Abstract
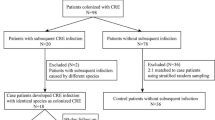
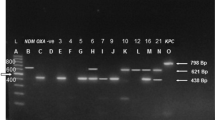
Faecal carriage of Carbapenem-resistant Enterobacteriaceae (CRE) is being observed as an important risk factor for bacteremia among patients with hematological malignancies. A prospective surveillance study was conducted among these patients to determine the gut colonization of CRE. Rectal/perianal swabs were collected to isolate CRE. Carbapenem resistance was detected by disk diffusion, modified-Hodge, Carba-NP test, and PCR for blaNDM-1, blaKPC, blaOXA-48, blaVIM, blaIMP genes. A total of 209 CRE isolates were identified from 151 patients. E. coli was the most common (83.2%) CRE identified, followed by Klebsiella spp. (9.6%). The majority of CRE were observed resistant to ertapenem (86%). blaNDM-1 was the most common gene (57.3%), followed by blaOXA-48 (37.8%). 26.8% isolates found to carry both blaNDM-1 and blaOXA-48 genes. CRE is increasingly observed to cause bacteremia among hematological malignancy patients due to increased colonization. Screening for gut CRE colonization is necessary to guide empirical therapy and apply infection control measures among these patients.
Similar content being viewed by others
References
World Health Organization (2014) Antimicrobial resistance global report on surveillance. World Health Organization, Geneva. http://apps.who.int/iris/bitstream/10665/112642/1/9789241564748_eng.pdf?ua1. (Accepted 12 Oct 2019)
Satlin MJ, Jenkins SG, Walsh TJ (2014) The global challenge of carbapenem-resistant Enterobacteriaceae in transplant recipients and patients with hematologic malignancies. Clin Infect Dis 58:1274–1283
Trecarichi EM, Pagano L, Martino B, Candoni A, Di Blasi R, Nadali G et al (2016) Bloodstream infections caused by Klebsiella pneumoniae in onco-hematological patients: clinical impact of carbapenem resistance in a multicentre prospective survey. Am J Hematol 91:1076–1081
Montagnani C, Prato M, Scolfaro C, Colombo S, Esposito S, Tagliabue C et al (2016) Carbapenem-resistant Enterobacteriaceae infections in children: an Italian retrospective multicenter study. Pediatr Infect Dis J 35:862–868
Zhang R, Liu L, Zhou H, Chan EW, Li J, Fang Y et al (2017) Nationwide surveillance of Clinical Carbapenem-resistant Enterobacteriaceae (CRE) Strains in China. EbioMedicine 19:98–106
Mittal G, Gaind R, Kumar D, Kaushik G, Gupta KB, Verma PK et al (2016) Risk factors for fecal carriage of carbapenemase producing Enterobacteriaceae among intensive care unit patients from a tertiary care center in India. BMC Microbiol 16:138
Das P, Singh AK, Pal T, Dasgupta S, Ramamurthy T, Basu S (2011) Colonization of the gut with Gram-negative bacilli, its association with neonatal sepsis and its clinical relevance in a developing country. J Med Microbiol 60:1651–1660
Queenan AM, Bush K (2007) Carbapenemases: the versatile beta-lactamases. Clin Microbiol Rev 20:440–458
Satlin MJ, Walsh TJ (2017) Multidrug-resistant Enterobacteriaceae, Pseudomonas aeruginosa, and vancomycin-resistant Enterococcus: three major threats to hematopoietic stem cell transplant recipients. Transplant Infect Dis. https://doi.org/10.1111/tid.12762
CDC 2012 CRE Toolkit: Guidance for Control of Carbapenem‐Resistant Enterobacteriaceae (CRE). http://www.cdc.gov/hai/organisms/cre/cre‐toolkit/index.html. (Accepted 25 Oct 2019)
Clinical and Laboratory Standards Institute, 26 ed. Wayne: CLSI supplement M100S.2016
Asthana S, Mathur P, Tak V (2014) Detection of Carbapenemase production in gram-negative bacteria. J Lab Phys 6:69–75
Lustberg MB (2012) Management of neutropenia in cancer patients. Clin Adv Hematol Oncol 10(12):825–826
Kokkayil P, Agarwal R, Mohapatra S, Bakshi S, Das B, Sood S et al (2018) Bacterial profile and antibiogram of blood stream infections in febrile neutropenic patients with hematological malignancies. J Infect Dev Ctries 12:442–447
Gopalakrishnan V, Jenq RR (2018) Implicating or exonerating the gut microbiome in blood–borne infection. Nat Med 24(12):1788–1789
Aklilu A, Manilal A, Ameya G, Woldemariam M, Siraj M (2020) Gastrointestinal tract colonization rate of extended-spectrum beta-Lactamase- and Carbapenemase-producing Enterobacteriaceae and associated factors among hospitalized patients in Arba Minch General Hospital, Arba Minch, Ethiopia. Infect Drug Resist 13:1517–1526
Montassier E, Al-Ghalith GA, Ward T, Corvec S, Gastinne T, Potel G, Moreau P, de la Cochetiere MF, Batard E, Knights D (2016) Pretreatment gut microbiome predicts chemotherapy-related bloodstream infection. Genome Med 8(1):49
Girmenia C, Viscoli C, Pichiocchi A, Cudillo L, Botti S, Errico A et al (2015) Management of carbapenem resistant Klebsiella pneumoniae infections in stem cell transplant recipients: an Italian multidiciplinary consensus statement. Hematologia 100:e373
Satlin MJ, Chen L, Patel G, Gomez-Simmonds A, Weston G, Kim AC et al (2017) Multicenter clinical and molecular epidemiological analysis of Bacteremia due to Carbapenem-Resistant Enterobacteriaceae (CRE) in the CRE epicenter of the United States. Antimicrob Agents Chemother 61:e02349-e2416
Zilberberg MD, Shorr AF (2013) Prevalence of multidrug-resistant Pseudomonas aeruginosa and carbapenem-resistant Enterobacteriaceae among specimens from hospitalized patients with pneumonia and bloodstream infections in the United States from 2000 to 2009. J Hosp Med 8:559–563
Baljin B, Baldan G, Chimeddorj B, Tulgaa K, Gunchin B, Sandag T et al (2016) Faecal carriage of gram-negative multidrug-resistant bacteria among patients hospitalized in two centres in Ulaanbaatar, Mongolia. PLoS ONE 11:e0168146
Salomão MC, Guimarães T, Duailibi DF, Perondi M, Letaif L, Montal AC et al (2017) Carbapenem-resistant Enterobacteriaceae in patients admitted to the emergency department: prevalence, risk factors, and acquisition rate. J Hosp Infect 97:241–246
Ouchar Mahamat O, Tidjani A, Lounnas M, Hide M, Benavides J, Somasse C et al (2019) Fecal carriage of extended-spectrum β-lactamase-producing Enterobacteriaceae in hospital and community settings in Chad. Antimicrob Resist Infect Control 8:169
Nicolas-Chanoine MH, Vigan M, Laouénan C, Robert J, E-carb Study Group (2019) Risk factors for carbapenem-resistant Enterobacteriaceae infections: a French case–control–control study. Eur J Clin Microbiol Infect Dis. 38(2):383–393
Torio RO, Paras DNT, Abad CLR (2019) 495 Risk factors of Carbapenem-resistant Enterobacteriaceae (CRE) infections among intensive care unit (ICU) patients in a Tertiary Hospital in the Philippines. Open Forum Infect Dis 6(2):S241–S242
Chemaly RF, Simmons S, Dale C Jr et al (2014) The role of the healthcare environment in the spread of multidrug-resistant organisms: update on current best practices for containment. Ther Adv Infect Dis 2(3–4):79–90
Magiorakos AP, Burns K, Rodríguez Baño J et al (2017) Infection prevention and control measures and tools for the prevention of entry of Carbapenem-resistant Enterobacteriaceae into healthcare settings: guidance from the European Centre for Disease Prevention and Control. Antimicrob Resist Infect Control 6:113
Chung HS, Yong D, Lee M (2016) Mechanisms of Ertapenem resistance in Enterobacteriaceae isolates in a tertiary university hospital. J Investig Med 64:1042–1049
Bir R, Mohapatra S, Kumar A, Tyagi S, Sood S, Das BK et al (2019) Comparative evaluation of in-house Carba NP test with other phenotypic tests for rapid detection of Carbapenem-resistant Enterobacteriaceae. J Clin Lab Anal 33:e22652
Nordmann P, Naas T, Poirel L (2011) Global spread of Carbapenemase-producing Enterobacteriaceae. Emerg Infect Dis 17:1791–1798
Yong D, Toleman MA, Giske CG, Cho HS, Sundman K, Lee K et al (2009) Characterization of a new metallo-beta-lactamase gene, bla(NDM-1), and a novel erythromycin esterase gene carried on a unique genetic structure in Klebsiella pneumoniae sequence type 14 from India. Antimicrob Agents Chemother 53:5046–5054
Kumarasamy KK, Toleman MA, Walsh TR, Bagaria J, Butt F, Balakrishnan R, Chaudhary U et al (2010) the emergence of a new antibiotic resistance mechanism in India, Pakistan, and the U.K.: a molecular, biological, and epidemiological study. Lancet Infect Dis 10:597–602
Taneja N, Sharma M (2019) Antimicrobial resistance in the environment: Indian scenario. Ind J Med Res 149:119–128
Author information
Authors and Affiliations
Contributions
Dr. A.K. had done the laboratory work and drafting of the manuscript. Dr. S.M. was the chief investigator, gave the concept, design of the study, and drafting of the manuscript. Dr. R.B. helped in the analysis of data. Mr. S.T. had helped in the molecular work. Dr. S.B. and Dr. M.M. had revised the manuscript critically for intellectual content. H.G. had contributed to writing the manuscript. Dr. S.S. had helped in the analysis of data. Dr. B.K.D. had revised it critically for intellectual content. Dr. A.K. had given the final approval of the version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics Approval
Ethics approval had been taken for this study by the institutional ethical committee, and all the protocols were followed as per the ethical standards.
Consent to Participate
Informed consent had been taken from the participants.
Consent of Publication
Consent had been taken from all the contributing authors for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kumar, A., Mohapatra, S., Bir, R. et al. Intestinal Colonization Due to Carbapenem-Resistant Enterobacteriaceae Among Hematological Malignancy Patients in India: Prevalence and Molecular Charecterisation. Indian J Hematol Blood Transfus 38, 1–7 (2022). https://doi.org/10.1007/s12288-021-01415-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12288-021-01415-y