Abstract
Multiple recurrent waves of the coronavirus disease 2019 (COVID-19) resulted in major fluctuations in blood supply and demand, which presented a major challenge for the blood centres to maintain adequate blood inventory. Hence, the primary aim of the present study was to determine whether safety stock as a simple mathematical tool can be used to maintain optimum blood inventory to meet all blood demands. The secondary aim of the study was to test whether daily blood stock index (DBSI), which was a novel index developed by the authors and derived from the calculated safety stock, can be used to minimize blood wastage due to the outdating of packed red blood cells (PRBC)/whole blood (WB) units. The present study was a descriptive, cross-sectional study conducted from 1st October 2019 to 31st December 2021 at a blood centre of a tertiary care hospital. For the purpose of data analysis, the time period of study was divided into 7 periods signifying different phases during the COVID-19 outbreak. Data of PRBC/WB (referred to as red cell) collection, red cell issue and the daily red cell stock were collected for these 7 time periods. Safety stock, percentage of out-dated whole blood/packed red blood cell units (OB) and DBSI were calculated based on the data extracted. Red cell collection as well as red cell utilization decreased during the 1st as well as the 2nd wave of the COVID-19 outbreak. The blood centre was able to meet the blood demand of the hospital at all times, as the daily average red cell stock remained above the calculated safety stock during all periods. OB (12.4%) and DBSI (2.3) were highest during the lockdown period of second wave of COVID-19 outbreak (period E). A strong direct relationship was seen between OB (dependent variable) and DBSI (predictor variable) [R = 0.79; p = 0.03]. Firstly, safety stock is a simple, user-friendly mathematic tool which can be used for efficient blood inventory management not only at times of a pandemic/disaster but also during routine times. Secondly, DBSI is a logical and empirical tool to reduce OB units and consequently reduce blood wastage.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The coronavirus disease 2019 (COVID-19) spread at a very rapid pace in the world, and as a result, India declared a complete lockdown on 24th March 2020 [1]. Only emergency services personnel were allowed movement during the complete lockdown period. The abrupt lockdown resulted in the cancellation of voluntary blood donation camps throughout the country which resulted in a drastic reduction in blood collection severely affecting the blood transfusion services (BTS) [2]. Subsequently, an advisory was issued by the Ministry of Health and Family Welfare, Government of India on 09.04.2020, containing a list of guidelines to ensure COVID appropriate behaviour at blood donation sites [3].
BTS form the backbone of any tertiary care hospital. Blood sufficiency is of paramount importance for any blood centre [4]. Meticulous maintenance of blood inventory is one of the main functions of BTS administration. The ultimate goal of any blood centre is to maintain adequate bloodstock to meet all blood demands while minimizing blood wastage as a result of units becoming outdated beyond the date of expiry. In current times, emphasis is on following evidence based transfusion medicine practices [5]. Several algorithms have been proposed in the past for the management of blood centre inventory [6,7,8]. Safety stock is one such model [9] and is defined as the reserve stock of an inventory required to meet demand for a specified period in case of no fresh stock is available to meet the demand during that specified period [10].
Multiple recurrent waves of the COVID-19 resulted in major fluctuations in blood supply and demand, which presented a major challenge for the blood centres to maintain adequate blood inventory [11,12,13]. At the same time, increased blood wastage due to outdating of blood units attributed to COVID-19 outbreak has been reported in various studies [2, 14]. Hence, the primary aim of the present study was to determine whether safety stock as a simple mathematical tool can be used to maintain optimum blood inventory to meet all blood demands. The secondary aim of the study was to test whether daily blood stock index (DBSI), which was a novel index, developed by the authors and derived from the calculated safety stock, can be used to minimize blood wastage due to the outdating of packed red blood cells (PRBC)/whole blood (WB) units.
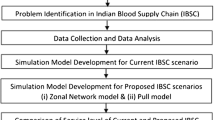
Materials and Methods
Study Design, Time Definitions and Study Procedure
The present study was a descriptive cross-sectional study conducted from 1st October 2019 to 31st December 2021 at a blood centre of a tertiary care hospital and research institute located in a hilly district of North India. Data was extracted from the blood centre records on the parameters namely: (i) total number of blood units collected; (ii) total number of PRBC/WB issued; (iii) total number of outdated PRBC/WB units beyond the date of expiry; (iv) daily stock of PRBC/WB units.
Based on this data, blood safety stock for PRBC/WB was calculated. Safety stock was defined as the bloodstock, sufficient to meet PRBC/WB (referred to as red cell) requirements for a period of 7 days (1 week) if the blood collection stops completely and blood usage remains to the maximum. Safety stock was calculated using the following formula [10]:
Average lead time is defined as the time which is required for the production/manufacture of the product before the product is included in the inventory. In our hospital, usually, the average lead time is 2 days (0.28 weeks) which includes the time for collection, testing and then labelling of units.
The maximum lead time depends on the type of disaster. It is the time period for which a disaster hampers the capacity of the blood centre to collect the blood units. Lockdown guidelines during COVID-19 outbreak in India were mostly issued for a period of 7 days at one time after which time the COVID-19 situation was reviewed and fresh guidelines were issued accordingly. Hence, in the present study, the maximum lead time as a result of the COVID-19 outbreak was taken as 7 days (1 week).
For the purpose of data analysis, the study was divided into 7 time periods as follows:
-
(i)
Period A: The pre-COVID-19 period (1st October 2019–23rd March 2020);
-
(ii)
Period B: The lockdown period during 1st wave of the COVID-19 outbreak (24th March 2020–8th June 2020);
-
(iii)
Period C: The unlocked period during the 1st wave of the COVID-19 outbreak (9th June–27th October 2020);
-
(iv)
Period D: The intervening period between the first and second wave of the COVID-19 outbreak (28th October 2020–7th April 2021);
-
(v)
Period E: The lockdown period during the 2nd wave of the COVID-19 outbreak (8th April 2021–21st June 2021);
-
(vi)
Period F: The unlocked period during the 2nd wave of the COVID-19 outbreak (22nd June 2021–7th August 2021);
-
(vii)
Period G: Time period after the 2nd wave of COVID-19 outbreak (8th August 2021–31st December 2021).
Since the duration of the seven periods was different in length, for the purpose of data analysis and comparison, the average weekly red cell collection and issue was calculated for each period.
Average daily red cell stock was calculated using the following formula:
Based on the average daily red cell stock and the calculated safety stock, the authors developed and derived a novel index termed as daily bloodstock index (DBSI) which was calculated using the following formula:
The percentage of outdated whole blood/packed red blood cell (OB) was calculated as per the formula used by the National Accreditation Board for Hospitals & Healthcare Providers (NABH), India [15]:
Therefore the hypothesis to be tested was:
H0 = DBSI does not predict OB; Ha = DBSI can be used to predict OB.
Outcome Measures Studied
The primary outcome studied was to determine the effectiveness of the safety stock formula as a mathematical tool for blood inventory during the COVID-19 pandemic. The secondary outcomes studied were: (i) to determine whether any relationship exists between DBSI and OB; (ii) to analyze the impact of the COVID-19 outbreak on BTS at a tertiary care hospital.
Statistical Analysis
Data was captured in Microsoft Excel spreadsheets. The quantitative data were expressed as mean and standard deviation (SD). A linear regression model was applied to study the effect of DBSI (predictor variable) on OB (outcome variable). Statistical tests were performed at a significance level of 0.05.
Ethical Considerations
The study was based on the ethical guidelines as given in the 1964 “Declaration of Helsinki” and its later amendments and was conducted after obtaining ethical clearance from the Institutional ethics committee vide IEC number MC/IEC/2021/26.
Results
The weekly red cell collection and red cell issued during periods were expressed as mean ± 2 standard deviations (SD) for uniform comparison. The daily red cell stock was also expressed as mean ± 2 standard deviations (SD). The results are presented under the seven different periods as shown in Table 1. The period wise fluctuations in blood collection and blood issues are shown in Fig. 1.
The average weekly red cell collection during 1st wave of COVID-19 lockdown (period B) decreased by 28.5% as compared to the pre-COVID period (period A) (30 ± 12 units vs. 42 ± 6 units). The average weekly red cell issued during period B was 35.8% less as compared to period A (25 ± 7 units vs. 39 ± 2 units).
Similarly, the average weekly red cell collection during the lockdown phase of 2nd wave of the COVID-19 outbreak (period E) was 16.6% less as compared to period D (30 ± 9 units vs. 36 ± 6 units). The average weekly red cell issued during period E was 26.4% less as compared to period D (25 ± 7 units vs. 34 ± 3 units). The calculated safety stock was the least for period E at 32 units.
The DBSI and OB during different periods are shown in Table 2. The maximum DBSI of 2.3 was seen during period E. Maximum OB of 12.3% was also seen during period E. Upon simple linear regression, a strong direct relationship was seen between OB (dependent variable) and DBSI (predictor variable) [R = 0.79; p = 0.03] (Fig. 2).
Discussion
Utilizing the Safety Stock Tool for Blood Centre Inventory Management
Efficient blood inventory management depends upon trained staff, effective implementation of standard operating protocols and effective inventory management tools [7]. A blood inventory management tool should be simple to understand and apply in order for it to be implemented in a blood centre. COVID-19 outbreak presented as a rapidly changing scenario which affected health care services around the world [16]. In the present study, the lockdown period of the first wave of the COVID-19 outbreak (period B) resulted in a drastic reduction in blood collection because of: (i) cancellation of voluntary blood donation camps; (ii) fear of contracting COVID-19 infection among the potential blood donors. The red cell collection during this period decreased to 30 ± 12 units per week which were 28.5% less as compared to the pre COVID period (period A). Similar findings were seen in other studies [12, 17, 18]. Hence period B presented the hardest challenge in terms of maintaining the average red cell stock inventory above the calculated red cell safety stock of 40 units. Various strategies were adopted to mitigate this decrease in blood collection. Firstly, an in-house blood donation camp was organized in collaboration with a local social organization following COVID appropriate behaviour. Secondly, regular repeat blood donors were counselled and informed about various measures taken by the blood centre to ensure social distancing and enhanced infection control measures. The donors who agreed to donate blood were issued a blood donation appointment letter which could be utilized as a movement pass.
In addition, all the blood centre staff was counselled to strictly follow the first in first out (FIFO) policy [19]. Interestingly, the red cell demand also decreased during period B as the average red cell issued during this period was 39 ± 2 units per week which were 35.8% less as compared to the pre-COVID period (period A). This was because the elective surgeries were postponed and more beds and hospital manpower were reserved for the management of COVID-19 patients. Due to the abovementioned interventions, the decrease in red cell collection was less as compared to the decrease in red cell utilization (28.5% vs 35.8%) and the blood centre was able to maintain the average daily red cell stock more than the calculated safety stock levels at all times during period B.
During period C, majority of the restrictions were gradually removed by the government. There was an increase in the average weekly red cell collection (51 ± 12 units) as well as the average weekly red cell issued (51 ± 4 units). The increase in red cell utilization was more than the collection during this period (104% vs. 70%). This can be attributed to the fact that a lot more information became available about COVID-19 and the hospitals were able to create mechanisms for providing both COVID and non-COVID health care services at the same time [20]. The total capacity of the hospital was also expanded from 500 to 700 beds. At the same time, the fear of COVID-19 also decreased among the general public [21]. However, the blood centre was successful in maintaining the average daily red cell stock above the calculated safety stock level by (i) strict implementation of the FIFO policy; (ii) increasing the number of voluntary blood donation camps; (iii) increased communication with the end-user clinicians for following restrictive strategy for blood transfusion [22].
Period D was the intervening period between the 1st and 2nd waves of the COVID-19 pandemic. The blood centre was able to maintain average daily red cell stock and remained above the calculated safety stock level at all times during this period without any special measures. Period E corresponded to the lockdown period of the 2nd wave of the COVID-19 pandemic which resulted in an overwhelming of health care facilities and the return of the lockdown measures to control the spread of the COVID-19 infection. Having learnt the lessons from the lockdown period of 1st wave of the pandemic, the blood centre was better prepared for period E. The blood collection only decreased by 16.6% compared to period D. However, the red cell demand decreased by 26.4% as compared to period D. This is again attributed to increased allocation of beds and manpower for COVID-19 management and postponement of elective surgeries. Since the % decrease in red cell demand was greater than the percentage decrease in blood collection, the average daily red cell stock reached 73 ± 6 units which was much higher than the calculated safety stock of 32 units for period E. This resulted in an increase in the total number of “near expiry date red cell units”. Some of the red cell units were transferred to the blood centre of a government hospital in another district of the state. However, eventually, the increased DBSI (2.3) resulted in increased wastage of blood due to the OB units during period E.
As seen in period C (the unlock period of the 1st wave of COVID-19), period F (the unlock period of the 2nd wave of COVID-19) also witnessed an increase in red cell demand by 52% as compared to period E as a result of reopening of non-COVID services in hospitals. Similarly, the blood collection also increased (↑ 43.3%) but efforts were made to decrease the gap between the average daily red cell stock and the calculated safety stock to decrease blood wastage. Finally, during period G (the endemic stage of COVID-19), the red cell demand increased by 28.9%, while blood collection was increased only by 9.3% to achieve further correction in the average daily bloodstock in line with the calculated safety stock to decrease blood wastage.
COVID-19 pandemic is a learning lesson that blood centres should be prepared for periodic health crises [16]. In the present study, by keeping the average daily blood stock above the calculated safety stock levels, the blood centre was able to meet the red cell requirements of the tertiary care hospital at all times.
Validity of OB as a Quality Indicator of Blood Wastage and the Relationship Between DBSI and OB
Blood stocks management scheme, which was established in United Kingdom in 2001, uses wastage as percentage of issue (WAPI) as an indicator of blood wastage [8]. WAPI is inversely proportional to blood utilization. In contrast, OB is inversely proportional to blood collection. Blood centres are in a much better position to control or optimize blood collection as it is the direct control of blood centre. Blood issued on the other end is related to blood demand and is dependent upon the end user clinical department. In 2016, WAPI was replaced by OB as a measure of blood wastage and also as a quality indicator of BTS by NABH, India [15]. Ideally, blood centres should try to achieve an OB of less than 7% for PRBC [23].
In the present study, upon simple linear regression, a strong direct relationship was seen between OB (dependent variable) and DBSI (predictor variable) [R = 0.79; p = 0.03]. The maximum DBSI of 2.3 was seen in period E (the lockdown period of the 2nd wave of the COVID-19 pandemic) which resulted in an increase in the “near expiry date units” and was directly responsible for high OB during period E as well as period F. Hence, based on the results of present study, it is suggested that to achieve minimum OB, the blood collection should be adjusted so that DBSI should be kept in the range of 1.4–1.7. If a blood centre is supporting more trauma patients and obstetric emergencies, then the DBSI should be kept near the upper range and for blood centre supporting more of routine surgery and medicine cases, the DBSI should be kept near to the lower range.
A limitation of the present study was that it was performed in blood centre of a tertiary care teaching hospital situated in a remote hilly location with relatively low demand/ consumption of PRBC and hence it was easier to manage blood collection accordingly. Therefore, whether these indices can be applied in blood centres of hospitals with large demand/consumption needs to be ascertained.
Conclusions
To sum up, the COVID-19 outbreak had a significant impact on the BTS. Safety stock is a simple, user-friendly mathematic formula which can be used for efficient blood inventory management. At the same time, DBSI, which an index derived from the calculated safety stock, is a logical and empirical tool to reduce OB units and consequently reduce blood wastage. However, it remains to be seen whether similar results can be reproduced in other blood centres of hospitals with large scale PRBC consumption, before the DBSI can be established as a predictor of OB.
References
Soni P (2021) Effects of COVID-19 lockdown phases in India: an atmospheric perspective. Environ Dev Sustain 23(8):12044–12055
Tripathi PP, Kumawat V, Patidar GK (2022) Donor’s perspectives on blood donation during Covid-19 pandemic. Indian J Hematol Blood Transfus 38(3):536–545. https://doi.org/10.1007/s12288-021-01504-y
Ministry of Health and Family Welfare. Government of India. Advisory for Voluntary Blood Donation during COVID-19 Pandemic. Accessed 9 Apr 2020. https://www.mohfw.gov.in/pdf/NBTCGUIDANCEFORCOVID19.pdf. Last Accessed 18 May 2022
Bönig H, Schmidt M, Hourfar K, Schüttrumpf J, Seifried E (2012) Sufficient blood, safe blood: can we have both? BMC Med 10:29. https://doi.org/10.1186/1741-7015-10-29
Garraud O, Vuk T, Lozano M, Tissot JD (2020) Transfusion medicine: overtime paradigm changes and emerging paradoxes. Transfus Clin Biol 27(4):262–267
Sun X, Xu Z, Feng Y et al (2021) RBC inventory-management system based on XGBoost model. Indian J Hematol Blood Transfus 37(1):126–133. https://doi.org/10.1007/s12288-020-01333-5
Stanger SH, Yates N, Wilding R, Cotton S (2012) Blood inventory management: hospital best practice. Transfus Med Rev 26(2):153–163
Chapman JF, Cook R (2002) The Blood Stocks Management Scheme, a partnership venture between the National Blood Service of England and North Wales and participating hospitals for maximizing blood supply chain management. Vox Sang 83(3):239–246
Radasanu AC (2016) Inventory management, service level and safety. J Public Admin Finance Law Invent 9:145–153
Lestari F, Ulfah, Nugraha N, Azwar B (2019) Managing inventory on blood supply chain. In: Ao SI, Gelman L, Kim H (eds) Transactions on engineering technologies. WCE, 2017. Springer, Singapore, pp 353–361. https://doi.org/10.1007/978-981-13-0746-1_27
Boroumand-Noughabi S, Rahmati A, Morovatdar N, Keramati M (2022) Significant decrease in the transfusion rates during the COVID-19 pandemic in the North East of Iran. TransfusClin Biol 29(2):181–182
Grandone E, Mastroianno M, Caroli A, Ostuni A (2020) Blood supply and transfusion support in southern Italy: findings during the first four weeks of the SARS-CoV-2 pandemic. Blood Transfus 18(3):230–232. https://doi.org/10.2450/2020.0107-20
Yahia AIO (2020) Management of blood supply and demand during the COVID-19 pandemic in King Abdullah Hospital, Bisha, Saudi Arabia. Transfus Apher Sci 59(5):102836. https://doi.org/10.1016/j.transci.2020.102836
Jacobs JW, Booth GS (2022) Blood shortages and changes to massive transfusion protocols: survey of hospital practices during the COVID-19 pandemic. Transfus Apher Sci 61(1):103297
Accreditation Standards on Blood Bank/Blood Centres and Transfusion Services (2016) National Accreditation Board for Hospitals & Healthcare Providers (NABH), 3rd edn. New Delhi, India
Garraud O (2020) COVID-19: is a paradigm change to be expected in health care and transfusion medicine? TransfusClin Biol 27(2):59–60
Barnes LS, Al-Riyami AZ, Ipe TS et al (2022) COVID-19 and the impact on blood availability and transfusion practices in low- and middle-income countries. Transfusion 62(2):336–345
Costa CB, Cortez AJP, Adão DD et al (2021) Optimization of red blood cell unit storage during SARS-COV-2 Pandemic: adopting new strategies to ensure supply in a decentralized blood bank in Brazil. HematolTransfus Cell Ther 43(3):229–235
Mishra S, Daga A, Gupta A (2021) Inventory management practices in the blood bank of an institute of national importance in India. J Family Med Prim Care 10(12):4489–4492
Ministry of Health and Family Welfare. Government of India. Updated Advisory for managing Health care workers working in COVID and Non-COVID areas of the hospital. Accessed 15 May 2020. Available from: https://www.mohfw.gov.in/. Last Accessed 15 May 2022
Buneviciene I, Bunevicius R, Bagdonas S, Bunevicius A (2021) COVID-19 media fatigue: predictors of decreasing interest and avoidance of COVID-19-related news. Public Health 196:124–128
Salpeter SR, Buckley JS, Chatterjee S (2014) Impact of more restrictive blood transfusion strategies on clinical outcomes: a meta-analysis and systematic review. Am J Med 127(2):124-131.e3
National Health Mission. Ministry of Health and Family Welfare. Government of India. Guidelines for recovery of processing charges for blood and blood components. Available from: http://naco.gov.in/sites/default/files/Guidelines%20on%20recovery%20of%20Processing%20Charges%20for%20Blood%20%26%20Blood%20Components.pdf. Last Accessed 14 May 2022
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical Approval
The study was conducted after taking approval from the Institutional Ethics Committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bansal, N., Bansal, Y., Raturi, M. et al. Blood Inventory Management During COVID-19 Pandemic Using a Simple Mathematical Tool: A Two-Year Study from a Tertiary Care Hospital in North India. Indian J Hematol Blood Transfus 39, 655–661 (2023). https://doi.org/10.1007/s12288-023-01631-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12288-023-01631-8