Abstract
Purpose of Review
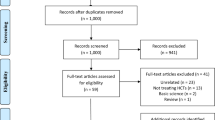
The lateral meniscus oblique radial tear (LMORT) of the posterior horn is a relatively new term for one of the more common types of lateral meniscal tears found in patients with acute anterior cruciate ligament (ACL) injuries. Given the importance of anatomical reduction and preservation of the lateral meniscus to maintain normal knee stability and slow the progression of early-onset osteoarthritis, LMORT classification and treatment guidelines have been formulated. This article provides a review of the prevalence, classification, biomechanics, surgical repair techniques, and outcomes related to LMORT injuries.
Recent Findings
Current research demonstrates favorable clinical results when LMORTs are surgically treated based on recent evidence. Biomechanically, repair of the higher grade 3 and 4 LMORT lesions have led to comparable results when compared to an intact lateral meniscus, and superior results when compared to partial meniscectomy and untreated tears. Ongoing research is aimed to determine the difference between LMORT repairs compared to intact lateral menisci at the time of ACL surgery regarding comparable patient outcomes.
Summary
LMORT lesions are common tears of the lateral meniscus that should be treated surgically based on tear type at the time of ACL surgery. The benefit of doing so has already been demonstrated biomechanically.











Similar content being viewed by others
Data Availability
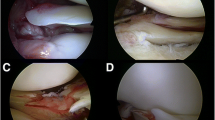
The Intraoperative arthroscopic images in figures 1-5 and 7-11are not publicly available in order to protect the patients' privacy; additionally, the data in tables 1-3 was retrieved from our institution's registry and may be available upon request.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Borchers JR, Kaeding CC, Pedroza AD, et al. Intra-articular findings in primary and revision anterior cruciate ligament reconstruction surgery: a comparison of the MOON and MARS study groups. Am J Sports Med. 2011;39(9):1889–93. https://doi.org/10.1177/0363546511406871.
Mansori AE, Lording T, Schneider A, Dumas R, Servien E, Lustig S. Incidence and patterns of meniscal tears accompanying the anterior cruciate ligament injury: possible local and generalized risk factors. Int Orthop. 2018;42(9):2113–21. https://doi.org/10.1007/s00264-018-3992-x.
Praz C, Vieira TD, Saithna A, et al. Risk Factors for lateral meniscus posterior root tears in the anterior cruciate ligament-injured knee: an epidemiological analysis of 3956 patients from the SANTI Study Group. Am J Sports Med. 2019;47(3):598–605. https://doi.org/10.1177/0363546518818820.
Feucht MJ, Bigdon S, Bode G, et al. Associated tears of the lateral meniscus in anterior cruciate ligament injuries: risk factors for different tear patterns. J Orthop Surg Res. 2015;10:34. https://doi.org/10.1186/s13018-015-0184-x. (Published 2015 Mar 18).
Forkel P, Reuter S, Sprenker F, et al. Different patterns of lateral meniscus root tears in ACL injuries: application of a differentiated classification system. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):112–8. https://doi.org/10.1007/s00167-014-3467-6.
Shelbourne KD, Roberson TA, Gray T. Long-term evaluation of posterior lateral meniscus root tears left in situ at the time of anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39(7):1439–43. https://doi.org/10.1177/0363546511398212.
Westermann RW, Wright RW, Spindler KP, Huston LJ, MOON Knee Group, Wolf BR. Meniscal repair with concurrent anterior cruciate ligament reconstruction: operative success and patient outcomes at 6-year follow-up. Am J Sports Med. 2014;42(9):2184–92. https://doi.org/10.1177/0363546514536022.
Wilson PL, Wyatt CW, Romero J, Sabatino MJ, Ellis HB. Incidence, presentation, and treatment of pediatric and adolescent meniscal root injuries. Orthop J Sports Med. 2018;6(11):2325967118803888. https://doi.org/10.1177/2325967118803888. (Published 2018 Nov 8).
•• Krych AJ, LaPrade MD, Cook CS, et al. Lateral meniscal oblique radial tears are common with acl injury: a classification system based on arthroscopic tear patterns in 600 consecutive patients. Orthop J Sports Med. 2020;8(5):2325967120921737. https://doi.org/10.1177/2325967120921737. (Published 2020 May 19). Explanation: This was the original study where the classification and prevalence of the LMORT lesion was first introduced.
LaPrade CM, James EW, Cram TR, Feagin JA, Engebretsen L, LaPrade RF. Meniscal root tears: a classification system based on tear morphology. Am J Sports Med. 2015;43(2):363–9. https://doi.org/10.1177/0363546514559684.
Thaunat M, Fayard JM, Guimaraes TM, Jan N, Murphy CG, Sonnery-Cottet B. Classification and surgical repair of ramp lesions of the medial meniscus. Arthrosc Tech. 2016;5(4):e871–5. https://doi.org/10.1016/j.eats.2016.04.009. (Published 2016 Aug 8).
• Smith PA, Bezold WA, Cook CR, et al. Kinematic analysis of lateral meniscal oblique radial tears in the anterior cruciate ligament-deficient knee. Am J Sports Med. 2021;49(14):3898–905. https://doi.org/10.1177/03635465211052521. Explanation: This was the first of the 2 LMORT biomechanical studies highlighting the increased anterior translation and meniscal extrusion associated with the LMORT lesion compared to an isolated ACL injury with an intact lateral meniscus.
• Smith PA, Bezold WA, Cook CR, et al. Kinematic analysis of lateral meniscal oblique radial tears in anterior cruciate ligament-reconstructed knees: untreated versus repair versus partial meniscectomy. Am J Sports Med. 2022;50(9):2381–9. https://doi.org/10.1177/03635465221102135. Explanation: this was the second of the 2 LMORT biomechanical studies highlighting the restoration of knee stability with LMORT type 3 and 4 repair to levels comparable to an intact meniscus. It is also highlighted the residual anterior translation and meniscus extrusion associated with leaving a higher grade LMORT lesion in situ or treating it with a partial meniscectomy at the time of ACLR.
• Jeon YS, Alsomali K, Yang SW, Lee OJ, Kang B, Wang JH. Posterior horn lateral meniscal oblique radial tear in acute anterior cruciate ligament reconstruction incidence and outcomes after all-inside repair: clinical and second-look arthroscopic evaluation. Am J Sports Med. 2022;50(14):3796–804. https://doi.org/10.1177/03635465221126506. Explanation: this was a second large LMORT study detailing the prevalence of the different LMORT lesions in consecutive patients who underwent ACLR. Additionally, a large percentage of the LMORT patients underwent a second-look arthroscopic procedure which demonstrated good healing potential of these lesions.
Weber J, Koch M, Angele P, Zellner J. The role of meniscal repair for prevention of early onset of osteoarthritis. J Exp Orthop. 2018;5(1):10. https://doi.org/10.1186/s40634-018-0122-z. (Published 2018 Apr 2).
Patil SS, Shekhar A, Tapasvi SR. Meniscal preservation is important for the knee joint. Indian J Orthop. 2017;51(5):576–87. https://doi.org/10.4103/ortho.IJOrtho_247_17.
Shimomura K, Hamamoto S, Hart DA, Yoshikawa H, Nakamura N. Meniscal repair and regeneration: current strategies and future perspectives [published correction appears in J Clin Orthop Trauma. 2020 Nov-Dec;11(6):1169-1171]. J Clin Orthop Trauma. 2018;9(3):247–53. https://doi.org/10.1016/j.jcot.2018.07.008.
Ohori T, Mae T, Shino K, et al. Different effects of the lateral meniscus complete radial tear on the load distribution and transmission functions depending on the tear site. Knee Surg Sports Traumatol Arthrosc. 2021;29(2):342–51. https://doi.org/10.1007/s00167-020-05915-8.
Uffmann W, ElAttrache N, Nelson T, et al. Posterior lateral meniscal root tears increase strain on the reconstructed anterior cruciate ligament: a cadaveric study. Arthrosc Sports Med Rehabil. 2021;3(2):e505–13. https://doi.org/10.1016/j.asmr.2020.11.005. (Published 2021 Feb 3).
Yagishita K, Muneta T, Ogiuchi T, Sekiya I, Shinomiya K. Healing potential of meniscal tears without repair in knees with anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32(8):1953–61. https://doi.org/10.1177/0363546504263702.
Pujol N, Beaufils P. Healing results of meniscal tears left in situ during anterior cruciate ligament reconstruction: a review of clinical studies. Knee Surg Sports Traumatol Arthrosc. 2009;17(4):396–401. https://doi.org/10.1007/s00167-008-0711-y.
Doral MN, Bilge O, Huri G, Turhan E, Verdonk R. Modern treatment of meniscal tears. EFORT Open Rev. 2018;3(5):260–8. https://doi.org/10.1302/2058-5241.3.170067. (Published 2018 May 21).
Golz AG, Mandelbaum B, Pace JL. All-inside meniscus repair. Curr Rev Musculoskelet Med. 2022;15(4):252–8. https://doi.org/10.1007/s12178-022-09766-3.
Höher J, Münster A, Klein J, Eypasch E, Tiling T. Validation and application of a subjective knee questionnaire. Knee Surg Sports Traumatol Arthrosc. 1995;3(1):26–33. https://doi.org/10.1007/BF01553522.
Shelbourne KD, Barnes AF, Gray T. Correlation of a single assessment numeric evaluation (SANE) rating with modified Cincinnati knee rating system and IKDC subjective total scores for patients after ACL reconstruction or knee arthroscopy. Am J Sports Med. 2012;40(11):2487–91. https://doi.org/10.1177/0363546512458576.
Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)–development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28(2):88–96. https://doi.org/10.2519/jospt.1998.28.2.88.
Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10(3):150–4. https://doi.org/10.1177/036354658201000306.
Greco NJ, Anderson AF, Mann BJ, et al. Responsiveness of the International Knee Documentation Committee Subjective Knee Form in comparison to the Western Ontario and McMaster Universities Osteoarthritis Index, modified Cincinnati Knee Rating System, and Short Form 36 in patients with focal articular cartilage defects. Am J Sports Med. 2010;38(5):891–902. https://doi.org/10.1177/0363546509354163.
Beletsky A, Naami E, Lu Y, et al. The minimally clinically important difference and substantial clinical benefit in anterior cruciate ligament reconstruction: a time-to-achievement analysis. Orthopedics. 2021;44(5):299–305. https://doi.org/10.3928/01477447-20210819-03.
Muller B, Yabroudi MA, Lynch A, et al. Defining thresholds for the patient acceptable symptom state for the IKDC subjective knee form and KOOS for patients who underwent ACL reconstruction. Am J Sports Med. 2016;44(11):2820–6. https://doi.org/10.1177/0363546516652888.
• Zhuo H, Chen Q, Zhu F, Li J. Arthroscopic side-to-side repair for complete radial posterior lateral meniscus root tears. BMC Musculoskelet Disord. 2020;21(1):130. https://doi.org/10.1186/s12891-020-3156-1. Explanation: demonstrated great healing potential for LMORT-like lesions when surgically repaired using an all-inside spanning suture repair. Additionally, the cohort in this series demonstrated satisfactory PROs following their procedure.
• Tsujii A, Yonetani Y, Kinugasa K, Matsuo T, Yoneda K, Ohori T, Hamada M. Outcomes more than 2 years after meniscal repair for radial/flap tears of the posterior lateral meniscus combined with anterior cruciate ligament reconstruction. Am J Sports Med. 2019;47(12):2888–94. https://doi.org/10.1177/0363546519869955. Explanation: This study demonstrated that patients with LMORT-like lesions had comparable postoperative PROMs when compared to those patients who underwent iACLR.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All patients signed an informed consent to be enrolled in our institution’s registry (Surgical Outcomes System [SOS]; Arthrex, Naples, FL) under the protection of the Salus IRB (Protocol: SOS #1).
Conflict of Interest
Adam V. Daniel, MD declares that he has no conflict of interest.
Aaron J. Krych, MD has received consulting fees from Arthrex, JRF, Vericel, and Responsive Arthroscopy; royalties from Arthrex and Responsive Arthroscopy; grants from DJO and Exatech; and research support from Aesculap/B.Braun, Ceterix, and Histogenics.
Patrick A. Smith, MD has received consulting fees and royalties from Arthrex; compensation for services other than consulting from Alpha Orthopedic Systems and Medical Device Business Services; support for education from Elite Orthopedics; and hospitality payments from Sanofi-Aventis, Davol Inc, Flexion Therapeutics, Scilex Pharmaceuticals, DePuy Synthes Sales, Lilly, Novartis Pharmaceuticals, and Breg.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Daniel, A.V., Krych, A.J. & Smith, P.A. The Lateral Meniscus Oblique Radial Tear (LMORT). Curr Rev Musculoskelet Med 16, 306–315 (2023). https://doi.org/10.1007/s12178-023-09835-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12178-023-09835-1