Abstract
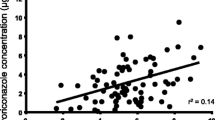
We investigated the role of therapeutic dose monitoring (TDM) in the treatment of fungal infections with voriconazole through 49 analyses of 34 patients who received treatment for hematologic diseases. Voriconazole concentration was highly variable among patients regardless of renal, liver functions, or age, and the effect of dose enhancement was not constant. This indicates the difficulty of predicting voriconazole concentration without TDM. We evaluated the outcome with the composite assessment system where patients were assumed non-responders when they failed to show improvement in at least 2 of the following 3 criteria: clinical, radiologic, and mycologic. We showed that concentration–response relationship depended on the status of underlying hematologic diseases; this relationship was observed only in cases without refractory hematologic diseases, but not in those with refractory diseases. In the former group, cases with >2 mg/L of concentration were associated with good response to voriconazole. On the other hand, elevation of hepatic enzyme was frequently observed when voriconazole concentration was >6 mg/L. From these results, we concluded that TDM should be executed and targeted to 2–6 mg/L to improve efficacy and to avoid side effects.





Similar content being viewed by others
References
Patterson TF, Kirkpatrick WR, White M, et al. Invasive aspergillosis. Disease spectrum, treatment practices, and outcomes. I3 Aspergillus study group. Medicine (Baltimore). 2000;79:250–60. doi:10.1097/00005792-200007000-00006.
Hachem R, Hanna H, Kontoyiannis D, Jiang Y, Raad I. The changing epidemiology of invasive candidiasis: Candida glabrata and Candida krusei as the leading causes of candidemia in hematologic malignancy. Cancer. 2008;112:2493–9. doi:10.1002/cncr.23466.
Chamilos G, Luna M, Lewis RE, et al. Invasive fungal infections in patients with hematologic malignancies in a tertiary care cancer center: an autopsy study over a 15-year period (1989–2003). Haematologica. 2006;91:986–9.
Herbrecht R, Denning DW, Patterson TF, et al. Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med. 2002;347:408–15. doi:10.1056/NEJMoa020191.
Perfect JR, Marr KA, Walsh TJ, et al. Voriconazole treatment for less-common, emerging, or refractory fungal infections. Clin Infect Dis. 2003;36:1122–31. doi:10.1086/374557.
Powers JH, Dixon CA, Goldberger MJ. Voriconazole versus liposomal amphotericin B in patients with neutropenia and persistent fever. N Engl J Med. 2002;346:289–90. doi:10.1056/NEJM200201243460414.
Purkins L, Wood N, Ghahramani P, Greenhalgh K, Allen MJ, Kleinermans D. Pharmacokinetics and safety of voriconazole following intravenous- to oral-dose escalation regimens. Antimicrob Agents Chemother. 2002;46:2546–53. doi:10.1128/AAC.46.8.2546-2553.2002.
Dodds Ashley ESLR, Lewis JS, Martin C, Andes D. Pharmacology of systemic antifungal agents. Clin Infect Dis. 2006;43:28–39. doi:10.1086/504492.
Geist MJ, Egerer G, Burhenne J, Mikus G. Safety of voriconazole in a patient with CYP2C9*2/CYP2C9*2 genotype. Antimicrob Agents Chemother. 2006;50:3227–8. doi:10.1128/AAC.00551-06.
Murayama N, Imai N, Nakane T, Shimizu M, Yamazaki H. Roles of CYP3A4 and CYP2C19 in methyl hydroxylated and N-oxidized metabolite formation from voriconazole, a new anti-fungal agent, in human liver microsomes. Biochem Pharmacol. 2007;73:2020–6. doi:10.1016/j.bcp.2007.03.012.
Shimizu T, Ochiai H, Asell F, et al. Bioinformatics research on inter-racial difference in drug metabolism I. Analysis on frequencies of mutant alleles and poor metabolizers on CYP2D6 and CYP2C19. Drug Metab Pharmacokinet. 2003;18:48–70. doi:10.2133/dmpk.18.48.
Smith J, Safdar N, Knasinski V, et al. Voriconazole therapeutic drug monitoring. Antimicrob Agents Chemother. 2006;50:1570–2. doi:10.1128/AAC.50.4.1570-1572.2006.
Pascual A, Calandra T, Bolay S, Buclin T, Bille J, Marchetti O. Voriconazole therapeutic drug monitoring in patients with invasive mycoses improves efficacy and safety outcomes. Clin Infect Dis. 2008;46:201–11. doi:10.1086/524669.
Juweid ME, Stroobants S, Hoekstra OS, et al. Use of positron emission tomography for response assessment of lymphoma: consensus of the Imaging Subcommittee of International Harmonization Project in Lymphoma. J Clin Oncol. 2007;25:571–8. doi:10.1200/JCO.2006.08.2305.
De Pauw B, Walsh TJ, Donnelly JP, et al. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis. 2008;46:1813–21. doi:10.1086/588660.
Kawazu M, Kanda Y, Nannya Y, et al. Prospective comparison of the diagnostic potential of real-time PCR, double-sandwich enzyme-linked immunosorbent assay for galactomannan, and a (1→3)-beta-d-glucan test in weekly screening for invasive aspergillosis in patients with hematological disorders. J Clin Microbiol. 2004;42:2733–41. doi:10.1128/JCM.42.6.2733-2741.2004.
Marr KA, Balajee SA, McLaughlin L, Tabouret M, Bentsen C, Walsh TJ. Detection of galactomannan antigenemia by enzyme immunoassay for the diagnosis of invasive aspergillosis: variables that affect performance. J Infect Dis. 2004;190:641–9. doi:10.1086/422009.
Greene RE, Schlamm HT, Oestmann JW, et al. Imaging findings in acute invasive pulmonary aspergillosis: clinical significance of the halo sign. Clin Infect Dis. 2007;44:373–9. doi:10.1086/509917.
Pascual A, Nieth V, Calandra T, et al. Variability of voriconazole plasma levels measured by new high-performance liquid chromatography and bioassay methods. Antimicrob Agents Chemother. 2007;51:137–43. doi:10.1128/AAC.00957-06.
Almyroudis NG, Kontoyiannis DP, Sepkowitz KA, DePauw BE, Walsh TJ, Segal BH. Issues related to the design and interpretation of clinical trials of salvage therapy for invasive mold infection. Clin Infect Dis. 2006;43:1449–55. doi:10.1086/508455.
National Cancer institute. Serious adverse events definitions. In Edition National Cancer Institute 2006.
Nivoix Y, Leveque D, Herbrecht R, Koffel JC, Beretz L, Ubeaud-Sequier G. The enzymatic basis of drug-drug interactions with systemic triazole antifungals. Clin Pharmacokinet. 2008;47:779–92. doi:10.2165/0003088-200847120-00003.
Perea JR, Diaz De Rada BS, Quetglas EG, Juarez MJ. Oral versus intravenous therapy in the treatment of systemic mycosis. Clin Microbiol Infect. 2004;10(Suppl 1):96–106. doi:10.1111/j.1470-9465.2004.00846.x.
Caillot D, Couaillier JF, Bernard A, et al. Increasing volume and changing characteristics of invasive pulmonary aspergillosis on sequential thoracic computed tomography scans in patients with neutropenia. J Clin Oncol. 2001;19:253–9.
Miceli MH, Maertens J, Buve K, et al. Immune reconstitution inflammatory syndrome in cancer patients with pulmonary aspergillosis recovering from neutropenia: Proof of principle, description, and clinical and research implications. Cancer. 2007;110:112–20. doi:10.1002/cncr.22738.
Obayashi T, Yoshida M, Tamura H, Aketagawa J, Tanaka S, Kawai T. Determination of plasma (1→3)-beta-d-glucan: a new diagnostic aid to deep mycosis. J Med Vet Mycol. 1992;30:275–80. doi:10.1080/02681219280000361.
Mennink-Kersten MA, Warris A, Verweij PE. 1,3-beta-d-glucan in patients receiving intravenous amoxicillin-clavulanic acid. N Engl J Med. 2006;354:2834–5. doi:10.1056/NEJMc053340.
Sulahian A, Touratier S, Ribaud P. False positive test for aspergillus antigenemia related to concomitant administration of piperacillin and tazobactam. N Engl J Med. 2003;349:2366–7. doi:10.1056/NEJM200312113492424.
Imhof A, Schaer DJ, Schanz U, Schwarz U. Neurological adverse events to voriconazole: evidence for therapeutic drug monitoring. Swiss Med Wkly. 2006;136:739–42.
Acknowledgments
We appreciate agency of Pfizer Japan Inc. and TSL Inc. for measuring voriconazole concentrations. We declare that we have no competing interests.
Conflict of interest statement
The authors do not have any conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Ueda, K., Nannya, Y., Kumano, K. et al. Monitoring trough concentration of voriconazole is important to ensure successful antifungal therapy and to avoid hepatic damage in patients with hematological disorders. Int J Hematol 89, 592–599 (2009). https://doi.org/10.1007/s12185-009-0296-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-009-0296-3