Abstract
Background
Dedicated breast positron emission tomography (dbPET) has been developed for detecting smaller breast cancer. We investigated the diagnostic performance of dbPET in patients with known breast cancer.
Methods
Eighty-two preoperative patients with breast cancer were included in the study (84 tumours: 11 ductal carcinomas in situ [DCIS], 73 invasive cancers). They underwent mammography (MMG), ultrasonography (US), and contrast-enhanced breast magnetic resonance imaging (MRI) before whole-body PET/MRI (WBPET/MRI) and dbPET. We evaluated the sensitivity of all modalities, and the association between the maximum standard uptake value (SUVmax) level and histopathological features.
Results
The sensitivities of MMG, US, MRI, WBPET/MRI and dbPET for all tumours were 81.2% (65/80), 98.8% (83/84), 98.6% (73/74), 86.9% (73/84), and 89.2% (75/84), respectively. For 11 DCIS and 22 small invasive cancers (≤ 2 cm), the sensitivity of dbPET (84.9%) tended to be higher than that of WBPET/MRI (69.7%) (p = 0.095). Seven tumours were detected by dbPET only, but not by WBPET/MRI. Five tumours were detected by only WBPET/MRI because of the blind area of dbPET detector, requiring a wider field of view. After making the mat of dbPET detector thinner, all 22 scanned tumours were depicted. The higher SUVmax of dbPET was significantly related to the negative oestrogen receptor status, higher nuclear grade, and higher Ki67 (p < 0.001).
Conclusions
The sensitivity of dbPET for early breast cancer was higher than that of WBPET/MRI. High SUVmax was related to aggressive features of tumours. Moreover, dbPET can be used for the diagnosis and oncological evaluation of breast cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most common cancer among women in Japan and worldwide. The morbidity associated with breast cancer in Japan is steadily increasing. The onset of breast cancer typically occurs at the age of 40–49 years in Asian countries, including Japan [1]. Younger women tend to have dense breast with less fat tissue compared with older women. Dense breast is one of the factors that reduce the sensitivity of mammography (MMG) in detecting breast cancer. There are some reports on extremely dense breast tending to have a higher risk of developing breast cancer than fatty breast [2]. Therefore, improving the accuracy of diagnostic imaging in dense breasts is a major challenge that must be urgently addressed.
Whole-body positron emission tomography (WBPET) using F-18 fluorodeoxyglucose (FDG) is widely used to evaluate the whole body for determining the stage and progression of breast cancer. Furthermore, the FDG uptake level is significantly associated with pathological and immunohistochemical factors [3,4,5,6,7,8]. However, WBPET is known to have a lower detection rate for smaller and lower grade breast cancers because of the limitation of spatial resolution and FDG uptake.
Breast positron emission tomography (PET) has been developed to detect early breast cancer and has been reported to be able to detect tumours sized < 1 cm, including both invasive cancers and ductal carcinomas in situ (DCIS), which are difficult to detect with WBPET [9,10,11]. Breast PET is classified into the following two types: the opposite type (positron emission mammography; PEM) and ring-shaped type (dedicated breast PET; dbPET) [12]. In PEM, the breast is compressed as in the scanning approach in an X-ray MMG. Using this type, it is possible to obtain multiple plane slices with a mobile detector in the sitting position. In contrast, dbPET with circumferentially arranged detectors enables imaging of the whole breast in the prone position, comparable to breast magnetic resonance imaging (MRI), and generates maximum-intensity projection images. Nishimatsu et al. [13] published a study comparing the sensitivity and specificity of dbPET and WBPET/computed tomography (CT). The lesion-based sensitivities of dbPET and WBPET/CT were 92% and 88%, respectively (p = 0.06). Moreover, dbPET was covered by the Japanese medical insurance in July 2013 on the condition that dbPET was performed on the same day as WBPET. In this study, we used the dbPET that was developed in Japan.
We investigated the imaging sensitivity of dbPET for breast cancer. For practical clinical application, we compared the sensitivity of dbPET with that of MMG, ultrasonography (US), contrast-enhanced MRI, and WBPET/MRI. We also analysed the association between the FDG uptake level on dbPET and histopathological features.
Patients and methods
Study design
This study was a combined effort of Showa University, Midtown Clinic, and Shimadzu Corporation. All patient recruitments were from Showa University Hospital between May 2015 and December 2016. Patient recruitment was continued during the study period. This study had a prospective design, and informed consent was obtained from all participants. However, the study was interrupted for approximately 6 months to improve the equipment mat described later. All WBPET/MRI and dbPET scanning were performed at Midtown Clinic. This study was conducted in accordance with the ethical principles of the Declaration of Helsinki and the ethical guidelines for human medical research (approved on 22 December 2014 by the Ministry of Health, Labour, and Welfare), was approved by the Institutional Review Board of Showa University Hospital (Approval number 1723), and registered on the University Hospital Medical Information Network (UMIN ID 000027227).
Patients
Patients who had been diagnosed with breast cancer but had not commenced treatment were included in the study. In total, 82 Japanese women with histologically diagnosed breast cancer (84 tumours) consented to participate in this study. In particular, 27 patients (33%) received some form of cancer treatment after scanning dbPET and WBPET/MRI. All patients underwent US, WBPET/MRI, and dbPET. Seventy-eight patients (80 tumours) underwent MMG and 70 (74 tumours) underwent MRI. All modalities were performed prior to the treatment of all patients.
Imaging protocol
All patients underwent WBPET/MRI using Biograph mMR® (Siemens Healthcare, Erlangen, Germany), followed by dbPET using the Elmammo® dbPET system (Shimadzu, Kyoto, Japan). WBPET/MRI was performed at 60 min after an F-18 FDG (3.0 MBq/kg) injection. First, WBPET/MRI was performed in the supine position, and breast PET/MRI with breast coil was performed in the prone position (magnetic resonance attenuation correction: volumetric interpolated breath-hold examination; 3-mm slice; repetition time, 3 ms; echo time, 1.03 ms; fractional anisotropy, 10; field of view [FOV], 450 mm). The total scanning time of WBPET/MRI and breast PET/MRI was approximately 60 min (scan time, 4 min/bed; image reconstruction: point-spread function; iteration, 3; subset, 21; filter, 4 mm; FOV, 420 mm; matrix, 172). The reason for the performance of additional breast PET/MRI in the prone position was to investigate the blind area of dbPET. The sensitivity of breast cancer by WBPET/MRI in this study was comprehensively evaluated using breast PET/MRI. The dbPET was performed 120 min after the F-18 FDG injection, and the emission time was 5 min per breast in the prone position. The detector consisted of four layers of a 32 × 32 cerium-doped lutetium gadolinium oxy-orthosilicate crystal array (crystal size, 1.44 × 1.44 × 18 mm), a light guide, and a 64-channel position-sensitive photomultiplier tube. The FOV was 185 × 156.5 mm. We initially used a 20-mm-thick mat on the detector. However, we changed the thickness of the mat from 20 to 5 mm, because there were some undetected tumours in the blind areas.
We compared the sensitivities of dbPET with those of the existing breast cancer modalities, including US, MMG, MRI, and WBPET/MRI. The US and MMG images were evaluated based on the guidelines for breast US [14] and mammography [15], respectively, by breast surgeons and radiologists at Showa University. Breast-enhanced MRI images were evaluated using the Breast Imaging Reporting and Data System (BI-RADS®) [16] by radiologists at Showa University. All PET images (WBPET/MRI and dbPET) were interpreted by one radiologist with over 6 years of experience as a nuclear medicine and diagnostic imaging specialist. The radiologist recognised in advance that the patients had breast cancer. However, the interpretations of WBPET/MRI and dbPET were performed without detailed information. At the study initiation, there was no consensus on the interpretation method for dbPET. Therefore, we regarded the lesion with SUVmax of ≥ 1 and the morphology suggesting a mass or segmental non-mass FDG uptake as the abnormal uptake. We considered cases with strong background breast fibroglandular uptake (bFGU) as those with an abnormal uptake, which was conspicuous from the bFGU.
Pathological diagnosis
In this study, we used histopathological information, which was obtained using needle biopsy before surgery or any drug treatments. We evaluated the histopathological features using histology, nuclear grade (NG), oestrogen receptor (ER) status, progesterone receptor (PgR) status, human epidermal growth factor 2 (HER2) status, and Ki67 labelling index (Ki67%). ER, PgR, and HER2 statuses were determined using the American Society of Clinical Oncology/College of American Pathologists guidelines for breast cancer [17, 18].
Statistical analysis
As this was an observational, prospective study, no formal sample size calculation was performed. The results are presented as the number and proportion of eligible populations. We analysed the characteristics of patients and clinicopathological features in the detected and undetected tumour groups using Pearson’s chi-squared test, Fisher’s exact test, and analysis of variance (ANOVA). The McNemar test was performed for the comparison of sensitivities. To analyse the relation between SUVmax and clinicopathological features, we used ANOVA and the t test. The SUVmax is expressed as mean ± standard deviation. We used the JMP professional software, version 15.0 (SAS Institute, Cary, NC, USA), for statistical processing. Statistical significance in all statistical tests was set at p < 0.05.
Results
The characteristics of the 82 patients (84 tumours) in this study are summarised in Table 1.
The median age of the patients included in this study was 50 (range, 32–85) years. The body mass index (BMI) tended to be higher in the detected than in the undetected group with no significant difference (p = 0.09). Four patients were diagnosed with stage IV breast cancer using WBPET/MRI. Eighty tumours (95.2%) were operable. Moreover, 27 patients (33%) received some form of cancer treatment after dbPET and WBPET/MRI. Seventy-five tumours (89.3%) were detected by dbPET but nine tumours (10.7%) were undetected. The dbPET detection rates of histological types in DCIS and invasive ductal carcinoma (IDC) cases were 81.8% and 92.7%, respectively. The two invasive lobular carcinoma (ILC) cases as well as the mucinous carcinoma case were undetected by dbPET. No significant differences were observed using dbPET between the detected and undetected groups in the clinical T stage (clinical size of the tumour), NG, ER, HER2 status, and Ki67% of the target tumours.
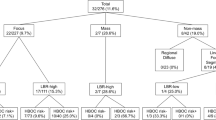
We compared the detected rates of dbPET and WBPET/MRI for all tumours, as shown in Fig. 1. Of 84 tumours, 68 (81%) were detected by both dbPET and WBPET/MRI. Neither dbPET nor WBPET/MRI detected four tumours (5%). Seven tumours (8%) were detected by dbPET only, but not by WBPET/MRI. The tumours included four cases of DCIS and three very small IDC cases. The details of those tumours detected only by dbPET are summarised in Table 2.
Five tumours (6%) were detected by WBPET/MRI only. Those tumours were located in the blind area of the dbPET detector. The out-of-field tumours triggered the need for improvement of the dbPET mat. Thus, we changed the mat thickness from 20 to 5 mm. After the reduction of the mat thickness, we restarted the study and scanned 22 patients. None of the 22 tumours were missed (Fig. 2).
Reducing the blind area of dbPET. a Detachable 20-mm mat and dbPET detector. b Right image: a sagittal view of the dbPET scanner using a 20-mm mat. The distance from the limit end of the chest wall was 32 mm; left image: a sagittal view of the dbPET scanner using a 5-mm mat. The distance from the limit end of the chest wall was 43 mm. Reducing the mat thickness was effective in reducing the blind area close to the chest wall. dbPET, dedicated breast positron emission tomography
Table 3 shows the sensitivity of each modality for 11 DCIS, 33 early breast cancers (11 DCIS and 22 small invasive cancers; invasive diameter, ≤ 20 mm), and all 84 tumours. US and MRI had the highest overall sensitivity (98.8% and 98.6%, respectively) for all breast cancers. For 11 DCIS, dbPET and MMG had the same sensitivity (81.8%), which was higher than that of WBPET/MRI (54.5%) without significant difference (p = 0.179). For 33 early breast cancers, the sensitivity of dbPET (84.9%) tended to be higher than that of WBPET/MRI (69.7%) and MMG (75.8%) but with no statistically significant difference (p = 0.095 and p = 0.365, respectively).
We analysed the association between the SUVmax of dbPET and the clinicopathological characteristics (Table 4). The SUVmax level tended to increase as the tumour diameter increased. However, there was no significant difference between the SUVmax and maximum infiltration diameter (p = 0.211), as well as between the HER2 status and SUVmax (p = 0.149). In contrast, the higher SUVmax of dbPET was significantly related to the negative ER status (p = 0.0001), higher NG (p = 0.0001), and higher Ki67 (p = 0.0002).
Discussion
dbPET has been developed to improve the detection of small breast cancers. One of the advantages of this study was the comparison of dbPET with other breast imaging modalities and the determination of breast cancer detectability, especially early breast cancer. In this study, the sensitivity of dbPET for all cases was 89%, similar to that of other reports (78–92%) [9, 11, 13, 19]. dbPET is a high-resolution molecular imaging machine for breast cancer with high sensitivity and specificity. In particular, the sensitivity of dbPET for early stage breast cancer was higher than that of WBPET/MRI. Kumar et al. [20] showed a sensitivity of 23% for primary breast cancers sized ≤ 10 mm using WBPET. The sensitivity of dbPET for DCIS was reported to be 41–90%, higher than that with WBPET [9, 13, 21]. In this study, the dbPET detection rate for DCIS was 81.8%, which was comparable to that of previous reports. US and MRI are associated with increased sensitivity for high-density breasts and reduced specificity [22]. The high-density breast was also related to the sensitivity of MMG. In this study, 15 lesions (total lesions scanned: 80) were undetected by MMG. In particular, 10 of the 15 lesions could be detected by dbPET. Thus, our findings indicated that dbPET could detect breast cancer that was undetected by MMG screening.
The FDG uptake of dbPET is significantly correlated with pathological and immunohistochemical factors [3,4,5,6,7,8]. In general, ILC shows a lower sensitivity and FDG uptake than IDC on FDG PET or WBPET/CT [3,4,5, 23,24,25]. In this study, two ILC cases were undetected by dbPET. In terms of immunohistology, poor prognostic factors, including a large tumour size (≥ 2 cm), negative ER status, negative PgR status, high Ki67%, and high histological grade, are correlated with high SUVmax [3,4,5,6,7,8]. In this study, the SUVmax of dbPET tended to be significantly higher, with negative ER status, higher grade, and higher Ki67% among the histopathological features. Furthermore, in most studies, triple-negative breast cancer (ER-/HER2-) showed the highest SUVmax compared with the other subtypes [3, 8, 23, 26,27,28,29]. The FDG uptake level is speculated to be one of the prognostic factors. As these results suggest accumulation of FDG as a sensitive biomarker of breast cancer tissue, it is expected to be applied to the evaluation of anticancer drug treatments [30, 31]. Based on these results, dbPET can assist in the detection of early stage breast cancers, systemic or contralateral breast screening, and prognosis prediction.
There is a certain limit to dbPET, depending on the detectable FOV and histopathological factors. The dbPET system takes an image with the patient lying prone with the breasts hanging down. Therefore, the areas near the chest wall tend to become blind areas. The limitation of FOV is attributed to the thickness of the breast and the location of the tumour on the patient’s side [21, 32]. In this study, five tumours were undetected by dbPET, despite detected by WBPET/MRI. It was presumed that the tumours were located outside the FOV. Of the five tumours, four tumours were located in the lateral area, and the BMI of the affected four patients was ≤ 20 kg/m2. We hypothesised that the cause was that the mat was not compressed due to less weight, and the breast could not hang down sufficiently. Therefore, we decided to improve the FOV based on the results.
We reduced the mat thickness of the detector in the middle of this study. First, we replaced the mat of the detector with a removable mat, which was used to relieve pressure and subsequent pain from the edge of the detector. After replacing the initial 20-mm mat with the 5-mm mat, we were able to secure a sufficient imaging range from the retro mammary space (Fig. 2). We also compared the emission scan time of dbPET, which ranged between 3 and 5 min, and confirmed that the detection ability was equivalent. In addition, the imaging range was expanded by adding a slight tilt to the imaging position. Finally, we could shorten the emission scan time and improve the patient position. The pain associated with scanning was also reduced, and the blind area could be further reduced by adjusting the patient position. We restarted the study using the thinner mat. After the improvement of the mat, scan time, and position, no tumour was located outside the FOV.
dbPET can also be used to obtain tomographic images. We demonstrate a case, wherein it was possible to detect the spread of the intraductal breast cancer component, similar to that in MRI (Fig. 3). Thus, there is a possibility that dbPET can be used for screening as well as to evaluate the tumour extent for surgery.
A representative case. a Sagittal MRI image. The contrast-enhanced area showed the spread of the DCIS. b Sagittal dbPET images. These images presented the segmental FDG uptake (SUVmax, 4.08). The FDG uptake areas were similar to the contrast-enhanced area of (a). c Axial WBPET/MR image. The FDG uptake was very weak and, thus, it was difficult to determine the spread of DCIS. d Surgical specimen and pathological result; DCIS with 5- × 2.5-cm size (green-shaded area); ER, 90%; PR, < 5%; HER2, 2+; NG2; Ki67, 20%. MRI, magnetic resonance imaging (MRI); DCIS, ductal carcinoma in situ; dbPET, dedicated breast positron emission tomography; FDG, F-18 fluorodeoxyglucose; SUVmax, maximum standard uptake value; WBPET/MRI, whole-body positron emission tomography/magnetic resonance imaging; ER, oestrogen receptor; PgR, progesterone receptor; HER2, human epidermal growth factor 2; NG, nuclear grade
However, the limitation of this study was that all lesions were diagnosed as breast cancers. We could not demonstrate the specificity of dbPET. Therefore, it is necessary to continue to investigate the specificity of dbPET.
In summary, dbPET could detect early breast cancers, some of which could not be detected on WBPET. Therefore, dbPET can be expected to become one of the preferred breast cancer screening modalities. Moreover, the FDG uptake level on dbPET can reflect the biology of breast cancer.
References
Leong SP, Shen ZZ, Liu TJ, Agarwal G, Tajima T, Paik NS, et al. Is breast cancer the same disease in Asian and Western countries? World J Surg. 2010;34:2308–24. https://doi.org/10.1007/s00268-010-0683-1.
Boyd NF, Martin LJ, Yaffe MJ, Minkin S. Mammographic density and breast cancer risk: current understanding and future prospects. Breast Cancer Res. 2011;13:223. https://doi.org/10.1186/bcr2942.
Heudel P, Cimarelli S, Montella A, Bouteille C, Mognetti T. Value of PET-FDG in primary breast cancer based on histopathological and immunohistochemical prognostic factors. Int J Clin Oncol. 2010;15:588–93. https://doi.org/10.1007/s10147-010-0120-3.
Ugurluer G, Yavuz S, Calikusu Z, Seyrek E, Kibar M, Serin M, et al. Correlation between 18F-FDG positron-emission tomography 18F-FDG uptake levels at diagnosis and histopathologic and immunohistochemical factors in patients with breast cancer. J Breast Health. 2016;12:112–8. https://doi.org/10.5152/tjbh.2016.3031.
Ueda S, Tsuda H, Asakawa H, Shigekawa T, Fukatsu K, Kondo N, et al. Clinicopathological and prognostic relevance of uptake level using 18F-fluorodeoxyglucose positron emission tomography/computed tomography fusion imaging (18F-FDG PET/CT) in primary breast cancer. Jpn J Clin Oncol. 2008;38:250–8. https://doi.org/10.1093/jjco/hyn019.
Lee SJ, Chung MS, Shin SJ, Choi YY. Correlation of tumor uptake on breast-specific gamma imaging and fluorodeoxyglucose PET/CT with molecular subtypes of breast cancer. Medicine (Baltimore). 2018;97: e12840. https://doi.org/10.1097/md.0000000000012840.
Song BI, Hong CM, Lee HJ, Kang S, Jeong SY, Kim HW, et al. Prognostic value of primary tumor uptake on F-18 FDG PET/CT in patients with invasive ductal breast cancer. Nucl Med Mol Imaging. 2011;45:117–24. https://doi.org/10.1007/s13139-011-0081-0.
Jo I, Zeon SK, Kim SH, Kim HW, Kang SH, Kwon SY, et al. Correlation of primary tumor FDG uptake with clinicopathologic prognostic factors in invasive ductal carcinoma of the breast. Nucl Med Mol Imaging. 2015;49:19–25. https://doi.org/10.1007/s13139-014-0296-y.
Berg WA, Madsen KS, Schilling K, Tartar M, Pisano ED, Larsen LH, et al. Breast cancer: comparative effectiveness of positron emission mammography and MR imaging in presurgical planning for the ipsilateral breast. Radiology. 2011;258:59–72. https://doi.org/10.1148/radiol.10100454.
Narayanan D, Madsen KS, Kalinyak JE, Berg WA. Interpretation of positron emission mammography and MRI by experienced breast imaging radiologists: performance and observer reproducibility. AJR Am J Roentgenol. 2011;196:971–81. https://doi.org/10.2214/ajr.10.5081.
Yamamoto Y, Ozawa Y, Kubouchi K, Nakamura S, Nakajima Y, Inoue T. Comparative analysis of imaging sensitivity of positron emission mammography and whole-body PET in relation to tumor size. Clin Nucl Med. 2015;40:21–5. https://doi.org/10.1097/rlu.0000000000000617.
Satoh Y, Kawamoto M, Kubota K, Murakami K, Hosono M, Senda M, et al. Clinical practice guidelines for high-resolution breast PET, 2019 edition. Ann Nucl Med. 2021;35:406–14. https://doi.org/10.1007/s12149-021-01582-y.
Nishimatsu K, Nakamoto Y, Miyake KK, Ishimori T, Kanao S, Toi M, et al. Higher breast cancer conspicuity on dbPET compared to WB-PET/CT. Eur J Radiol. 2017;90:138–45. https://doi.org/10.1016/j.ejrad.2017.02.046.
The Japan Association of Breast and Thyroid Sonology (2014) Guideline for breast ultrasound: management and diagnosis. Revised 3rd ed. NANKODO, Tokyo (in Japanese)
Japan Radiological Society, Japanese Society of Radiological Technology (2014) Mammography guideline, 2nd edn. Igaku-shoin, Tokyo (in Japanese)
American College of Radiology (2014) 2013 ACR Breast imaging reporting and data system Atlas: Breast Imaging Reporting and Data System, 5th edn. VA American College of Radiology, Reston
Allison KH, Hammond MEH, Dowsett M, McKernin SE, Carey LA, Fitzgibbons PL, et al. Estrogen and progesterone receptor testing in breast cancer: ASCO/CAP guideline update. J Clin Oncol. 2020;38:346–66. https://doi.org/10.1200/JCO.19.02309.
Wolff AC, Hammond MEH, Allison KH, Harvey BE, Mangu PB, Bartlett JMS, et al. Human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline focused update. J Clin Oncol. 2018;36:2105–22. https://doi.org/10.1200/JCO.2018.77.8738.
Iima M, Nakamoto Y, Kanao S, Sugie T, Ueno T, Kawada M, et al. Clinical performance of 2 dedicated PET scanners for breast imaging: initial evaluation. J Nucl Med. 2012;53:1534–42. https://doi.org/10.2967/jnumed.111.100958.
Kumar R, Chauhan A, Zhuang H, Chandra P, Schnall M, Alavi A. Clinicopathologic factors associated with false negative FDG-PET in primary breast cancer. Breast Cancer Res Treat. 2006;98:267–74. https://doi.org/10.1007/s10549-006-9159-2.
Sasada S, Masumoto N, Goda N, Kajitani K, Emi A, Kadoya T, et al. Which type of breast cancers is undetectable on ring-type dedicated breast PET? Clin Imaging. 2018;51:186–91. https://doi.org/10.1016/j.clinimag.2018.05.010.
Uematsu T. The need for supplemental breast cancer screening modalities: a perspective of population-based breast cancer screening programs in Japan. Breast Cancer. 2017;24:26–31. https://doi.org/10.1007/s12282-016-0707-2.
Groheux D, Giacchetti S, Moretti JL, Porcher R, Espie M, Lehmann-Che J, et al. Correlation of high 18F-FDG uptake to clinical, pathological and biological prognostic factors in breast cancer. Eur J Nucl Med Mol Imaging. 2011;38:426–35. https://doi.org/10.1007/s00259-010-1640-9.
Fujii T, Yajima R, Kurozumi S, Higuchi T, Obayashi S, Tokiniwa H, et al. Clinical Significance of 18F-FDG-PET in invasive lobular carcinoma. Anticancer Res. 2016;36:5481–5. https://doi.org/10.21873/anticanres.11129.
Gil-Rendo A, Martinez-Regueira F, Zornoza G, Garcia-Velloso MJ, Beorlegui C, Rodriguez-Spiteri N. Association between [18F]fluorodeoxyglucose uptake and prognostic parameters in breast cancer. Br J Surg. 2009;96:166–70. https://doi.org/10.1002/bjs.6459.
Koolen BB, Vrancken Peeters MJ, Wesseling J, Lips EH, Vogel WV, Aukema TS, et al. Association of primary tumour FDG uptake with clinical, histopathological and molecular characteristics in breast cancer patients scheduled for neoadjuvant chemotherapy. Eur J Nucl Med Mol Imaging. 2012;39:1830–8. https://doi.org/10.1007/s00259-012-2211-z.
Sasada S, Masumoto N, Suzuki E, Sueoka S, Goda N, Kajitani K, et al. Prediction of biological characteristics of breast cancer using dual-phase FDG PET/CT. Eur J Nucl Med Mol Imaging. 2019;46:831–7. https://doi.org/10.1007/s00259-019-4259-5.
Garcia Vicente AM, Soriano Castrejon A, Leon Martin A, Chacon Lopez-Muniz I, Munoz Madero V, Munoz Sanchez Mdel M, et al. Molecular subtypes of breast cancer: metabolic correlation with (1)(8)F-FDG PET/CT. Eur J Nucl Med Mol Imaging. 2013;40:1304–11. https://doi.org/10.1007/s00259-013-2418-7.
Kitajima K, Fukushima K, Miyoshi Y, Nishimukai A, Hirota S, Igarashi Y, et al. Association between (1)(8)F-FDG uptake and molecular subtype of breast cancer. Eur J Nucl Med Mol Imaging. 2015;42:1371–7. https://doi.org/10.1007/s00259-015-3070-1.
Sasada S, Masumoto N, Goda N, Kajitani K, Emi A, Kadoya T, et al. Dedicated breast PET for detecting residual disease after neoadjuvant chemotherapy in operable breast cancer: a prospective cohort study. Eur J Surg Oncol. 2018;44:444–8. https://doi.org/10.1016/j.ejso.2018.01.014.
Jones EF, Ray KM, Li W, Seo Y, Franc BL, Chien AJ, et al. Dedicated breast positron emission tomography for the evaluation of early response to neoadjuvant chemotherapy in breast cancer. Clin Breast Cancer. 2017;17:e155–9. https://doi.org/10.1016/j.clbc.2016.12.008.
O’Connor MK, Tran TD, Swanson TN, Ellingson LR, Hunt KN, Whaley DH. Improved visualization of breast tissue on a dedicated breast PET system through ergonomic redesign of the imaging table. EJNMMI Res. 2017;7:100. https://doi.org/10.1186/s13550-017-0351-7.
Acknowledgements
We would like to thank Tokyo Midtown Clinic and Shimadzu Corporation for their assistance with our study.
Funding
This study was supported by Shimadzu Corporation.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Rikako Hashimoto, Sadako Akashi-Tanaka, Chie Watanabe, Hiroko Masuda, Kanae Taruno, Tomoko Takamaru, Yoshimi Ide, and Takashi Kuwayama. The first draft of the manuscript was written by Rikako Hasimoto and all authors commented on the previous versions of the manuscript. All authors read and approved the final manuscript. Conceptualization: Sadako Akashi-Tanaka. Methodology: Sadako Akashi-Tanaka, Rikako Hasimoto. Formal analysis and investigation: Rikako Hasimoto, Chie Watanabe. Writing—original draft preparation: Rikako Hasimoto. Writing—review and editing: Sadako Akashi-Tanaka. Funding acquisition: Sadako Akashi-Tanaka. Resources: Shimadzu Corporation. Supervision: Yasuhiro Kobayashi, Masafumi Takimoto, Seigo Nakamura.
Corresponding author
Ethics declarations
Conflict of interest
The funds for this collaborative research were provided by Shimadzu Corporation. All dedicated breast positron emission tomography and WBPET were scanned free of charge at Midtown Clinic. Sadako Akashi-Tanaka received a research grant from Shimadzu Corporation.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Hashimoto, R., Akashi-Tanaka, S., Watanabe, C. et al. Diagnostic performance of dedicated breast positron emission tomography. Breast Cancer 29, 1013–1021 (2022). https://doi.org/10.1007/s12282-022-01381-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-022-01381-x