Abstract
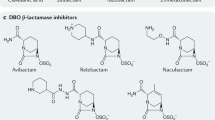
β-Lactam antibiotics are the most commonly prescribed antibiotics worldwide; however, antimicrobial resistance (AMR) is a global challenge. The β-lactam resistance in Gram-negative bacteria is due to the production of β-lactamases, including extended-spectrum β-lactamases, metallo-β-lactamases, and carbapenem-hydrolyzing class D β-lactamases. To restore the efficacy of BLAs, the most successful strategy is to use them in combination with β-lactamase inhibitors (BLI). Here we review the medically relevant β-lactamase families and penicillins, diazabicyclooctanes, boronic acids, and novel chemical scaffold-based BLIs, in particular approved and under clinical development.
Similar content being viewed by others
References
Aboklaish, A.F., Okujava, R., El-Bouseary, M., Zampaloni, C., Najera, I., Bradley, K., Walsh, T.R., and Tyrrell, J.M. 2018. Nacubactam antibacterial activity alone and in combination with β-lactam antibiotics against contemporary Enterobacteriaceae clinical isolates. European Congress of Clinical Microbiology and Infectious Diseases (28th ECCMID) Madrid Spain, Abs. P1034.
Aktaş, Z., Kayacan, C., and Oncul, O. 2012. In vitro activity of avibactam (NXL104) in combination with β-lactams against Gram-negative bacteria, including OXA-48 β-lactamase-producing Klebsiella pneumoniae. Int. J. Antimicrob. Agents39, 86–89.
Alvarez, M., Tran, J.H., Chow, N., and Jacoby, G.A. 2004. Epidemiology of conjugative plasmid-mediated AmpC β-lactamases in the United States. Antimicrob. Agents Chemother.48, 533–537.
Ambler, R.P. 1980. The structure of β-lactamases. Philos. Trans. R. Soc. Lond. B Biol. Sci.289, 321–331.
Bebrone, C. 2007. Metallo-β-lactamases (Classification, activity, genetic organization, structure, Zinc coordination) and their superfamily. Biochem. Pharmacol.74, 1686–1701.
Beck, J., Sauvage, E., Charlier, P., and Marchand-Brynaert, J. 2008. 2-Aminopropane-1, 2, 3-tricarboxylic acid: synthesis and co-crystallization with the class A β-lactamase BS3 of Bacillus licheniformis. Bioorg. Med. Chem. Lett.18, 3764–3768.
Biedenbach, D.J., Kazmierczak, K., Bouchillon, S.K., Sahm, D.F., and Bradford, P.A. 2015. In vitro activity of Aztreonam-Avibactam against a global collection of Gram-negative pathogens from 2012 and 2013. Antimicrob. Agents Chemother.59, 4239–4248.
Bonomo, R.A. and Szabo, D. 2006. Mechanisms of multidrug resistance in Acinetobacter species and Pseudomonas aeruginosa. Clin. Infect. Dis.43, S49–S56.
Brem, J., van Berkel, S.S., Aik, W., Rydzik, A.M., Avison, M.B., Pettinati I., Umland, K.D., Kawamura, A., Spencer, J., Claridge, T.D.W., et al. 2014. Rhodanine hydrolysis leads to potent thioenolate mediated metallo-β-lactamase inhibition. Nat. Chem.6, 1084–1090.
Brem, J., van Berkel, S.S., Zollman, D., Lee, S.Y., Gileadi, O., McHugh, P.J., Walsh, T.R., McDonough, M.A., and Schofield, C.J. 2016. Structural basis of metallo-β-lactamase inhibition by captopril stereoisomers. Antimicrob. Agents Chemother.60, 142–150.
Burns, C.J., Daigle, D., Liu, B., Jackson, R.W., Hamrick, J., McGarry, D., Pevear, D.C., and Trout, R.E.L. 2017. β-Lactamase inhibitors. US Patent 9637504 B2, Venatorx Pharmaceuticals Inc., Philadelphia, USA.
Bush, K. 2018. Past and present perspectives on β-lactamases. Antimicrob. Agents Chemother.62, e01076–18.
Bush, K. and Bradford, P.A. 2019. Interplay between β-lactamases and new β-lactamases inhibitors. Nat. Rev. Microbiol.17, 295–306.
Bush, K. and Jacoby, G.A. 2010. Updated functional classification of β-lactamases. Antimicrob. Agents Chemother.54, 969–976.
Bush, K., Jacoby, G.A., and Medeiros, A.A. 1995. A functional classification scheme for β-lactamases and its correlation with molecular structure. Antimicrob. Agents Chemother.39, 1211–1233.
Bush, K., Macalintal, C., Rasmussen, B.A., Lee, V.J., and Yang, Y. 1993. Kinetic interactions of tazobactam with β-lactamases from all major structural classes. Antimicrob. Agents Chemother.37, 851–858.
Cahill, S.T., Cain, R., Wang, D.Y., Lohans, C.T., Wareham, D.W., Oswin, H.P., Mohammed, J., Spencer, J., Fishwick, C.W.G., Mc-Donough, M.A., et al. 2017. Cyclic boronates inhibit all classes of β-lactamases. Antimicrob. Agents Chemother.61, e02260–16.
Chen, A.Y., Thomas, P.W., Stewart, A.C., Bergstrom, A., Cheng, Z., Miller, C., Bethel, C.R., Marshall, S.H., Credille, C.V., Riley, C.L., et al. 2017. Dipicolinic acid derivatives as inhibitors of New Delhi metallo-β-lactamase-1. J. Med. Chem.60, 7267–7283.
Citron, D.M., Tyrrell, K.L., Merriam, V., and Goldstein, E.J.C. 2011. In vitro activity of Ceftazidime-NXL104 against 396 strains of β-lactamase-producing anaerobes. Antimicrob. Agents Chemother.55, 3616–3620.
Cluck, D., Lewis, P., Stayer, B., Spivey, J., and Moorman, J. 2015. Ceftolozane-tazobactam: a new-generation cephalosporin. Am. J. Health Syst. Pharm.72, 2135–2146.
Coleman, K. 2011. Diazabicyclooctanes (DBOs): a potent new class of non-β-lactam β-lactamase inhibitors. Curr. Opin. Microbiol.14, 550–555.
Day, J.A. and Cohen, S.M. 2013. Investigating the selectivity of metalloenzyme inhibitors. J. Med. Chem.56, 7997–8007.
Dever, L.A. and Dermody, T.S. 1991. Mechanisms of bacterial resistance to antibiotics. Arch. Intern. Med.151, 886–895.
Dhillon, S. 2018. Meropenem/Vaborbactam: a review in complicated urinary tract infections. Drugs78, 1259–1270.
Doi, Y. 2019. Treatment options for carbapenem-resistant Gram-negative bacterial infections. Clin. Infect. Dis.69, S565–S575.
Drawz, S.M., Bethel, C.R., Doppalapudi, V.R., Sheri, A., Pagadala, S.R.R., Hujer, A.M., Skalweit, M.J., Anderson, V.E., Chen, S.G., Buynak, J.D., et al. 2010. Penicillin sulfone inhibitors of class D β-lactamases. Antimicrob. Agents Chemother.54, 1414–1424.
Drawz, S.M. and Bonomo, R.A. 2010. Three decades of β-lactamase inhibitors. Clin. Microbiol. Rev.23, 160–201.
Drawz, S.M., Papp-Wallace, K.M., and Bonomo, R.A. 2014. New β-lactamase inhibitors: a therapeutic renaissance in an MDR world. Antimicrob. Agents Chemother.58, 1835–1846.
Duin, D.V. and Bonomo, R.A. 2016. Ceftazidime/Avibactam and Ceftolozane/Tazobactam: second-generation β-lactam/β-lactamase inhibitor combinations. Clin. Infect. Dis.63, 234–241.
Duin, D.V. and Paterson, D. 2016. Multidrug-resistant bacteria in the community: trends and lessons learned. Infect. Dis. Clin. North Am.30, 377–390.
Durand-Réville, T.F., Guler, S., Comita-Prevoir, J., Chen, B., Bifulco, N., Huynh, H., Lahiri, S., Shapiro, A.B., McLeod, S.M., Carter, N.M., et al. 2017. ETX2514 is a broad-spectrum β-lactamase inhibitor for the treatment of drug-resistant Gram-negative bacteria including Acinetobacter baumannii. Nat. Microbiol.2, 17104.
Ehmann, D.E., Jahic, H., Ross, P.L., Gu, R.F., Hu, J., Durand-Réville, T.F., Lahiri, S., Thresher, J., Livchak, S., Gao, N., et al. 2013. Kinetics of Avibactam inhibition against Class A, C, and D β-lactamases. J. Biol. Chem.288, 27960–27971.
Giacobbe, D.R., Bassetti, M., De Rosa, F.G., Del Bono, V., Grossi, P.A., Menichetti, F., Pea, F., Rossolini, G.M., Tumbarello, M., Viale, P., et al. 2018. Ceftolozane/tazobactam: place in therapy. Expert Rev. Anti. Infext. Ther.16, 307–320.
Gin, A., Dilay, L., Karlowsky, J.A., Walkty, A., Rubinstein, E., and Zhanel, G.G. 2007. Piperacillin-tazobactam: a β-lactam/β-lactamase inhibitor combination. Expert Rev. Anti. Infect. Ther.5, 365–383.
González-Bello, C. 2017. Antibiotic adjuvants-a strategy to unlock bacterial resistance to antibiotics. Bioorg. Med. Chem. Lett.27, 4221–4228.
González-Bello, C., Rodríguez, D., Pernas, M., Rodríguez, A., and Colchón, E. 2020. β-Lactamase inhibitors to restore the efficacy of antibiotics against superbugs. J. Med. Chem.63, 1859–1881.
Gordon, E., Duncton, M., Lal, R., and Trias, J. 2019. Oral prodrugs of avibactam, medicinal chemistry, and synthesis of ARX1796. European Congress of Clinical Microbiology and Infectious Diseases (29th ECCMID), Amsterdam, Netherlands. Poster P1159.
Haider, G., Clancy, C.J., Chen, L., Samanta, P., Shields, R.K., Kreiswirth, B.N., Nguyen, M.H. 2017. Identifying spectra of activity and therapeutic niches for ceftazidime-avibactam and imipenem-relebactam against carbapenem-resistant Enterobacteriaceae. Antimicrob. Agents Chemother.61, e00642–17.
Hecker, S.J., Reddy, R.K., Glinka, T., and Rodny, O. 2020a. Boronic acid derivatives and therapeutic uses thereof. US Patent 1057-0159B2, Qpex Biopharma, Inc., San Diego, USA.
Hecker, S.J., Reddy, R.K., Lomovskaya, O., Griffith, D.C., Rubio-Aparicio, D., Nelson, K., Tsivkovski, R., Sun, D., Sabet, M., Tarazi, Z., et al. 2020b. Discovery of cyclic boronic acid QPX7728, an ultrabroad-spectrum inhibitor of serine and metallo-β-lactamases. J. Med. Chem. DOI: https://doi.org/10.1021/acs.jmedchem.9b01976.
Heinz, U., Bauer, R., Wommer, S., Meyer-Klaucke, W., Papamichaels, C., Bateson, J., and Adolph, H.W. 2003. Coordination geometries of metal ions in D- or L-captopril-inhibited metallo-β-lactamases. J. Biol. Chem.278, 20659–20666.
Higgins, P.G., Wisplinghoff, H., Stefanik, D., and Seifert, H. 2004. In vitro activities of the β-lactamase inhibitors clavulanic acid, sulbactam, and tazobactam alone or in combination with β-lactams against epidemiologically characterized multidrug-resistant Acinetobacter baumannii strains. Antimicrob. Agent Chemother.48, 1586–1592.
Hirsch, E.B., Ledesma, K.R., Chang, K.T., Schwartz, M.S., Motyl, M.R., and Tam, V.H. 2012. In vitro activity of MK-7655, a novel β-lactamase inhibitor, in combination with imipenem against carbapenem-resistant Gram-negative bacteria. Antimicrob. Agents Chemother.56, 3753–3757.
Holten, K.B. and Onusko, E.M. 2000. Appropriate prescribing of oral β-lactam antibiotics. Am. Fam. Physician.62, 611–620.
Iyer, R., Moussa, S.H., Durand-Réville, T.F., Tommasi, R., and Miller, A. 2018. Acinetobacter baumanni OmpA is a selective antibiotic permeant porin. ACS Infect. Dis.4, 373–381.
Jacoby, G.A. 2009. AmpC β-lactamases. Clin. Microbiol. Rev.22, 161–182.
Jones, B.M., Huelfer, K., and Bland, C.M. 2020. Clinical and safety evaluation of continuously infused ceftolozane/tazobactam in the outpatient setting. Open Forum Infect. Dis.7, ofaa014.
June, C.M., Vallier, B.C., Bonomo, R.A., Leonard, D.A., and Powers, R.A. 2014. Structural origins of oxacillinase specificity in class D β-lactamases. Antimicrob. Agents Chemother.58, 333–341.
Kano, A., Koresawa, T., Matsumoto, K., Ouchi, S., and Kondo, K. 2015. First in human study to assess safety, tolerability and pharmacokinetics of β-lactamase inhibitor OP0595. Abstracts of the Twenty-fifth European Congress of Clinical Microbiology and Infectious Diseases, Copenhagen (ESCMID), Basel, Switzerland. Abs. P0236.
Kim, M.K., An, Y.J., Na, J.H., Seol, J.H., Ryu, J.Y., Lee, J.W., Kang, L.W., Chung, K.M., Lee, J.H., Moon, J.H., et al. 2017. Structural and mechanistic insights into the inhibition of class C β-lactamases through the adenylylation of the nucleophilic serine. J. Antimicrob. Chemother. 72, 735–743.
Kim, J.Y., Jung, H.I., An, Y.J., Lee, J.H., Kim, S.J., Jeong, S.H., Lee, K.J., Suh, P.G., Lee, H.S., Lee, S.H., et al. 2006. Structural basis for the extended substrate spectrum of CMY-10, a plasmid-encoded class C β-lactamase. Mol. Microbiol.60, 907–916.
Krajnc, A., Brem, J., Hinchliffe, P., Calvopiña, K., Panduwawala, T.D., Lang, P., Kamps, J.J.A.G., Tyrrell, J.M., Widlake, E., Saward, B.G., et al. 2019. Bicyclic boronate VNRX-5133 inhibits metallo- and serine-β-Lactamase. J. Med. Chem.62, 8544–8556.
Krajnc, A., Lang, P.A., Panduwawala, T.D., Brem, J., and Schofield, C.J. 2019. Will morphing boron-based inhibitors beat the β-lactamases? Curr. Opin. Chem. Biol.50, 101–110.
Liu, B., Trout, R.E.L., Chu, G.H., McGarry, D., Jackson, R.W., Hamrick, J.C., Diagle, D.M., Cusick, S.M., Pozzi, C., de Luca, F., et al. 2020. Discovery of Taniborbactam (VNRX-5133): a broad-spectrum serine- and metallo-β-lactamase inhibitor for carbapenem-resistant bacterial infections. J. Med. Chem.63, 2789–2801.
Livermore, D.M., Mushtaq, S., Warner, M., Vickers, A., and Woodford, N. 2017. In vitro activity of Cefepime/Zidebactam (WCK 5222) against Gram-negative bacteria. J. Antimicrob. Chemother.72, 1373–1385.
Lob, S.H., Hackel, M.A., Kazmierczak, K.M., Young, K., Motyl, M.R., Karlowsky, J.A., and Sahm, D.F. 2017. In vitro activity of imipenem-relebactam against Gram-negative ESKAPE pathogens isolated by clinical laboratories in the United States in 2015 (results from the SMART global surveillance program). Antimicrob. Agents Chemother.61, e02209–16.
Mammeri, H., Poirel, L., and Nordmann, P. 2007. Extension of the hydrolysis spectrum of AmpC β-lactamase of Escherichia coli due to amino acid insertion in the H-10 helix. J. Antimicrob. Chemother.60, 490–494.
McLeod, S., Carter, N., Hackel, M., Badal, R., Mueller, J., Tommasi, R., and Miller, A. 2018. The novel β-lactamase inhibitor ETX1317 effectively restores the activity of cefpodoxime against extended spectrum β-lactamase (ESBL)- and carbapenemase-expressing enterobacteriaceae isolated from recent urinary tract infections. ASM Microbe Atlanta, Georgia, USA. Friday-603.
McLeod, S., Shapiro, A., Moussa, S., Carter, N., Johnstone, M., McLaughlin, R., Dejonge, B., Tommasi, R., Mueller, J., Miller, A. 2016. Sulbactam combined with the novel β-lactamase inhibitor ETX2514 for the treatment of multidrug-resistant Acinetobacter baumannii infections. Open Forum Infect. Dis.3, suppl_1.
Mendes, R.E., Rhomberg, P.R., Watters, A.A., Castanheira, M., and Flamm, R. 2019. In vitro activity of the orally available ceftibuten/VNRX-7145 combination against a challenge set of Enterobacteriaceae pathogens carrying molecularly characterized β-lactamase genes. European Congress of Clinical Microbiology and Infectious Diseases (29th ECCMID), Amsterdam, Netherlands. Abs. P1180.
Morán-Barrio, J., Lisa, M.N., Larrieux, N., Drusin, S.I., Viale, A.M., Moreno, D.M., Buschiazzo, A., and Vila, A.J. 2016. Crystal structure of the metallo-β-lactamase GOB in the periplasmic dizinc form reveals an unusual metal site. Antimicrob. Agents Chemother. 60, 6013–6022.
Morandi, S., Morandi, F., Caselli, E., Shoichet, B.K., and Prati, F. 2008. Structure-based optimization of cephalothin-analogue boronic acids as β-lactamase inhibitors. Bioorg. Med. Chem.16, 1195–1205.
Morinaka, A., Tsutsumi, Y., Yamada, M., Suzuki, K., Watanabe, T., Abe, T., Furuuchi, T., Inamura, S., Sakamaki, Y., Mitsuhashi, N., et al. 2015. OP0595, a new diazabicyclooctane: mode of action as a serine β-lactamase inhibitor, antibiotic and β-lactam ‘Enhancer’. J. Antimicrob. Chemother.70, 2779–2786.
Morrissey, I., Magnet, S., Hawser, S., Shapiro, S., and Knechtle, P. 2019. In vitro activity of cefepime-enmetazobactam against Gram-negative isolates collected from U.S. and European hospitals during 2014–2015. Antimicrob. Agents Chemother.63, e00514–19.
Moya, B., Barcelo, I.M., Bhagwat, S., Patel, M., Bou, G., Papp-Wallace, K.M., Bonomo, R.A., and Oliver, A. 2017a. Potent β-lactam enhancer activity of Zidebactam and WCK 5153 against Acinetobacter baumannii, including carbapenemase-producing clinical isolates. Antimicrob. Agents Chemother.61, e01238–17.
Moya, B., Barcelo, I.M., Bhagwat, S., Patel, M., Bou, G., Papp-Wallace, K.M., Bonomo, R.A., and Oliver, A. 2017b. WCK 5107 (Zidebactam) and WCK 5153 are novel inhibitors of PBP2 showing potent “β-lactam enhancer” activity against Pseudomonas aeruginosa, including multidrug-resistant metallo-β-lactamase-producing high-risk clones. Antimicrob. Agents Chemother.61, e02529–16.
Mushtaq, S., Vickers, A., Woodford, N., and Livermore, D. 2018. Potentiation of cefepime by the boronate VNRX-5133 versus Gram-negative bacteria with known β-lactamases. European Congress of Clinical Microbiology and Infectious Diseases (28th ECCMID), Madrid Spain. Abs. P1536.
Na, J.H., An, Y.J., and Cha, S.S. 2017. GMP and IMP are competitive inhibitors of CMY-10, an extended-spectrum class C β-lactamase. Antimicrob. Agents Chemother. 61, e00098–17.
Na, J.H. and Cha, S.S. 2016. Structural basis for the extended substrate spectrum of AmpC BER and structure-guided discovery of the inhibition activity of citrate against the class C β-lactamases AmpC BER and CMY-10. Acta Cryst. D Struct. Biol.72, 976–985.
Na, J.H., Lee, T.H., Park, S.B., Kim, M.K., Jeong, B.G., Chung, K.M., and Cha, S.S. 2018. In vitro and in vivo inhibitory activity of NADPH against the AmpC BER class C β-lactamase. Front. Cell. Infect. Microbiol.8, 441.
Nordmann, P. and Mammeri, H. 2007. Extended-spectrum cephalosporinases: structure, detection and epidemiology. Future Microbiol.2, 297–307.
O’Donnell, J., Chen, A., Tanudra, A., Mueller, J., Tommasi, R., Miller, A., Carter, N., McLeod, S., Comita-Prevoir, J., and Durand-Réville, T. 2017. Cefpodoxime proxetil/ETX0282: a novel oral β-lactam/β-lactamase inhibitor combination to treat the emerging threat of multi-drug resistant Enterobacteriaceae. ASM Microbe, New Orleans, Louisiana, USA.
Page, M.I. and Badarau, A. 2008. The mechanisms of catalysis by metallo β-lactamases. Bioinorg. Chem. Appl.2008, 576297.
Papp-Wallace, K.M. 2019. The latest advances in β-lactam-β-lactamase inhibitor combinations for the treatment of Gram-negative bacterial infections. Expert Opin. Pharmacother.20, 2169–2184.
Papp-Wallace, K.M., Bethel, C.R., Barnes, M.D., Rutter, J.D., Taracila, M.A., Bajaksouzian, S., Jacobs, M.R., and Bonomo, R.A. 2017. AAI101, a novel β-lactamase inhibitor: microbiological and enzymatic profiling. Open Forum Infect. Dis.4(suppl_1), S375.
Papp-Wallace, K.M., Bethel, C.R., Caillon, J., Barnes, M.D., Potel, G., Bajaksouzian, S., Rutter, J.D., Reghal, A., Shapiro, S., Taracila, M.A., et al. 2019. Beyond piperacillin-tazobactam: cefepime and AAI101 as a potent β-lactam-β-lactamase inhibitor combination. Antimicrob. Agents Chemother.63, e00105–19.
Papp-Wallace, K.M. and Bonomo, R.A. 2016. New β-lactamase inhibitors in the clinic. Infect. Dis. Clin. North Am.30, 441–464.
Papp-Wallace, K.M., Nguyen, N.Q., Jacobs, M.R., Bethel, C.R., Barnes, M.D., Kumar, V., Bajaksouzian, S., Rudin, S.D., Rather, P.N., Bhavsar, S., et al. 2018. Strategic approaches to overcome resistance against Gram-negative pathogens using β-lactamase inhibitors and β-lactam enhancers activity of three novel Diazabicyclooctanes WCK 5153, Zidebactam (WCK 5107), and WCK 4234. J. Med. Chem.61, 4067–4086.
Penwell, W.F., Shapiro, A.B., Giacobbe, R.A., Gu, R.F., Gao, N., Thresher, J., McLaughlin, R.E., Huband, M.D., DeJonge, B.L.M., Ehmann, D.E., et al. 2015. Molecular mechanisms of sulbactam antibacterial activity and resistance determinants in Acinetobacter baumannii. Antimicrob. Agents Chemother.59, 1680–1689.
Perez, F., Hujer, A.M., Hujer, K.M., Decker, B.K., Rather, P.N., and Bonomo, R.A. 2007. Global challenge of multidrug-resistant Acinetobacter baumannii. Antimicrob. Agents Chemother.51, 3471–3484.
Petty, L.A., Henig, O., Patel, T.S., Pogue, J.M., and Kaye, K.S. 2018. Overview of meropenem-vaborbactam and newer antimicrobial agents for the treatment of carbapenem-resistant Enterobacteriaceae. Infect. Drug Resist.11, 1461–1472.
Philippon, A., Arlet, G., and Jacoby, G.A. 2002. Plasmid-determined AmpC-type β-lactamases. Antimicrob. Agents Chemother.46, 1–11.
Philippon, A., Labia, R., and Jacoby, G. 1989. Extended-spectrum β-lactamases. Antimicrob. Agents Chemother.33, 1131–1136.
Pogue, J.M., Kaye, K.S., Cohen, D.A., and Marchaim, D. 2015. Appropriate antimicrobial therapy in the era of multidrug-resistant human pathogens. Clin. Microbiol. Infect.21, 302–312.
Pratt, R.F. 2008. Substrate specificity of bacterial DD-peptidases (penicillin-binding proteins). Cell. Mol. Life Sci.65, 2138–2155.
Qin, W., Panunzio, M., and Biondi, S. 2014. β-Lactam antibiotics renaissance. Antibiotics3, 193–215.
Queenan, A.M. and Bush, K. 2007. Carbapenemases: the versatile β-lactamases. Clin. Microbiol. Rev.20, 440–458.
Rawat, D. and Nair, D. 2010. Extended-spectrum β-lactamases in Gram negative bacteria. J. Glob. Infect. Dis.2, 263–274.
Rice, L.B. 2008. Federal funding for the study of antimicrobial resistance in nosocomial pathogens: No ESKAPE. J. Infect. Dis.197, 1079–1081.
Sader, H.S., Flamm, R.K., Huband, M.D., Rhomberg, P.R., and Castanheira, M. 2017. Antimicrobial activity of meropenem-WCK 4234 (WCK 5999) against clinical isolates of Acinetobacter spp. collected worldwide and stratified by infection type. ASM Microbe, New Orleans, Louisiana, USA.
Sader, H.S., Mendes, R.E., Pfaller, M.A., Shortridge, D., Flamm, R.K., and Castanheira, M. 2018. Antimicrobial activities of aztreonam-avibactam and comparator agents against contemporary (2016) clinical Enterobacteriaceae isolates. Antimicrob. Agents Chemother.62, e01856–17.
Santajit, S. and Indrawattana, N. 2016. Mechanisms of antimicrobial resistance in ESKAPE pathogens. Biomed Res. Int.2016, 2475067.
Santillana, E., Beceiro, A., Bou, G., and Romero, A. 2007. Crystal structure of the carbapenemase OXA-24 reveals insights into the mechanism of carbapenem hydrolysis. Proc. Natl. Acad. Sci. USA104, 5354–5359.
Schultsz, C. and Geerlings, S. 2012. Plasmid-mediated resistance in Enterobacteriaceae: changing landscape and implications for therapy. Drugs72, 1–16.
Schwarz, S., Loeffler, A., and Kadlec, K. 2017. Bacterial resistance to antimicrobial agents and its impact on veterinary and human medicine. Vet. Dermatol.28, 82–e19.
Shrivastava, S.M., Kumar, S., and Chaudhary, M. 2009. Ceftriaxone-sulbactam combination: microbial analysis by variation of ratios and comparative disc diffusion. Curr. Res. Bacteriol.2, 50–55.
Smet, A., Martel, A., Persoons, D., Dewulf, J., Heyndrickx, M., Herman, L., Haesebrouck, F., and Butaye, P. 2010. Broad-spectrum β-lactamases among Enterobacteriaceae of animal origin: molecular aspects, mobility and impact on public health. FEMS Microbiol. Rev.34, 295–316.
Spicer, T., Minond, D., Enogieru, I., Saldanha, S.A., Allais, C., Liu, Q., Mercer, B.A., Roush, W.R., and Hodder, P. 2014. ML302, a novel β-lactamase (BLA) inhibitor. In Probe Reports from the NIH Molecular Libraries Program [Internet]. National Center for Biotechnology Information (US).
Stachyra, T., Péchereau, M.C., Bruneau, J.M., Claudon, M., Frere, J.M., Miossec, C., Coleman, K., and Black, M.T. 2010. Mechanistic studies of the inactivation of TEM-1 and P99 by NXL104, a novel non-β-lactam β-lactamase inhibitor. Antimicrob. Agents Chemother. 54, 5132–5138.
Takeda, S., Ishii, Y., Hatano, K., Tateda, K., and Yamaguchi, K. 2007. Stability of FR264205 against AmpC β-lactamase of Pseudomonas aeruginosa. Int. J. Antimicrob. Agents.30, 443–445.
Tehrani, K.H.M.E. and Martin, N.I. 2018. β-lactam/β-lactamase inhibitor combinations: an update. Medchemcomm.9, 1439–1456.
Testa, R., Cantón, R., Giani, T., Morosini, M.I., Nichols, W.W., Seifert, H., Stefanik, D., Rossolini, G.M., and Nordmann, P. 2015. In vitro activity of ceftazidime, ceftaroline and aztreonam alone and in combination with avibactam against european Gram-negative and Gram-positive clinical isolates. Int. J. Antimicrob. Agents.45, 641–646.
Therrien, C. and Levesque, R.C. 2000. Molecular basis of antibiotic resistance and β-lactamase inhibition by mechanism-based inactivators: perspectives and future directions. FEMS Microbiol. Rev.24, 251–262.
Theuretzbacher, U., Bush, K., Harbarth, S., Paul, M., Rex, J.H., Tacconelli, E., and Thwaites, G.E. 2020. Critical analysis of antibacterial agents in clinical development. Nat. Rev. Microbiol.18, 286–298.
Toney, J.H., Hammond, G.G., Fitzgerald, P.M., Sharma, N., Balkovec, J.M., Rouen, G.P., Olson, S.H., Hammond, M.L., Greenlee M.L., and Gao, Y.D. 2001. Succinic acids as potent inhibitors of plasmid-borne IMP-1 metallo-β-lactamase. J. Biol. Chem.276, 31913–31918.
Tsivkovski, R., Totrov, M., Lomovskaya, O. 2020. Biochemical characterization of QP7728, a new ultrabroad-spectrum β-lactamase inhibitor of serine and metallo-β-lactamases. Antimicrob. Agents Chemother.64, e00130–20.
Tyers, M. and Wright, G.D. 2019. Drug combinations: a strategy to extend the life of antibiotics in the 21st century. Nat. Rev. Microbiol.17, 141–155.
Typas, A., Banzhaf, M., Gross, C.A., and Vollmer, W. 2011. From the regulation of peptidoglycan synthesis to bacterial growth and morphology. Nat. Rev. Microbiol.10, 123–136.
Wang, D.Y., Abboud, M.I., Markoulides, M.S., Brem, J., and Schofield, C.J. 2016. The road to avibactam: the first clinically useful non-β-lactam working somewhat like a β-lactam. Future Med. Chem.8, 1063–1084.
Wang, Y., Wang, J., Wang, R., and Cai, Y. 2020. Resistance to ceftazidime-avibactam and underlying mechanisms. J. Glob. Antimicrob. Resist.22, 18–27.
Yusof, Y., Tan, D.T.C., Arjomandi, O.K., Schenk, G., and McGeary, R.P. 2016. Captopril analogues as metallo-β-lactamase inhibitors. Bioorg. Med. Chem. Lett.26, 1589–1593.
Zervosen, A., Sauvage, E., Frère, J.M., Charlier, P., and Luxen, A. 2012. Development of new drugs for an old target-the penicillin binding proteins. Molecules17, 12478–12505.
Zhanel, G.G., Lawson, C.D., Adam, H., Schweizer, F., Zelenitsky, S., Lagacé-Wiens, R.S., Denisuik, A., Gin, A.S., Hoban, D.J., Lynch, J.P., et al. 2013. Ceftazidime-avibactam: a novel cephalosporin/β-lactamase inhibitor combination. Drugs73, 159–177.
Acknowledgments
This work was supported by Jungwon University Research Grant (2017-022).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Jalde, S.S., Choi, H.K. Recent advances in the development of β-lactamase inhibitors. J Microbiol. 58, 633–647 (2020). https://doi.org/10.1007/s12275-020-0285-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12275-020-0285-z