P, Alsumali A, Eguale T. Prevalence, disease burden and unmet needs of patients with essential tremor: a systematic review and meta-analysis. Value Health. 2018;21:S204–5. https://doi.org/10.1016/j.jval.2018.04.1390.
Louis ED. Medication non-adherence in essential tremor. Parkinsonism Relat Disord. 2015;21:138–41. https://doi.org/10.1016/j.parkreldis.2014.12.001.
Shah C, Jackson GR, Sarwar AI, Mandava P, Jamal F. Treatment patterns in essential tremor: a retrospective analysis. Tremor Other Hyperkinet Mov (NY). 2022;12:10. https://doi.org/10.5334/tohm.682.
Giordano M, Caccavella VM, Zaed I, et al. Comparison between deep brain stimulation and magnetic resonance-guided focused ultrasound in the treatment of essential tremor: a systematic review and pooled analysis of functional outcomes. J Neurol Neurosurg Psychiatry. 2020;91(12):1270–8. https://doi.org/10.1136/jnnp-2020-323216.
Huss DS, Dallapiazza RF, Shah BB, Harrison MB, Diamond J, Elias WJ. Functional assessment and quality of life in essential tremor with bilateral or unilateral DBS and focused ultrasound thalamotomy. Mov Disord. 2015;30(14):1937–43. https://doi.org/10.1002/mds.26455.
Niemann N, Jankovic J. Botulinum toxin for the treatment of hand tremor. Toxins (Basel). 2018;10(7):299. https://doi.org/10.3390/toxins10070299.
Verla T, Marky A, Farber H, et al. Impact of advancing age on post-operative complications of deep brain stimulation surgery for essential tremor. J Clin Neurosci. 2015;22:872–6. https://doi.org/10.1016/j.jocn.2014.11.005.
Diaz NL, Louis ED. Survey of medication usage patterns among essential tremor patients: movement disorder specialists vs. general neurologists. Parkinsonism Relat Disord. 2010;16:604–7. https://doi.org/10.1016/j.parkreldis.2010.07.011.
Koller WC, Vetere-Overfield B. Acute and chronic effects of propranolol and primidone in essential tremor. Neurology. 1989;39:1587–8. https://doi.org/10.1212/wnl.39.12.1587.
Hedera P, Cibulčík F, Davis TL. Pharmacotherapy of essential tremor. J Cent Nerv Syst Dis. 2013;5:43–55. https://doi.org/10.4137/jcnsd.S6561.
Acknowledgements
Funding
All work for this study, including the journal’s Rapid Service and Open Access fees, was funded by Praxis Precision Medicines, Boston, MA, USA.
Medical Writing, Editorial, and Other Assistance
We thank Charles River Associates for their assistance with data collection and analysis, and Janna Afanasjeva, PharmD, and Alyssa Theodore, PhD, of Simpson Healthcare for assistance in preparing the manuscript. These activities were funded by Praxis Precision Medicines, Boston, MA, USA.
Author Contributions
Conceptualization: Christine Vetterick, Robert Pendal, Bernard Ravina; Interpretation: Christine Vetterick, Kelly E. Lyons, Lillian G. Matthews, Robert Pendal, Bernard Ravina; Visualization: Christine Vetterick, Lillian G. Matthews, Robert Pendal; Writing- review and editing: Christine Vetterick, Kelly E. Lyons, Lillian G. Matthews, Robert Pendal, Bernard Ravina. All authors read and approved the final manuscript.
Disclosures
Christine Vetterick and Robert Pendal are current employees of Praxis Precision Medicines and are Praxis shareholders. Kelly E. Lyons serves as a consultant for Abbott, Jazz, Praxis, and Sage, and is the president of the International Essential Tremor Foundation. Lillian G. Matthews serves as a paid consultant to Praxis Precision Medicines and is a Praxis shareholder. Bernard Ravina was an employee of Praxis Precision Medicines during study conduct and manuscript preparation, serves as a paid strategic advisor to Praxis Precision Medicines, and is a Praxis shareholder.
Compliance with Ethics Guidelines
Analyses in the current study included only deidentified data; thus, institutional review board approval was not required. Data were used with permission and under license from Compile Health.
Data Availability
The datasets generated during and/or analyzed during the current study are not publicly available as restrictions apply to the availability of these data, which were used with permission and under license for this study from Compile Health. Derived data supporting the findings of this study are available upon reasonable request from the corresponding author.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Vetterick, C., Lyons, K.E., Matthews, L.G. et al. The Hidden Burden of Disease and Treatment Experiences of Patients with Essential Tremor: A Retrospective Claims Data Analysis. Adv Ther 39, 5546–5567 (2022). https://doi.org/10.1007/s12325-022-02318-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02318-8