Abstract
Background
Nasointestinal decompression was implemented into clinical practice in 1930s. Earlier clinical trials have confirmed the efficacy of nasointestinal tubes in treating adhesive small bowel obstructions. A recent study showed controversial results: efficacy after nasogastric intervention was not less efficient compared to nasointestinal decompression. Hydrophilic silicon triple lumen tubes used for intestinal decompression were introduced in 2003. A variety of modifications were introduced and applied in clinical practice. Our study attempts to compare the decompression efficacy between the modern ileus tube and nasogastric tubes used for decompression in patients with malignant bowel obstruction.
Methods
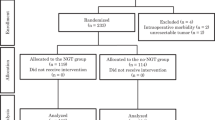
A total of 132 consecutive patients with intestinal obstruction were included in this study. There was no significant difference between the two groups with regard to clinical characteristics and laboratory variables documented on admission. The endoscopically inserted intestinal tube was used for gastrointestinal decompression in 64 patients, and nasogastric tube was applied in 68 patients. The therapeutic efficacy of applied strategies was compared between the two groups using Chi-squared test.
Results
Compared with the strategy applying nasogastric tubes, the group of patients treated with intestinal tube showed significantly shorter time for surgical rehabilitation (4.8 ± 2.2 d vs 9.6 ± 4.8 d). Significant difference was registered in laboratory test results (P < 0.01). In the study group, the output of drainage and the length of hospital stay were significantly shorter compared to the control (P < 0.05).
Conclusion
Nasointestinal decompression used in the surgical management of small intestinal obstruction with malignancy has significantly higher efficacy compared to nasogastric decompression.


Similar content being viewed by others
References
Eren T, Boluk S, Bayraktar B, Ozemir IA, Yildirim Boluk S, Tombalak E, Alimoglu O (2015) Surgical indicators for the operative treatment of acute mechanical intestinal obstruction due to adhesions. Ann Surg Treat Res 88(6):325–333
Sazhin AV, Tyagunov AE, Larichev SE, Lebedev IS, Makhuova GB, Marchenko IP, Polushkin VG, Tyagunov AA, Sazhin IV, Nechay TV, Ivakhov GB, Titkova SM, Anurov MV, Gasanov MM, Kolygin AV, Mirzoyan AT, Glagolev NS, Kurashinova LS. (2018) Optimal time of surgery for acute adhesive small bowel obstruction]. Khirurgiia (Mosk) (3):24-30
Hort A, Hameed A, Middleton PG, Pleass HC (2019, 2019) Distal intestinal obstruction syndrome: an important differential diagnosis for abdominal pain in patients with cystic fibrosis. ANZ J Surg. https://doi.org/10.1111/ans.15357
Mohanty D, Garg PK, Kumar A, Jain BK (2014) Abdominal lump with intestinal obstruction: prior history of abdominal surgery is a clue to diagnosis. Ann Afr Med 13(2):95–96
Bento JH, Bianchi ET, Tustumi F, Leonardi PC, Junior UR, Ceconello I (2019) Surgical management of malignant intestinal obstruction: outcome and prognostic factors. Chirurgia (Bucur) 114(3):343–351
Mu JF, Wang Q, Wang SD, Wang C, Song JX, Jiang J, Cao XY (2018) Clinical factors associated with intestinal strangulating obstruction and recurrence in adhesive small bowel obstruction: a retrospective study of 288 cases. Medicine (Baltimore) 97(34):e12011
Timofeev ME, Larichev SE, Fedorov ED, Polushkin VG, Shapoval'iants SG. (2015) Laparoscopic diagnosis and treatment of acute early adhesive intestinal obstruction. Khirurgiia (Mosk) (8):46-53
Demetrashvili ZM (2012) Cholelythic intestinal obstruction. Surgery. 3:65–68
de Li C, Li RH, Tian Q (2016) Efficacy of intestinal decompression with long nasointestinal tube and selective contrast radiography in the treatment of small bowel obstruction in elderly patients. Minerva Chir 71(2):85–90
Pedersen KS, Raghav K, Overman MJ (2019) Small bowel adenocarcinoma: etiology, presentation, and molecular alterations. J Natl Compr Cancer Netw 17(9):1135–1141
Nutu OA, Marcacuzco Quinto AA, Jiménez Romero LC (2017) Primary malignant tumors of the small intestine: a retrospective analysis of 15 years experience. Med Clin (Barc) 149(3):129–130
Scélo G, Boffetta P, Hemminki K, Pukkala E, Olsen JH, Andersen A, Tracey E, Brewster DH, McBride ML, Kliewer EV, Tonita JM, Pompe-Kirn V, Chia KS, Jonasson JG, Martos C, Colin D, Brennan P (2006) Associations between small intestine cancer and other primary cancers: an international population-based study. Int J Cancer 118(1):189–196
Pujara D, Chiang YJ, Cormier JN, Bruera E, Badgwell B (2017) Selective approach for patients with advanced malignancy and gastrointestinal obstruction. J Am Coll Surg 225(1):53–59
Levin AL (1921) A new gastroduodenal catheter. JAMA 76:1007–1009
Wangensteen OH, Paine JR (1933) Treatment of acute intestinal obstruction by suction with the duodenal tube. JAMA 101:1532–1539
Ullah MA, Rahman MA, Chowdhury LH, Mohammed S, Hasan MI (2017) Outcome of upper gastrointestinal surgery with or without nasogastric intubation. Mymensingh Med J 26(3):650–657
Macarone Palmieri R, Amodio PM, Rizzello M, Goglia A, Piciollo M, Piccioni E, Guglielmelli P, Rubino F (2012) Does the nasogastric tube has a role in elective colo-rectal surgery? G Chir 33(3):58–61
Karakonstantis S, Kalemaki D (2018) Symptomatic relief as an outcome in studies of nasogastric decompression in small bowel obstruction. Am J Emerg Med 36(6):1109–1110
Tavassoli A, Rajabi MT, Abdollahi A, Bagheri R, Noorshafiee S (2011) Efficacy and necessity of nasojejunal tube after gastrectomy. Int J Surg 9(3):233–236
VijayGanapathy S, Karthikeyan VS, Mallya A, Poonawala A, Keshavamurthy R (2018) Nasogastric tube as abdominal pressure sensor in urodynamics-proof of concept of a novel approach. Neurourol Urodyn 37(2):785–791
Kunstman JW, Klemen ND, Fonseca AL, Araya DL, Salem RR (2013) Nasogastric drainage may be unnecessary after pancreaticoduodenectomy: a comparison of routine vs selective decompression. J Am Coll Surg 217(3):481–488
Mangano A, Marciano L (2018) One-day nasogastric tube decompression after distal gastrectomy: a prospective randomized study. Surg Today 48(1):127
Glasheen WP, Cordier T, Gumpina R, Haugh G, Davis J, Renda A (2019) Charlson comorbidity index: ICD-9 update and ICD-10 translation. Am Health Drug Benefits 12(4):188–197
Soloviov IE (2000) Modified system of SAPS Модифицированная система SAPS for the evaluation of patients with acute malignant intestinal obstruction. Oncology 3:204–206
Karadeli E, Erbay G, Parlakgumus A, Yabanoglu H (2017) Abdominal CT findings in patients with primary lymphoma causing small bowel obstruction. J Coll Physicians Surg Pak 27(11):711–713
Uludag M, Agkun I, Yetkin G et al (2004) Factors affecting morbidity and mortality in mechanical intestinal obstruction. Ulus Trauma Derg 10:177–184
Thompson WM, Kilani RK, Smit BB et al (2007) Accuracy of abdominal radiography in acute small bowel obstruction: does reviewer experience matter? AJR Am J Roetgenol 188(33):233–238
Ullah S, Khan M (2008) Intestinal obstruction: a spectrum of causes, Department of Surgery, postgraduate medical institute Lady Reading hospital, Peshawar Pakistan. JPMI. 8(1):210–213
Bolliger M, Kroehnert JA, Molineus F, Kandioler D, Schindl M, Riss P (2018) Experiences with the standardized classification of surgical complications (Clavien-Dindo) in general surgery patients. Eur Surg 50(6):256–261
Pan SY, Morrison H (2011) Epidemiology of cancer of the small intestine. World J Gastrointest Oncol 3(3):33–42
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
The study was approved by the YSMU research ethics committee.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mirijanyan, A.A., Grigoryan, K.H. & Mirijanyan, M.M. Comparative Analysis of Efficacy of Intraoperative Decompression with Nasogastric and Nasojejunal Tubes in Patients with Malignant Small Bowel Obstruction. Indian J Surg 82, 656–661 (2020). https://doi.org/10.1007/s12262-020-02091-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-020-02091-4