Abstract
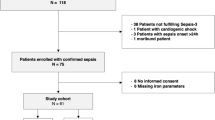
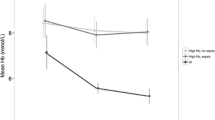
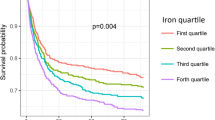
There is lack of data on iron metabolism in critically ill sepsis children from population with high prevalence of iron deficiency (ID). The study was designed to study impact of sepsis on iron parameters in children with ID. Sepsis patients (age 6–59 months) and their apparently healthy sibling/cousin as controls were enrolled in this case–control pilot study. Serum iron, TIBC, transferrin saturation, ferritin and sTfR were measured in the two groups. sTfR-Ferritin index was calculated. Patients (n = 134) were significantly underweight compared to controls (n = 54) (WAZ score < − 2; 58% vs. 28%; p < 0.001). Serum iron and sTfR (mg/L) were lower [71.5 (51.0, 115.0) vs. 87.0 (64.5, 130.5), p = 0.068; 3.1 (2.1, 4.5) vs. 3.5 (2.8, 4.8), p = 0.026 respectively] while serum ferritin was higher [229 (94, 484.5) vs. 22 (9.2, 51); p < 0.001] in patients compared to controls. sTfR-Ferritin index was lower in patients [1.3 (0.8, 2.3) vs. 2.5 (1.8, 4.5); p < 0.001]. ROC AUC (patients vs. controls) were 0.89 (95% CI 0.83–0.95) and 0.76 (95% CI 0.68–0.85) for ferritin and sTfR-ferritin index respectively. Survivors and non-survivors were similar in terms of iron parameters. Sepsis-induced alterations in iron parameters among ID children are complex. Qualitatively it is similar (with quantitative differences) to non-ID adult population. Lack of correlation of iron parameters with mortality may be due to ID-associated immune dysfunction.

Similar content being viewed by others
References
Darveau M, Denault AY, Blais N et al (2004) Bench-to-bedside review: iron metabolism in critically ill patients. Crit Care 8:356–362
Tacke F, Nuraldeen R, Koch A et al (2016) Iron parameters determine the prognosis of critically ill patients. Crit Care Med 44:1049–1058
Piagnerelli M, Boudjeltia KZ, Gulbis B, Vanhaeverbeek M, Vincent JL (2007) Anemia in sepsis: the importance of red blood cell membrane changes. Transfus Altern Transfus Med 9:143–149
Cherayil BJ (2011) The role of iron in the immune response to bacterial infection. Immunol Res 50:1–9
Sazawal S, Black RE, Ramsan M et al (2006) Effects of routine prophylactic supplementation with iron and folic acid on admission to hospital and mortality in preschool children in a high malaria transmission setting: community-based, randomised, placebo-controlled trial. Lancet 367:133–143
Veenemans J, Milligan P, Prentice AM et al (2011) Effect of supplementation with zinc and other micronutrients on malaria in Tanzanian children: a randomised trial. PLoS Med 8:e1001125
Soofi S, Cousens S, Iqbal SP et al (2013) Effect of provision of daily zinc and iron with several micronutrients on growth and morbidity among young children in Pakistan: a cluster-randomised trial. Lancet 382:29–40
Bhatnagar S, Lodha R, Choudhury P et al (2007) IAP guidelines 2006 on hospital based management of severely malnourished children (adapted from the WHO Guidelines). Indian Pediatr 44:443–461
Ashworth A, Khanum S, Jackson A, Schofield C. Guidelines for the inpatient treatment of severely malnourished children. 1. Guidelines for the inpatient treatment of severely malnourished children. World Health Organization 2003. Available at https://www.who.int/nutrition/publications/guide_inpatient_text.pdf. Accessed on April 1, 2020
Shah A, Roy NB, McKechnie S et al (2016) Iron supplementation to treat anaemia in adult critical care patients: a systematic review and meta-analysis. Crit Care 20:306
Gonmei Z, Toteja GS (2018) Micronutrient status of Indian population. Indian J Med Res 148:511–521
Skikne BS, Flowers CH, Cook JD (1990) Serum transferrin receptor: a quantitative measure of tissue iron deficiency. Blood 75:1870–1876
Shin DH, Kim HS, Park MJ et al (2015) Utility of access soluble transferrin receptor (sTfR) and sTfR/log ferritin index in diagnosing iron deficiency anemia. Ann Clin Lab Sci 45:396–402
Oustamanolakis P, Koutroubakis IE, Messaritakis I et al (2011) Soluble transferrin receptor-ferritin index in the evaluation of anemia in inflammatory bowel disease: a case–control study. Ann Gastroenterol 24:108–114
Krawiec P, Pac-Kożuchowska E (2019) Soluble transferrin receptor and soluble transferrin receptor/log ferritin index in diagnosis of iron deficiency anemia in pediatric inflammatory bowel disease. Dig Liver Dis 51:352–357
Goyal R, Das R, Bambery P et al (2008) Serum transferrin receptor-ferritin index shows concomitant iron deficiency anemia and anemia of chronic disease is common in patients with rheumatoid arthritis in North India. Indian J Pathol Microbiol 51:102–104
Murthy S, Kissoon N (2018) Hyperferritinemia in sepsis in children: ironing out the global details. Pediatr Crit Care Med 19:692–693
Goldstein B, Giroir B, Randolph A (2005) International Consensus Conference on Pediatric Sepsis. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med 6:2–8
Revised recommendations for the measurements of the serum iron in human blood (1990) Iron panel of the international committee for standardization in haematology. Br J Haematol 75:615–616
Saarinen UM, Siimes MA (1977) Developmental changes in serum iron, total iron-binding capacity, and transferrin saturation in infancy. J Pediatr 91:875–877
Punnonen K, Irjala K, Rajamäki A (1997) Serum transferrin receptor and its ratio to serum ferritin in the diagnosis of iron deficiency. Blood 89:1052–1057
Lopez A, Cacoub P, Macdougall PC, Peyrin-Biroulet L (2016) Iron deficiency anaemia. Lancet 387:907–916
R Core Team (2019) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. Available at https://www.R-project.org/
Robin X, Turck N, Hainard A et al (2011) pROC: an open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinform 12:77
Wickham H (2016) ggplot2: elegant graphics for data analysis. Springer, New York
Wickham H, Bryan J (2019) readxl: Read Excel Files. R package version 1.3.1.2019. Available at https://CRAN.R-project.org/package=readxl
Schloerke B, Crowley J, Cook D, Briatte F, Marbach M, Thoen E, Elberg A, Larmarange J (2020) GGally: Extension to ‘ggplot2’. R package version 1.5.0. 2020. Available at https://CRAN.R-project.org/package=GGally
Sjoberg DD, Hannum M, Whiting K, Zabor EC (2019) gtsummary: presentation-ready data summary and analytic result tables. R package version 1.2.4. 2019. Available at https://CRAN.R-project.org/package=gtsummary
Ghosh S, Baranwal AK, Bhatia P et al (2018) Suspecting hyperferritinemic sepsis in iron-deficient population: do we need a lower plasma ferritin threshold? Pediatr Crit Care Med 19:e367–e373
Heming N, Montravers P, Lasocki S (2011) Iron deficiency in critically ill patients: highlighting the role of hepcidin. Crit Care 15:210
Finch CA, Huebers H (1982) Perspectives in iron metabolism. N Engl J Med 306:1520–1528
Worwood M (2002) Serum transferrin receptor assays and their application. Ann Clin Biochem 39:221–230
Fahmey M, Young SP (1993) Modulation of iron metabolism in monocyte cell line U937 by inflammatory cytokines: changes in tranferrin uptake, iron handling and ferritin mRNA. Biochem J 296:175
Marković M, Majkić-Singh N, Ignjatović S, et al (2007) Reticulocyte haemoglobin content vs. soluble transferrin receptor and ferritin index in iron deficiency anaemia accompanied with inflammation. Int J Lab Hematol 29:341–346
Beesley R, Filteau S, Tomkins A et al (2000) Impact of acute malaria on plasma concentrations of transferrin receptors. Trans R Soc Trop Med Hyg 94:295–298
Williams TN, Maitland K, Rees DC et al (1999) Reduced soluble transferrin receptor concentrations in acute malaria in Vanuatu. Am J Trop Med Hyg 60:875–878
Olivares M, Walter T, Cook JD et al (2000) Usefulness of serum transferrin receptor and serum ferritin in diagnosis of iron deficiency in infancy. Am J Clin Nutr 72:1191–1195
Skikne BS, Punnonen K, Caldron PH et al (2011) Improved differential diagnosis of anemia of chronic disease and iron deficiency anemia: a prospective multicenter evaluation of soluble transferrin receptor and the sTfR/log ferritin index. Am J Hematol 86:923–927
Maggini S, Pierre A, Calder PC (2018) Immune function and micronutrient requirements change over the life course. Nutrients 10:1531. https://doi.org/10.3390/nu10101531
Acknowledgements
This study was performed at Division of Pediatric Critical Care, Advanced Pediatrics Center, Postgraduate Institute of Medical Education and Research, Chandigarh, India.
Author information
Authors and Affiliations
Contributions
Arun Kumar Baranwal: Conceptualization, Study design, Fund Acquisition, Data curation, Literature search, Original and Final draft preparation, Supervision of Statistical analysis, Guarantor. Reena Das: Conceptualization, Methodology, Laboratory analysis, Supervision, Critical review and Editing. Ramachandran Rameshkumar: Data collection, Data curation, Review and Editing. Praveen Kumar-M: Statistical analysis, Data curation, Software. Prateek Bhatia: Literature search, Review and Editing. Ashwini Nair: Literature search, Data curation, Statistical analysis.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.

Supplementary Figure 1
Multi-correlation plot between different iron parameters for patients and control. Spearman correlation coefficient [rho (ρ)] and associated p values are mentioned for each comparison. Density plots are depicted in the diagonal line.(JPEG 2888 kb)
Rights and permissions
About this article
Cite this article
Baranwal, A.K., Das, R., Rameshkumar, R. et al. Effect of Sepsis on Iron Parameters in a Population with High Prevalence of Malnutrition and Iron Deficiency: A Cross-Sectional Case–Control Pilot Study. Indian J Hematol Blood Transfus 37, 609–615 (2021). https://doi.org/10.1007/s12288-020-01393-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12288-020-01393-7