Abstract
Introduction
The purpose of this study was to retrospectively evaluate the effect of the Dynasplint® Trismus System (DTS; Dynasplint Systems Inc, Severna Park, Md, USA) for patients who were recently diagnosed with trismus following radiation therapy, dental treatment, oral surgery, or following a neural pathology such as a stroke.
Methods
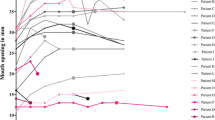
We reviewed 48 patient histories (treated in 2006–2007), and divided into 4 cohort groups (radiation therapy for head/neck cancer, dental treatment, oral surgery, or stroke), to measure the efficacy of this treatment’s modality. Patients were prescribed the DTS after diagnosis of trismus based on examination that showed <40 mm maximal interincisal distance. The DTS uses low-load, prolonged-duration stretch with replicable, dynamic tension to achieve longer time at end range (of motion). Each patient used this device for 20–30 min, 3 times per d.
Results
This cohort case series showed that there was a statistically significant difference within all patient groups (P<0.0001; t=10.3289), but there was not a significant difference between groups (P=0.374).
Conclusion
The biomechanical modality of DTS with a low-load, prolonged-duration stretch was attributed to the success in reducing contracture in this study. This improved range of motion, allowing patients to regain the eating, hygiene and speaking patterns they had before developing trismus.
Similar content being viewed by others
References
Dhanrajani PJ, Jonaidel O. Trismus: aetiology, differential diagnosis and treatment. Dent Update. 2002;29:88–92, 94.
Dijkstra PU, Kalk WW, Roodenburg JL. Trismus in head and neck oncology: a systematic review. Oral Oncol. 2004;40:879–889.
Moore PA, Brar P, Smiga ER, Costello BJ. Preemptive rofecoxib and dexamethasone for prevention of pain and trismus following third molar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:E1–E7.
Goldstein M, Maxymiw WG, Cummings BJ, Wood RE. The effects of antitumor irradiation on mandibular opening and mobility: a prospective study of 58 patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:365–373.
Brunello DL, Mandikos MN. The use of a dynamic opening device in the treatment of radiation induced trismus. Aust Prosthodont J. 1995;9:45–48.
Dijkstra PU, Huisman PM, Roodenburg JL. Criteria for trismus in head and neck oncology. Int J Oral Maxillofac Surg. 2006;35:337–342.
Jansma J, Vissink A, Spijkervet FK, et al. Protocol for the prevention and treatment of oral sequelae resulting from head and neck radiation therapy. Cancer. 1992;70:2171–2180.
Silverman S. Oral Cancer. 4th ed. Ontario, Canada: BC Decker; 1997.
Wang CJ, Huang EY, Hsu HC, Chen HC, Fang FM, Hsiung CY. The degree and time-course assessment of radiation-induced trismus occurring after radiotherapy for nasopharyngeal cancer. Laryngoscope. 2005;115:1458–1460.
Goldstein M, Maxymiw WG, Cummings BJ, Wood RE. The effects of antitumor irradiation on mandibular opening and mobility: a prospective study of 58 patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:365–373.
Israel IA, Syrop SB. The important role of motion in the rehabilitation of patients with mandibular hypomobility: a review of the literature. J Craniomandibular Pract. 1997;15:1.
Miller EH, Quinn AI. Dental considerations in the management of head and neck cancer patients. Otolaryngol Clin North Am. 2006;39:319–329.
Hepburn, G. Contracture and stiff joint management with Dynasplint. J Ortho Sports Phys Ther. 1987;8:498–504.
MacKay-Lyons M. Low-load, prolonged stretch in treatment of elbow flexion contractures secondary to head trauma: a case report. Phys Ther. 1989;69:292–296.
Schenk I, Vesper M, Nam VC. Initial results using extracorporeal low energy shockwave therapy ESWT in muscle reflex-induced lock jaw [in German]. Mund Kiefer Gesichtschir. 2002;6:351–355.
Willis B. Post-TBI gait rehabilitation. Applied Neurol. 2007;3:25–26.
Dijkstra PU, Sterken MW, Pater R, Spijkervet FK, Roodenburg JL. Exercise therapy for trismus in head and neck cancer. Oral Oncol. 2007;43:389–394.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shulman, D.H., Shipman, B. & Willis, F.B. Treating trismus with dynamic splinting: A cohort, case series. Adv Therapy 25, 9–16 (2008). https://doi.org/10.1007/s12325-008-0007-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-008-0007-0