Abstract
Purpose
To evaluate the long-term cost-effectiveness of transferring type 2 diabetes patients to an insulin detemir regimen after failure to achieve adequate control with oral antidiabetic agents (OADs) alone, or in combination with neutral protamine hagedorn (NPH) insulin, or with insulin glargine in Germany.
Methods
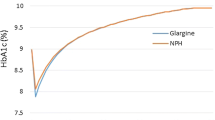
A computer simulation model of diabetes was used to make long-term projections of future clinical outcomes and direct medical costs based on findings from a German subanalysis of the PREDICTIVE trial. The study analysed the impact of converting patients failing their current treatments to an insulin detemir regimen. Therapy conversion to insulin detemir ± OADs was associated with a significant reduction in glycosylated haemoglobin (HbA1c) compared with OADs alone, NPH insulin ± OADs, and insulin glargine ± OADs. Across all three groups, hypoglycaemia rates decreased by 80% and patients lost an average of 0.9 kg of body weight during treatment with insulin detemir ± OADs.
Results
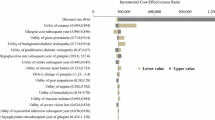
Therapy conversion to insulin detemir ± OADs was projected to improve life expectancy by 0.28 years compared with OADs alone, and by 0.13 years compared with the NPH and glargine regimens. Transfer to insulin detemir was associated with improvements in quality-adjusted life expectancy of 0.21 quality-adjusted life years (QALYs) over OADs alone, 0.28 QALYs over NPH ± OADs, and 0.29 QALYs over glargine ± OADs. Insulin detemir was associated with savings over patient lifetimes due to reduced diabetes-related complications in all three comparisons.
Conclusions
Therapy conversion to insulin detemir ± OADs in type 2 diabetes patients failing OADs alone, NPH or insulin glargine regimens was associated with improvements in life expectancy, quality-adjusted life expectancy and cost savings in all three scenarios evaluated.
Similar content being viewed by others
References
Liebl A. Costs involved in the early and late phases of diabetes mellitus [in German]. Internist (Berl). 2007;48:708–714.
Liebl A, Spannheimer A, Reitberger U, Gortz A. Costs of long-term complications in type 2 diabetes patients in Germany. Results of the CODE-2 study [in German]. Med Klin (Munich). 2002;97:713–719.
Koster I, Hauner H, von FL. Heterogeneity of costs of diabetic patients: the Cost of Diabetes Mellitus study [in German]. Dtsch Med Wochenschr. 2006;131:804–810.
The UK Prospective Diabetes Study Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352:837–853.
The UK Prospective Diabetes Study Group. Effect of intensive blood glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet. 1998;352:854–865.
Stratton IM, Adler AI, Neil HA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321:405–412.
Schneider CA, Herold G, Gysan D, Albus C, Bjarnason-Wehrens B, Predel HG. Prevalence of cardiovascular risk factors in middle-aged type 2 diabetic automobile employees assessed at the workplace — the Praeford study. J Occup Environ Med. 2007;49:481–483.
Pittrow D, Stalla GK, Zeiher AM, et al. Prevalence, drug treatment and metabolic control of diabetes mellitus in primary care [in German]. Med Klin (Munich). 2006;101:635–644.
Yurgin N, Secnik K, Lage MJ. Antidiabetic prescriptions and glycemic control in German patients with type 2 diabetes mellitus: a retrospective database study. Clin Ther. 2007;29:316–325.
Philis-Tsimikas A, Charpentier G, Clauson P, Ravn GM, Roberts VL, Thorsteinsson B. Comparison of once-daily insulin detemir with NPH insulin added to a regimen of oral antidiabetic drugs in poorly controlled type 2 diabetes. Clin Ther. 2006;28:1569–1581.
Abraham C, Priest L. Crisis in cataract surgery epitomizes waiting-list woes. Globe and Mail. 11 September 2004.
Hermansen K, Davies M, Derezinski T, Martinez RG, Clauson P, Home P. A 26-week, randomized, parallel, treat-totarget trial comparing insulin detemir with NPH insulin as add-on therapy to oral glucose-lowering drugs in insulin-naive people with type 2 diabetes. Diabetes Care. 2006;29:1269–1274.
Meneghini LF, Rosenberg KH, Koenen C, Merilainen MJ, Luddeke HJ. Insulin detemir improves glycaemic control with less hypoglycaemia and no weight gain in patients with type 2 diabetes who were insulin naive or treated with NPH or insulin glargine: clinical practice experience from a German subgroup of the PREDICTIVE study. Diabetes Obes Metab. 2007;9:418–427.
Palmer AJ, Roze S, Valentine WJ, et al. The CORE diabetes model: projecting longterm clinical outcomes, costs and costeffectiveness of interventions in diabetes mellitus (types 1 and 2) to support clinical and reimbursement decision-making. Curr Med Res Opin. 2004;20(8 suppl):5–26.
Palmer AJ, Roze S, Valentine W, et al. Validation of the CORE diabetes model against epidemiological and clinical studies. Curr Med Res Opin. 2004;20(suppl 1):S27–S40.
Liebl A, Mata M, Eschwege E. Evaluation of risk factors for development of complications in type II diabetes in Europe. Diabetologia. 2002;45:S23–S28.
Liebl A, Neiss A, Spannheimer A, et al. Complications, co-morbidity, and blood glucose control in type 2 diabetes mellitus patients in Germany-results from the CODE-2 study. Exp Clin Endocrinol Diabetes. 2002;110:10–16.
Koster I, von FL, Ihle P, Schubert I, Hauner H. The cost burden of diabetes mellitus: the evidence from Germany-the CoDiM study. Diabetologia. 2006;49:1498–1504.
Neeser K, Lubben G, Siebert U, Schramm W. Cost effectiveness of combination therapy with pioglitazone for type 2 diabetes mellitus from a German statutory healthcare perspective. Pharmacoeconomics. 2004;22:321–341.
Banz K, Dinkel R, Hanefeld M, Schwanebeck U. Evaluation of the potential clinical and economic effects of bodyweight stabilisation with acarbose in patients with type 2 diabetes mellitus. A decisionanalytical approach. Pharmacoeconomics. 1998;13:449–459.
Szucs TD, Smala A, Fischer T. Costs of intensive insulin therapy in type 1 diabetes mellitus: experiences from the DCCT study [in German]. Fortschr Med. 1998;116:34–38.
Statistisches Bundesamt Deutschland. Preisindizes für die Lebenshaltung. Gesundheitsbericht fur Deutschland. Statistisches Bundesamt Deutschland 19982005 (7.8) (Stuttgart: Metzler Poeschel; 1998:410–413). Available at: www. statistisches-bundesamt.de
Krankenhausdiagnosestatistik: diagnosedaten der krankenhauspatienten von 1997. Wiesbaden: Statistisches Bundesamt Deutchland; 1999.
Palmer AJ, Annemans L, Roze S, Lamotte M, Rodby RA, Ritz E. Health economic consequences of the use of irbesartan in patients in Germany with type 2 diabetes, nephropathy and hypertension [in German]. Dtsch Med Wochenschr. 2004;129:13–18.
Reduced costs with bisoprolol treatment for heart failure: an economic analysis of the second Cardiac Insufficiency Bisoprolol Study (CIBIS-II). Eur Heart J. 2001;22:1021–1031.
Rychlik R, Pfiel T, Daniel D, Habs M, Klapper H. Socioeconomic relevance of treatment of chronic heart failure stage NYHA 2 with crataegus extract WS 1442 — a prospective 3-year pharmacoeconomic study. Value Health. 2004;7:695.
Laaser U, Breckenkamp J, Niermann U. Cost-effectiveness analysis of medical interventions in patients with stroke in Germany under special consideration of “stroke units”. Gesundh Okon Qual Manag. 1999;4:176–183.
Statistisches Bundesamt Deutschland. Preisindizes für die Lebenshaltung. Gesundheitsbericht fur Deutschland. Statistisches Bundesamt Deutschland 20051998 (5.23) (Stuttgart: Metzler Poeschel; 1998:254–258). Available at: www.statistisches-bundesamt.de
Schadlich PK, Brecht JG, Brunetti M, Pagano E, Rangoonwala B, Huppertz E. Cost effectiveness of ramipril in patients with non-diabetic nephropathy and hypertension: economic evaluation of Ramipril Efficacy In Nephropathy (REIN) study for Germany from the perspective of statutory health insurance. Pharmacoeconomics. 2001;19:497–512.
Köhler A. Kölner Kommentar zum EBM 2002. Kölné: Deutscher Ärzte-Verlag; 2001.
Kelm-Kahl I, Ohrloff C. Minimal invasive chirurgie beim grauen star: was zahlt die kassee — medizin and gesdunheit [1.10.2001]; 2001. Available at: http://www3.lifeline.de/yavivo/
Ghatnekar O. Cost-effectiveness of treating deep diabetic foot ulcers with Promogran in four different European countries. J Wound Care. 2002;11:70.
Dahmen HG. Diabetic foot syndrome and its risks: amputation, handicap, high-cost sequelae [in German]. Gesundheitswesen. 1997;59:566–568.
Tarn T, Smith M. Pharmacoeconomic guidelines around the world. ISPOR Connections. 2004;10:5–15.
Briggs AH, Wonderling DE, Mooney CZ. Pulling cost-effectiveness analysis up by its bootstraps: a non-parametric approach to confidence interval estimation. Health Econ. 1997;6:327–340.
Haak T, Tiengo A, Draeger E, Suntum M, Waldhausl W. Lower within-subject variability of fasting blood glucose and reduced weight gain with insulin detemir compared to NPH insulin in patients with type 2 diabetes. Diabetes Obes Metab. 2005;7:56–64.
Raslova K, Bogoev M, Raz I, Leth G, Gall MA, Hancu N. Insulin detemir and insulin aspart: a promising basal-bolus regimen for type 2 diabetes. Diab Res Clin Pract. 2004;66:193–201.
Pieber TR, Treichel HC, Hompesch B, et al. Comparison of insulin detemir and insulin glargine in subjects with type 1 diabetes using intensive insulin therapy. Diabet Med. 2007;24:635–642.
Heise T, Nosek L, Ronn BB, et al. Lower within-subject variability of insulin detemir in comparison to NPH insulin and insulin glargine in people with type 1 diabetes. Diabetes. 2004;53:1614–1620.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Valentine, W.J., Goodall, G., Aagren, M. et al. Evaluating the cost-effectiveness of therapy conversion to insulin detemir in patients with type 2 diabetes in Germany: a modelling study of long-term clinical and cost outcomes. Adv Therapy 25, 567–584 (2008). https://doi.org/10.1007/s12325-008-0069-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-008-0069-z