Abstract
Purpose of Review
Anterior cruciate ligament (ACL) rupture is a common injury that has important clinical and economic implications. We aimed to review the literature to identify gender, racial and ethnic disparities in incidence, treatment, and outcomes of ACL injury.
Recent Findings
Females are at increased risk for ACL injury compared to males. Intrinsic differences such as increased quadriceps angle and increased posterior tibial slope may be contributing factors. Despite lower rates of injury, males undergo ACL reconstruction (ACLR) more frequently. There is conflicting evidence regarding gender differences in graft failure and ACL revision rates, but males demonstrate higher return to sport (RTS) rates. Females report worse functional outcome scores and have worse biomechanical metrics following ACLR. Direct evidence of racial and ethnic disparities is limited, but present. White athletes have greater risk of ACL injury compared to Black athletes. Non-White and Spanish-speaking patients are less likely to undergo ACLR after ACL tear. Black and Hispanic youth have greater surgical delay to ACLR, increased risk for loss to clinical follow-up, and less physical therapy sessions, thereby leading to greater deficits in knee extensor strength during rehabilitation. Hispanic and Black patients also have greater risk for hospital admission after ACLR, though this disparity is improving.
Summary
Females have higher rates of ACL injury with inconclusive evidence on anatomic predisposition and ACL failure rate differences between genders. Recent literature has suggested inferior RTS and functional outcomes following ACLR in females. Though there is limited and mixed data on incidence and outcome differences between races and ethnic groups, recent studies suggest there may be disparities in those who undergo ACLR and time to treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Differences in race, ethnicity, gender, and socioeconomic status within the diverse population of the USA have led to the permeation of disparities across many different specialties in medicine and surgery [1,2,3]. Within orthopedic surgery in particular, disparities in utilization, selection, treatment, and outcomes have been shown in multiple subspecialties [4,5,6,7,8,9]. Here, we review the existing evidence in the literature pertaining to disparities in anterior cruciate ligament (ACL) injury, management, and outcomes. ACL injury is the most common isolated ligamentous injury that occurs in athletes, with over 100,000 ACL reconstructions performed per year and over three billion dollars in estimated costs annually in the USA alone [10,11,12,13]. The profound clinical and economic impact of ACL injuries highlights the importance of understanding and addressing disparities that exist to ensure adequate patient care.
Gender Disparity in ACL Injury, Treatment, and Outcomes
Compared to male counterparts within the same sport, it has been well established that female athletes are two to eight times more likely to sustain an ACL injury [14,15,16]. With the increase in participation in youth athletics as well as expansion of women’s collegiate and professional programs over the last few decades [17], it has become increasingly important to better understand potential mechanisms underlying the gender difference in injury rates.
Intrinsic Risk Factors and Predisposition to Injury
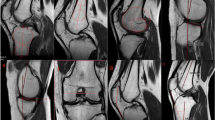
Anatomic variation in the femoral intercondylar notch (ICN) has been studied as a possible intrinsic risk factor contributing to the discrepancy in ACL injury between male and female athletes. Notch width index (NWI) is a measure that attempts to standardize notch width relative to overall distal femoral width and is commonly used to define the size of the ICN. Compared to males, females have smaller NWI and smaller standardized ACL cross-sectional area [18, 19]. While ICN stenosis has been shown to be associated with an increased risk of noncontact ACL injury [20], there is conflicting data surrounding the significance of NWI differences between males and females in the context of ACL injury [21,22,23]. A study of 108 ACL injury radiographs compared to controls showed a higher proportion of A-shaped notches (notch narrows from base to midsection and apex) in females relative to males; however, notch shape and sex did not correlate with injury status [24]. Similarly, there have been conflicting findings regarding the association of notch size and ACL size [22, 25]. In summary, there appears to be a difference in ICN size and ACL size between genders without conclusive correlation to injury (Table 1).
Recently, much emphasis has been placed on the geometry of the knee, specifically the quadriceps angle (Q angle) and posterior tibial slope (PTS). The Q angle has been shown to be up to 5.8° greater in females compared to that in males leading to a more laterally directed pull of the quadriceps, which may place the ACL at higher risk for injury [18, 26]. It is widely accepted that an increase in PTS places the tibia more anterior relative to the femur during quadriceps contraction, which may result in increased strain on the ACL. This has been supported by multiple studies that have demonstrated increased risk of ACL injuries in those with higher PTS.
Hohmann et al. found that PTS of the medial plateau was higher in ACL-injured females than males [27]. Similarly, Terauchi et al. found that medial plateau PTS was significantly greater in the ACL-deficient females compared to controls, whereas no significant difference was seen between the injured and control male groups [28]. In contrast, multiple studies have noted no significant difference in PTS measurements between men and women with ACL injury [29, 30]. Given the mixed results when comparing gender, it may be that the risk for ACL injury in relation to PTS is associated with a particular threshold measure rather than sex.
Estrogen, progesterone, and androgen receptors have been localized to fibroblasts and endothelial cells within the ACL, thereby suggesting a hormonal influence on susceptibility to ACL injury [31, 32]. A meta-analysis found that anterior knee laxity was greater in the ovulatory phase than in the luteal phase and lowest in the follicular phase [33]. Interestingly, ACL injury is more likely to occur in the early and late follicular phases [34, 35]. There is a lack of large-scale studies that compare hormone levels, markers of laxity, and injury between genders. Thus, the current data is insufficient to make any conclusive statement regarding the influence of hormonal and menstrual cycles on the rate of ACL injury in females.
Biomechanical and kinematic factors have also been extensively studied as possible explanations to gender differences in ACL injury. Females have a higher quadriceps-to-hamstring mass ratio and a higher ratio of quadriceps-to-hamstring recruitment [36]. Furthermore, females have been noted to land in a more erect posture with an external rotation position [19]. These factors have been theorized to increase the stress on the ACL. Females have also been shown to have higher recruitment of lateral thigh musculature and to consequently have up to a 2.5 times greater knee abduction moment [37]. While this has not been directly linked to ACL injury, these abduction moment differences arise after pubertal growth spurts around the time which the disproportionate increase in female injury rates occurs [38].
Ultimately, many physiologic, biomechanical, and kinematic differences have been established that may explain differences in ACL injury rates between males and females, which as it stands appears to be a multifactorial phenomenon.
Treatment
Over the past few decades, there has been a significant increase in the rates of ACLR among both men and women in the USA and internationally [39,40,41]. A 2017 study showed that females aged 13–17 had the highest rate of ACLR, more than any other sex-age strata [42]. Despite higher rates of primary injury in female athletes, males have been reported to undergo ACLR more frequently [43, 44]. However, there has been an increase in the proportion of females undergoing ACLR compared to males in both ambulatory and inpatient settings [45]. Additionally, graft choice has previously been thought to be influenced by gender, with females more likely to receive an allograft as opposed to autograft revision ACLR [46]. However, Svantesson et al. subsequently reported no gender difference with graft choice in primary ACLR [47].
Outcomes
Currently, there exists conflicting evidence regarding differences in graft failure between genders. While females have been shown to have greater laxity on post-operative physical exam [48], a multitude of studies have shown no significant difference in graft rupture/failure rates [49,50,51,52,53,54]. On the contrary, other studies have identified male sex as a risk factor for ipsilateral revision and graft failure following primary ACLR [55, 56]. Risk for contralateral ACLR also has conflicting evidence, with some studies identifying female sex as a risk factor [57,58,59], and others showing no significant difference between male and female patients [60, 61].
Another primary outcome of interest specifically in athletes that undergo ACLR is the overall time to return to sport (RTS). Young, male athletes have significantly higher RTS rates compared to female athletes at 12 months post primary ACLR (differences summarized in Table 2) [62, 63•]. One potential explanation is that male patients have been shown to have greater psychological readiness to RTS throughout the entire rehabilitation process compared to females [64, 65, 66•] and self-reported psychological readiness has been identified as the most significant factor in predicting subsequent return to comparable athletic performance [67]. This implies a potential role for psychological treatment as part of the post-ACLR rehabilitation programs and a need to further understand RTS protocols for athletes.
In the current literature, male patients have superior functional outcomes following primary ACLR. Data from the Swedish knee ligament registry shows favorable outcomes for males for the Knee Injury and Osteoarthritis Outcome (KOOS) score and EuroQol EQ-5D health status measure [68]. Similar findings have been documented with self-reported knee questionnaires [69, 70]. Furthermore, male patients who return to work and drive sooner have greater odds of participating in moderate-to-vigorous physical activity after ACLR [71, 72].
In addition to RTS and functional outcomes, post-operative biomechanical testing also favors males. In both animal and human studies, females have decreased knee extensor muscle strength compared to males at 1 year after surgery, and slower rates of quadriceps torque development in the affected limb [73, 74•, 75,76,77]. Female athletes with ACLR also display worse Landing Error Scoring System (LESS) scores and are more likely than males to commit errors related to medial knee displacement during landing movement patterns [78]. The overall discrepancy in outcomes between genders, specifically for primary ACLR, highlights the importance of personalized rehabilitation protocols and further level I studies to elucidate the important modifiable risk factors both pre- and post-operatively.
Disparities in Race and Ethnicity
Predisposition to Injury
Anatomic variation in femoral ICN has been studied within patients of different races and ethnicities as a possible risk factor for ACL injury. Compared with African American males, Caucasian males consistently have narrower ICN width; however, there is conflicting evidence surrounding females of various races, with some studies showing significant differences between African American and White females, and others showing no difference [79, 80]. Additionally, no significant anatomic discrepancy has been identified in Q angle or PTS between White and African patients [81, 82]. Injury trends within the Women’s National Basketball Association (WNBA) help illustrate potential disparities by race, with White athletes having more than 6 times the ACL tear rate of other ethnic groups combined [83]. Data of Han Chinese patients with ACL injuries shows a higher proportion of patients with a small tibial footprint size compared to Western populations with ACL injuries, suggesting differences in tibial footprint size could play a role between races [84, 85]. There is a paucity of studies and limited data on racial and ethnic predisposition to ACL injury despite well-described anatomic differences.
Treatment
Race and ethnicity have been shown to influence treatment following ACL injury. White patients are more likely than non-White patients to undergo ACLR after ACL injury diagnosis [86]. Language similarly influences rates of ACLR, as patients that speak English as a primary language are most likely to undergo surgical reconstruction, followed by multilanguage households, while exclusively Spanish-speaking patients are significantly less likely to undergo reconstruction [86]. Among pediatric and adolescent populations, Black and Hispanic patients experience greater surgical delays after ACL rupture [87••]. In the Kaiser Permanente ACL registry data, when controlling for insurance status, Asian, Hispanic, and Black patients were less likely to undergo elective ACL revision compared to White patients, despite having comparable access to care through Kaiser [88••]. Race distribution was significantly different across graft types used in the Kaiser data, with a lower proportion of White patients in the bone-tendon-bone (BTB) autograft group compared to the hamstring autograft or allograft groups [89]. Black high school and collegiate athletes are more likely to receive a BTB versus hamstring autograft [90]. In the post-operative period, Black and other non-White races have significantly increased risk of loss to clinical follow-up [91]. Additionally, young Black and Hispanic athletes also have less physical therapy sessions during the rehabilitation process, highlighting further racial disparity in ACL treatment [87••].
Outcomes
There is limited and mixed evidence on the influence of race and ethnicity on post-operative complications following ACLR. Some studies have shown that White patients have a significantly higher risk than Hispanic, Asian, and Black patients for ipsilateral revision and contralateral ACLR [92,93,94] while others have found no difference in ipsilateral revision rates between races [87••, 95]. Hispanic ethnicity [96] and Black race [97] have been identified as risk factors for post-operative readmission following ACLR. However, between 2007 and 2015, readmission rates of Black and Hispanic patients have been decreasing relative to that of White patients [98•].
There is limited and thus inconclusive data for disparities in RTS and biomechanical testing. A study of 915 pediatric primary ACLRs showed no difference in RTS clearance by race, though Black and Hispanic patients were significantly less likely to be cleared to RTS overall [87••]. Another study did not find a significant difference between White and non-White patients in RTS rates at 2-year follow-up [99]. Isokinetic dynamometer testing has shown that Black and Hispanic pediatric and adolescent patients experience significantly greater quadriceps deficits at 6 and 9 months following ACLR, likely due in part to a discrepancy in physical therapy follow-up [87••]. Overall, while the studies are limited, racial and ethnic disparities exist in treatment and outcome and this is likely multifactorial, but implies the presence of biases that require further investigation.
Where Do We Go from Here?
Gender differences are evident and call for gender-specific studies in order to better understand injury and pathophysiology and close the gap in outcomes between males and females. Given the much higher incidence of ACL injury in females, there is a demand for more studies focusing on injury prevention such as neuromuscular and proprioceptive training. Special attention is needed for young female athletes as the number of sports programs continues to increase. There is a paucity of literature on high-performance female athletes compared to available data for male athletes [100]. Limited understanding of differences in anatomy, physiology, and biomechanics along with applying male-dominant research to all is likely contributing to the inferior outcomes reported among females.
Health care providers across all specialties including orthopedic surgery show implicit biases related to race and gender, similar to those of the general public [101, 102]. Druckman et al. analyzed how sports medical staff responded to student-athlete case vignettes and showed that staff viewed Black athletes as having higher initial pain tolerance after ACL tear compared to their White peers [103]. While such biases have not been directly shown to effect outcomes, it is likely a contributory factor that has to be addressed at the individual level. Providers must make an effort to take into consideration not only race and gender, but also important social determinants of health, access to care, and patient expectations all of which can have a large impact on patient outcomes.
Lastly, it has been well documented that patient satisfaction and health outcomes are favorable when there is racial, ethnic, and linguistic concordance between the physician and patient [104,105,106]). Within orthopedic surgery residency programs, between 2006 and 2015, female representation increased from 10.9 to 14.4%, but this rate of increase was significantly lower than those of many other surgical specialties. Additionally, there was no significant improvement in racial/ethnic diversity among orthopedic residency programs over the same time period [107•]. A recent study similarly showed that Latino, African American, and Native American groups were significantly underrepresented in orthopedic residencies [108]. A more representative workforce from surgeon to physical therapists to athletic trainers may have a positive impact on disparities and treatment outcomes.
Conclusion
There is broad evidence of disparities surrounding the incidence, treatment, and outcomes following ACL injury. Disproportionate rates of injury, anatomic differences, variable biomechanics, access to care, and implicit biases among other factors must be considered. While there is evidence of improvement in certain areas, we still have work to do to close the gap and optimize care for all.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Howell EA. Reducing disparities in severe maternal morbidity and mortality. Clin Obstet Gynecol [Internet]. 2018;61:387–99. Available from: https://journals.lww.com/00003081-201806000-00022
Bonds DE, Zaccaro DJ, Karter AJ, Selby JV, Saad M, Goff DC. Ethnic and racial differences in diabetes care: The Insulin Resistance Atherosclerosis Study. Diabetes Care [Internet]. 2003;26:1040–6. https://doi.org/10.2337/diacare.26.4.1040.
Haider AH, Scott VK, Rehman KA, Velopulos C, Bentley JM, Cornwell EE, et al. Racial disparities in surgical care and outcomes in the United States: a comprehensive review of patient, provider, and systemic factors. J Am Coll Surg [Internet]. 2013;216:482–492.e12. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1072751512013798
Skinner J, Weinstein JN, Sporer SM, Wennberg JE. Racial, ethnic, and geographic disparities in rates of knee arthroplasty among Medicare patients. N Engl J Med [Internet]. 2003;349:1350–9. https://doi.org/10.1056/NEJMsa021569.
Hawkins K, Escoto KH, Ozminkowski RJ, Bhattarai GR, Migliori RJ, Yeh CS. Disparities in major joint replacement surgery among adults with Medicare supplement insurance. Popul Health Manag [Internet]. 2011;14:231–8. https://doi.org/10.1089/pop.2010.0042.
Bass AR, McHugh K, Fields K, Goto R, Parks ML, Goodman SM. Higher total knee arthroplasty revision rates among United States Blacks than Whites. J Bone Jt Surg [Internet]. 2016;98:2103–8. Available from: http://journals.lww.com/00004623-201612210-00010
Sanford Z, Taylor H, Fiorentino A, Broda A, Zaidi A, Turcotte J, Patton C. Racial disparities in surgical outcomes after spine surgery: an ACS-NSQIP analysis. Glob Spine J [Internet]. 2019;9:583–90. https://doi.org/10.1177/2192568218811633.
Singh JA, Ramachandran R. Racial disparities in total ankle arthroplasty utilization and outcomes. Arthritis Res Ther [Internet]. 2015;17:70. Available from: http://arthritis-research.com/content/17/1/70
Singh JA, Ramachandran R. Persisting racial disparities in total shoulder arthroplasty utilization and outcomes. J Racial Ethn Heal Disparities [Internet]. 2016;3:259–66. https://doi.org/10.1007/s40615-015-0138-3.
Kaeding CC, Léger-St-Jean B, Magnussen RA. Epidemiology and diagnosis of anterior cruciate ligament injuries. Clin Sports Med [Internet]. 2017;36:1–8. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0278591916300722
Beynnon BD, Johnson RJ, Abate JA, Fleming BC, Nichols CE. Treatment of anterior cruciate ligament injuries. Part I. Am J Sports Med [Internet]. 2005;33:1579–602. https://doi.org/10.1177/0363546505279913.
Beynnon BD, Johnson RJ, Abate JA, Fleming BC, Nichols CE. Treatment of anterior cruciate ligament injuries, Part 2. Am J Sports Med [Internet]. 2005;33:1751–67. https://doi.org/10.1177/0363546505279922.
Hewett TE, Myer GD, Ford KR, Paterno MV, Quatman CE. Mechanisms, prediction, and prevention of ACL injuries: cut risk with three sharpened and validated tools. J Orthop Res [Internet]. 2016;34:1843–55. https://doi.org/10.1002/jor.23414.
Agel J, Rockwood T, Klossner D. Collegiate ACL injury rates across 15 sports. Clin J Sport Med [Internet]. 2016;26:518–23. Available from: http://journals.lww.com/00042752-201611000-00011
Hewett TE, Ford KR, Myer GD. Anterior cruciate ligament injuries in female athletes. Am J Sports Med [Internet]. 2006;34:490–8. https://doi.org/10.1177/0363546505282619.
Arendt E, Dick R. Knee injury patterns among men and women in collegiate basketball and soccer. Am J Sports Med [Internet]. 1995;23:694–701. https://doi.org/10.1177/036354659502300611.
Stracciolini A, Amar-Dolan L, Howell DR, Alex T, Berkner P, Sandstrom NJ, et al. Female sport participation effect on long-term health-related quality of life. Clin J Sport Med [Internet]. 2018; Publish Ah. Available from: https://journals.lww.com/00042752-900000000-99150
Giugliano DN, Solomon JL. ACL tears in female athletes. Phys Med Rehabil Clin N Am [Internet]. 2007;18:417–38. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1047965107000459
Sutton KM, Bullock JM. Anterior cruciate ligament rupture: differences between males and females. J Am Acad Orthop Surg [Internet]. 2013;21:41–50. https://doi.org/10.5435/JAAOS-21-01-41.
LaPrade RF, Burnett QM. Femoral intercondylar notch stenosis and correlation to anterior cruciate ligament injuries. Am J Sports Med [Internet]. 1994;22:198–203. https://doi.org/10.1177/036354659402200208.
Bayer S, Meredith SJ, Wilson KW, de SA D, Pauyo T, Byrne K, et al. Knee morphological risk factors for anterior cruciate ligament injury. J Bone Jt Surg [Internet]. 2020;102:703–18. https://doi.org/10.2106/JBJS.19.00535.
Anderson AF, Dome DC, Gautam S, Awh MH, Rennirt GW. Correlation of anthropometric measurements, strength, anterior cruciate ligament size, and intercondylar notch characteristics to sex differences in anterior cruciate ligament tear rates. Am J Sports Med [Internet]. 2001;29:58–66. https://doi.org/10.1177/03635465010290011501.
Rosenberg TD, Paulos LE, Parker RD, Coward DB, Scott SM. The forty-five-degree posteroanterior flexion weight-bearing radiograph of the knee. J Bone Jt Surg [Internet]. 1988;70:1479–83. Available from: http://journals.lww.com/00004623-198870100-00006
Ireland ML, Ballantyne BT, Little K, McClay IS. A radiographic analysis of the relationship between the size and shape of the intercondylar notch and anterior cruciate ligament injury. Knee Surgery, Sport Traumatol Arthrosc [Internet]. 2001;9:200–5. https://doi.org/10.1007/s001670100197.
Dienst M, Schneider G, Altmeyer K, Voelkering K, Georg T, Kramann B, Kohn D. Correlation of intercondylar notch cross sections to the ACL size: a high resolution MR tomographic in vivo analysis. Arch Orthop Trauma Surg [Internet]. 2007;127:253–60. https://doi.org/10.1007/s00402-006-0177-7.
Conley S, Rosenberg A, Crowninshield R. The female knee: anatomic variations. J Am Acad Orthop Surg [Internet]. 2007;15:S31–6. Available from: http://journals.lww.com/00124635-200700001-00009
Hohmann E, Bryant A, Reaburn P, Tetsworth K. Is there a correlation between posterior tibial slope and non-contact anterior cruciate ligament injuries? Knee Surgery. Sport Traumatol Arthrosc [Internet]. 2011;19:109–14. https://doi.org/10.1007/s00167-011-1547-4.
Liu SH, Al-Shaikh R, Panossian V, Yang R-S, Nelson SD, Soleiman N, et al. Primary immunolocalization of estrogen and progesterone target cells in the human anterior cruciate ligament. J Orthop Res [Internet]. 1996;14:526–33. https://doi.org/10.1002/jor.1100140405.
Todd MS, Lalliss S, Garcia E, DeBerardino TM, Cameron KL. The relationship between posterior tibial slope and anterior cruciate ligament injuries. Am J Sports Med [Internet]. 2010;38:63–7. https://doi.org/10.1177/0363546509343198.
Hashemi J, Chandrashekar N, Mansouri H, Gill B, Slauterbeck JR, Schutt RC, et al. Shallow medial tibial plateau and steep medial and lateral tibial slopes: new risk factors for anterior cruciate ligament injuries. Am J Sports Med [Internet]. 2010;38:54–62. https://doi.org/10.1177/0363546509349055.
Liu SH, Al-Shaikh R, Panossian V, Yang RS, Nelson SD, Soleiman N, et al. Primary immunolocalization of estrogen and progesterone target cells in the human anterior cruciate ligament. J Orthop Res. 1996;14(4):526–33.
Hamlet WP, Liu SH, Panossian V, Finerman GAM. Primary immunolocalization of androgen target cells in the human anterior cruciate ligament. J Orthop Res [Internet]. 1997;15:657–63. https://doi.org/10.1002/jor.1100150505.
Zazulak BT, Paterno M, Myer GD, Romani WA, Hewett TE. The effects of the menstrual cycle on anterior knee laxity. Sport Med [Internet]. 2006;36:847–62. https://doi.org/10.2165/00007256-200636100-00004.
Beynnon BD, Johnson RJ, Braun S, Sargent M, Bernstein IM, Skelly JM, Vacek PM. The relationship between menstrual cycle phase and anterior cruciate ligament injury. Am J Sports Med [Internet]. 2006;34:757–64. https://doi.org/10.1177/0363546505282624.
Griffin LY, Albohm MJ, Arendt EA, Bahr R, Beynnon BD, DeMaio M, Dick RW, Engebretsen L, Garrett WE, Hannafin JA, Hewett TE, Huston LJ, Ireland ML, Johnson RJ, Lephart S, Mandelbaum BR, Mann BJ, Marks PH, Marshall SW, et al. Understanding and preventing noncontact anterior cruciate ligament injuries. Am J Sports Med [Internet]. 2006;34:1512–32. https://doi.org/10.1177/0363546506286866.
Hewett TE. A review of electromyographic activation levels, timing differences, and increased anterior cruciate ligament injury incidence in female athletes. Br J Sports Med [Internet]. 2005;39:347–50. https://doi.org/10.1136/bjsm.2005.018572.
Hewett TE, Myer GD, Ford KR, Heidt RS, Colosimo AJ, McLean SG, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med [Internet]. 2005;33:492–501. https://doi.org/10.1177/0363546504269591.
Ford KR, Shapiro R, Myer GD, van den Bogert AJ, Hewett TE. Longitudinal sex differences during landing in knee abduction in young athletes. Med Sci Sport Exerc [Internet]. 2010;42:1923–31. Available from: http://journals.lww.com/00005768-201010000-00016
Sanders TL, Maradit Kremers H, Bryan AJ, Larson DR, Dahm DL, Levy BA, Stuart MJ, Krych AJ. Incidence of anterior cruciate ligament tears and reconstruction. Am J Sports Med [Internet]. 2016;44:1502–7. https://doi.org/10.1177/0363546516629944.
Zbrojkiewicz D, Vertullo C, Grayson JE. Increasing rates of anterior cruciate ligament reconstruction in young Australians, 2000–2015. Med J Aust [Internet]. 2018;208:354–8. https://doi.org/10.5694/mja17.00974.
Abram SGF, Price AJ, Judge A, Beard DJ. Anterior cruciate ligament (ACL) reconstruction and meniscal repair rates have both increased in the past 20 years in England: hospital statistics from 1997 to 2017. Br J Sports Med [Internet]. 2020;54:286–91. https://doi.org/10.1136/bjsports-2018-100195.
Herzog MM, Marshall SW, Lund JL, Pate V, Mack CD, Spang JT. Incidence of anterior cruciate ligament reconstruction among adolescent females in the United States, 2002 through 2014. JAMA Pediatr [Internet]. 2017;171:808. https://doi.org/10.1001/jamapediatrics.2017.0740.
Herzog MM, Marshall SW, Lund JL, Pate V, Mack CD, Spang JT. Trends in incidence of ACL reconstruction and concomitant procedures among commercially insured individuals in the United States, 2002-2014. Sport Heal A Multidiscip Approach [Internet]. 2018;10:523–31. https://doi.org/10.1177/1941738118803616.
Gans I, Retzky JS, Jones LC, Tanaka MJ. Epidemiology of recurrent anterior cruciate ligament injuries in National Collegiate Athletic Association sports: the Injury Surveillance Program, 2004-2014. Orthop J Sport Med [Internet]. 2018;6:232596711877782. https://doi.org/10.1177/2325967118777823.
Buller LT, Best MJ, Baraga MG, Kaplan LD. Trends in anterior cruciate ligament reconstruction in the United States. Orthop J Sport Med [Internet]. 2015;3:232596711456366. https://doi.org/10.1177/2325967114563664.
Group M. Factors influencing graft choice in revision anterior cruciate ligament reconstruction in the MARS group. J Knee Surg [Internet]. 2015;29:458–63. https://doi.org/10.1055/s-0035-1564723.
Svantesson E, Hamrin Senorski E, Baldari A, Ayeni OR, Engebretsen L, Franceschi F, et al. Factors associated with additional anterior cruciate ligament reconstruction and register comparison: a systematic review on the Scandinavian knee ligament registers. Br J Sports Med [Internet]. 2019;53:418–25. https://doi.org/10.1136/bjsports-2017-098192.
Tan SHS, Lau BPH, Khin LW, Lingaraj K. The importance of patient sex in the outcomes of anterior cruciate ligament reconstructions. Am J Sports Med [Internet]. 2016;44:242–54. https://doi.org/10.1177/0363546515573008.
Ryan J, Magnussen RA, Cox CL, Hurbanek JG, Flanigan DC, Kaeding CC. ACL reconstruction. J Bone Jt Surg [Internet]. 2014;96:507–12. Available from: http://journals.lww.com/00004623-201403190-00011
Thaunat M, Clowez G, Saithna A, Cavalier M, Choudja E, Vieira TD, et al. Reoperation rates after combined anterior cruciate ligament and anterolateral ligament reconstruction: a series of 548 patients from the SANTI study group with a minimum follow-up of 2 years. Am J Sports Med [Internet]. 2017;45:2569–77. https://doi.org/10.1177/0363546517708982.
Thaunat M, Clowez G, Saithna A, Cavalier M, Choudja E, Vieira TD, Fayard JM, Sonnery-Cottet B. Reoperation rates after combined anterior cruciate ligament and anterolateral ligament reconstruction: a series of 548 patients from the SANTI study group with a minimum follow-up of 2 years. Am J Sports Med. 2017;45:2569–77.
Samitier G, Marcano AI, Alentorn-Geli E, Cugat R, Farmer KW, Moser MW. Failure of anterior cruciate ligament reconstruction. Arch bone Jt Surg [Internet]. 2015;3:220–40. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26550585
Ponce B, Cain E, Pflugner R, Fleisig G, Young B, Boohaker H, et al. Risk factors for revision anterior cruciate ligament reconstruction. J Knee Surg [Internet]. 2015;29:329–36. https://doi.org/10.1055/s-0035-1554925.
Persson A, Fjeldsgaard K, Gjertsen J-E, Kjellsen AB, Engebretsen L, Hole RM, et al. Increased risk of revision with hamstring tendon grafts compared with patellar tendon grafts after anterior cruciate ligament reconstruction. Am J Sports Med [Internet]. 2014;42:285–91. https://doi.org/10.1177/0363546513511419.
Rahardja R, Zhu M, Love H, Clatworthy MG, Monk AP, Young SW. Rates of revision and surgeon-reported graft rupture following ACL reconstruction: early results from the New Zealand ACL Registry. Knee Surgery, Sport Traumatol Arthrosc [Internet]. 2020;28:2194–202. https://doi.org/10.1007/s00167-019-05773-z.
Schlumberger M, Schuster P, Schulz M, Immendörfer M, Mayer P, Bartholomä J, et al. Traumatic graft rupture after primary and revision anterior cruciate ligament reconstruction: retrospective analysis of incidence and risk factors in 2915 cases. Knee Surgery, Sport Traumatol Arthrosc [Internet]. 2017;25:1535–41. https://doi.org/10.1007/s00167-015-3699-0.
Snaebjörnsson T, Hamrin Senorski E, Sundemo D, Svantesson E, Westin O, Musahl V, et al. Adolescents and female patients are at increased risk for contralateral anterior cruciate ligament reconstruction: a cohort study from the Swedish National Knee Ligament Register based on 17,682 patients. Knee Surgery, Sport Traumatol Arthrosc [Internet]. 2017;25:3938–44. https://doi.org/10.1007/s00167-017-4517-7.
Pierce T, Issa K, Cassidy K, Festa A, McInerney V, Scillia A. Risk factors for contralateral ACL injury: a single institution case–control study. J Knee Surg [Internet]. 2018;31:846–50. https://doi.org/10.1055/s-0037-1615823.
Nawasreh Z, Adams G, Pryzbylkowski O, Logerstedt D. Influence of patient demographics and graft types on ACL second injury rates in ipsilateral versus contralateral knees: a systematic review and meta-analysis. Int J Sports Phys Ther [Internet]. 2018;13:561–74. Available from: https://spts.org/member-benefits-detail/enjoy-member-benefits/journals/ijspt/ijspt-v13n4#ijspt20180561
Fältström A, Hägglund M, Magnusson H, Forssblad M, Kvist J. Predictors for additional anterior cruciate ligament reconstruction: data from the Swedish national ACL register. Knee Surgery, Sport Traumatol Arthrosc [Internet]. 2016;24:885–94. https://doi.org/10.1007/s00167-014-3406-6.
Andernord D, Desai N, Björnsson H, Gillén S, Karlsson J, Samuelsson K. Predictors of contralateral anterior cruciate ligament reconstruction. Am J Sports Med [Internet]. 2015;43:295–302. https://doi.org/10.1177/0363546514557245.
Hamrin Senorski E, Svantesson E, Beischer S, Thomeé C, Thomeé R, Karlsson J, Samuelsson K. Low 1-year return-to-sport rate after anterior cruciate ligament reconstruction regardless of patient and surgical factors: a prospective cohort study of 272 patients. Am J Sports Med [Internet]. 2018;46:1551–8. https://doi.org/10.1177/0363546518765120.
Webster KE, Feller JA. Return to level I sports after anterior cruciate ligament reconstruction: evaluation of age, sex, and readiness to return criteria. Orthop J Sport Med [Internet]. 2018;6:232596711878804. https://doi.org/10.1177/2325967118788045. Study finding that in athletes under age 36, males had significantly higher return to sport rates than females
Kostyun RO, Burland JP, Kostyun KJ, Milewski MD, Nissen CW. Male and female adolescent athletes’ readiness to return to sport after anterior cruciate ligament injury and reconstruction. Clin J Sport Med. 2019;31(4):383–7.
Sims M, Mulcahey MK. Sex-specific differences in psychological response to injury and return to sport following ACL reconstruction. JBJS Rev [Internet]. 2018;6:e9–9. Available from: https://journals.lww.com/01874474-201807000-00009
Webster KE, Nagelli CV, Hewett TE, Feller JA. Factors associated with psychological readiness to return to sport after anterior cruciate ligament reconstruction surgery. Am J Sports Med [Internet]. 2018;46:1545–50. 10.1177/0363546518773757. Emphasizes current disparity in psychological readiness between male and female athletes to RTS after ACLR
Webster KE, McPherson AL, Hewett TE, Feller JA. Factors associated with a return to preinjury level of sport performance after anterior cruciate ligament reconstruction surgery. Am J Sports Med [Internet]. 2019;47:2557–62. https://doi.org/10.1177/0363546519865537.
Ageberg E, Forssblad M, Herbertsson P, Roos EM. Sex differences in patient-reported outcomes after anterior cruciate ligament reconstruction. Am J Sports Med [Internet]. 2010;38:1334–42. https://doi.org/10.1177/0363546510361218.
Teitsma XM, van der Hoeven H, Tamminga R, de Bie RA. Impact of patient sex on clinical outcomes. Orthop J Sport Med [Internet]. 2014;2:232596711455063. https://doi.org/10.1177/2325967114550638.
Webster KE, Feller JA. Younger patients and men achieve higher outcome scores than older patients and women after anterior cruciate ligament reconstruction. Clin Orthop Relat Res [Internet]. 2017;475:2472–80. Available from: https://journals.lww.com/00003086-201710000-00022
Obermeier MC, Sikka RS, Tompkins M, Nelson BJ, Hamilton A, Reams M, et al. Examination of Early Functional Recovery After ACL Reconstruction: functional milestone achievement and self-reported function. Sport Heal A Multidiscip Approach [Internet]. 2018;10:345–54. https://doi.org/10.1177/1941738118779762.
Kuenze C, Lisee C, Pfeiffer KA, Cadmus-Bertram L, Post EG, Biese K, Bell DR. Sex differences in physical activity engagement after ACL reconstruction. Phys Ther Sport [Internet]. 2019;35:12–7. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1466853X18304577
Kiapour AM, Fleming BC, Proffen BL, Murray MM. Sex influences the biomechanical outcomes of anterior cruciate ligament reconstruction in a preclinical large animal model. Am J Sports Med [Internet]. 2015;43:1623–31. https://doi.org/10.1177/0363546515582024.
Lesevic M, Kew ME, Bodkin SG, Diduch DR, Brockmeier SF, Miller MD, et al. The effect of patient sex and graft type on postoperative functional outcomes after primary ACL reconstruction. Orthop J Sport Med [Internet]. 2020;8:232596712092605. https://doi.org/10.1177/2325967120926052. Provides critical insight into gender-differences in biomechanical measures after ACLR
Arundale AJH, Capin JJ, Zarzycki R, Smith A, Snyder-Mackler L. Functional and patient-reported outcomes improve over the course of rehabilitation: a secondary analysis of the ACL-SPORTS Trial. Sport Heal A Multidiscip Approach [Internet]. 2018;10:441–52. https://doi.org/10.1177/1941738118779023.
Kim DK, Park WH. Sex differences in knee strength deficit 1 year after anterior cruciate ligament reconstruction. J Phys Ther Sci [Internet]. 2015;27:3847–9. Available from: https://www.jstage.jst.go.jp/article/jpts/27/12/27_jpts-2015-673/_article
Kuenze C, Lisee C, Birchmeier T, Triplett A, Wilcox L, Schorfhaar A, Shingles M. Sex differences in quadriceps rate of torque development within 1 year of ACL reconstruction. Phys Ther Sport [Internet]. 2019;38:36–43. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1466853X19300549
Kuenze CM, Trigsted S, Lisee C, Post E, Bell DR. Sex differences on the landing error scoring system among individuals with anterior cruciate ligament reconstruction. J Athl Train [Internet]. 2018;53:837–43. Available from: https://meridian.allenpress.com/jat/article/53/9/837/73385/Sex-Differences-on-the-Landing-Error-Scoring
Shelbourne KD, Gray T, Benner RW. Intercondylar notch width measurement differences between African American and White men and women with intact anterior cruciate ligament knees. Am J Sports Med [Internet]. 2007;35:1304–7. https://doi.org/10.1177/0363546507300060.
Everhart JS, Flanigan DC, Chaudhari AMW. Anteromedial ridging of the femoral intercondylar notch: an anatomic study of 170 archival skeletal specimens. Knee Surgery, Sport Traumatol Arthrosc [Internet]. 2014;22:80–7. https://doi.org/10.1007/s00167-012-2282-1.
Waiwaiole A, Gurbani A, Motamedi K, Seeger L, Sim MS, Nwajuaku P, et al. Relationship of ACL injury and posterior tibial slope with patient age, sex, and race. Orthop J Sport Med [Internet]. 2016;4:232596711667285. https://doi.org/10.1177/2325967116672852.
Omololu BB, Ogunlade OS, Gopaldasani VK. Normal Q-angle in an adult Nigerian population. Clin Orthop Relat Res [Internet]. 2009;467:2073–6. Available from: https://journals.lww.com/00003086-200908000-00021
Trojian TH, Collins S. The anterior cruciate ligament tear rate varies by race in professional women’s basketball. Am J Sports Med [Internet]. 2006;34:895–8. https://doi.org/10.1177/0363546505284384.
Li F, Qin L, Gong X, Huang Z, Wang T, Liu Z, et al. The Chinese ACL injury population has a higher proportion of small ACL tibial insertion sizes than Western patients. Knee Surgery, Sport Traumatol Arthrosc [Internet]. 2020;28:888–96. https://doi.org/10.1007/s00167-019-05541-z.
Zhang C, Xie G, Fang Z, Zhang X, Huangfu X, Zhao J. Assessment of relationship between three dimensional femoral notch volume and anterior cruciate ligament injury in Chinese Han adults: a retrospective MRI study. Int Orthop [Internet]. 2019;43:1231–7. https://doi.org/10.1007/s00264-018-4068-7.
Collins JE, Katz JN, Donnell-Fink LA, Martin SD, Losina E. Cumulative incidence of ACL reconstruction after ACL injury in adults. Am J Sports Med [Internet]. 2013;41:544–9. https://doi.org/10.1177/0363546512472042.
Bram JT, Talathi NS, Patel NM, DeFrancesco CJ, Striano BM, Ganley TJ. How do race and insurance status affect the care of pediatric anterior cruciate ligament injuries? Clin J Sport Med [Internet]. 2018;Publish Ah. Available from: https://journals.lww.com/00042752-900000000-99090; First study to investigate differences in isokinetic strength testing after pediatric ACLR by race and insurance status
Navarro RA, Prentice HA, MCS I, Wyatt R, Maletis GB. The association between race/ethnicity and revision following ACL reconstruction in a universally insured cohort. J Bone Jt Surg [Internet]. 2019;101:1546–53. https://doi.org/10.2106/JBJS.18.01408. Highlighted racial disparity in elective revision following ACLR, given a universally insured cohort and copmarable care through their institution. Emphasizes the need for fruther investigation into barriers to equal access to care
Inacio MCS, Paxton EW, Maletis GB, Csintalan RP, Granan L-P, Fithian DC, et al. Patient and surgeon characteristics associated with primary anterior cruciate ligament reconstruction graft selection. Am J Sports Med [Internet]. 2012;40:339–45. https://doi.org/10.1177/0363546511424130.
Spindler KP, Huston LJ, Zajichek A, Reinke EK, Amendola A, Andrish JT, et al. Anterior cruciate ligament reconstruction in high school and college-aged athletes: does autograft choice influence anterior cruciate ligament revision rates? Am J Sports Med [Internet]. 2020;48:298–309. https://doi.org/10.1177/0363546519892991.
Ramkumar PN, Tariq MB, Amendola A, Andrish JT, Brophy RH, Dunn WR, et al. Risk factors for loss to follow-up in 3202 patients at 2 years after anterior cruciate ligament reconstruction: implications for identifying health disparities in the MOON Prospective Cohort Study. Am J Sports Med [Internet]. 2019;47:3173–80. https://doi.org/10.1177/0363546519876925.
Maletis GB, Inacio MCS, Funahashi TT. Risk factors associated with revision and contralateral anterior cruciate ligament reconstructions in the Kaiser Permanente ACLR Registry. Am J Sports Med [Internet]. 2015;43:641–7. https://doi.org/10.1177/0363546514561745.
Gallo MC, Bolia IK, Jalali O, Rosario S, Rounds A, Heidari KS, et al. Risk factors for early subsequent (revision or contralateral) ACL reconstruction: a retrospective database study. Orthop J Sport Med [Internet]. 2020;8:232596711990117. https://doi.org/10.1177/2325967119901173.
Capogna BM, Mahure SA, Mollon B, Duenes ML, Rokito AS. Young age, female gender, Caucasian race, and workers’ compensation claim are risk factors for reoperation following arthroscopic ACL reconstruction. Knee Surgery, Sport Traumatol Arthrosc [Internet]. 2020;28:2213–23. https://doi.org/10.1007/s00167-019-05798-4.
Pullen WM, Bryant B, Gaskill T, Sicignano N, Evans AM, DeMaio M. Predictors of revision surgery after anterior cruciate ligament reconstruction. Am J Sports Med [Internet]. 2016;44:3140–5. https://doi.org/10.1177/0363546516660062.
Bokshan SL, DeFroda SF, Owens BD. Risk factors for hospital admission after anterior cruciate ligament reconstruction. Arthrosc J Arthrosc Relat Surg [Internet]. 2017;33:1405–11. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0749806317301275
Cooper JD, Lorenzana DJ, Heckmann N, McKnight B, Mostofi A, Gamradt SC, Rick Hatch GF III. The effect of obesity on operative times and 30-day readmissions after anterior cruciate ligament reconstruction. Arthrosc J Arthrosc Relat Surg [Internet]. 2019;35:121–9. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0749806318306200
Li LT, Bokshan SL, McGlone PJ, Owens BD. Decline in racial disparities for United States hospital admissions after anterior cruciate ligament reconstruction from 2007 to 2015. Orthop J Sport Med [Internet]. 2020;8:232596712096447. 10.1177/2325967120964473. Outlines recent improvement of disparity in hospitalizations by race after ACLR
Nwachukwu BU, Voleti PB, Berkanish P, Chang B, Cohn MR, Williams RJ, Allen AA. Return to play and patient satisfaction after ACL reconstruction: study with minimum 2-year follow-up. J Bone Joint Surg Am. 2017;99:720–5.
Emmonds S, Heyward O, Jones B. The challenge of applying and undertaking research in female sport. Sport Med - Open [Internet]. 2019;5:51. https://doi.org/10.1186/s40798-019-0224-x.
Hall WJ, Chapman MV, Lee KM, Merino YM, Thomas TW, Payne BK, Eng E, Day SH, Coyne-Beasley T. Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: a systematic review. Am J Public Health [Internet]. 2015;105:e60–76. https://doi.org/10.2105/AJPH.2015.302903.
FitzGerald C, Hurst S. Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics [Internet]. 2017;18:19. https://doi.org/10.1186/s12910-017-0179-8.
Druckman JN, Trawalter S, Montes I, Fredendall A, Kanter N, Rubenstein AP. Racial bias in sport medical staff’s perceptions of others’ pain. J Soc Psychol. 2018;158:721–9.
Saha S, Komaromy M, Koepsell TD, Bindman AB. Patient-physician racial concordance and the perceived quality and use of health care. Arch Intern Med [Internet]. 1999;159:997. https://doi.org/10.1001/archinte.159.9.997.
Walker KO, Moreno G, Grumbach K. The association among specialty, race, ethnicity, and practice location among California physicians in diverse specialties. J Natl Med Assoc [Internet]. 2012;104:46–52. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0027968415301267
Poma PA. Race/ethnicity concordance between patients and physicians. J Natl Med Assoc [Internet]. 2017;109:6–8. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0027968416301328
Poon S, Kiridly D, Mutawakkil M, Wendolowski S, Gecelter R, Kline M, et al. Current trends in sex, race, and ethnic diversity in orthopaedic surgery residency. J Am Acad Orthop Surg [Internet]. 2019;27:e725–33. Available from: http://journals.lww.com/00124635-201908150-00009. Outlines the current landscape of diversity in orthopedic surgery residency programs and important areas to grow in representation
McDonald TC, Drake LC, Replogle WH, Graves ML, Brooks JT. Barriers to increasing diversity in orthopaedics. JBJS Open Access [Internet]. 2020;5:e0007–7. https://doi.org/10.2106/JBJS.OA.20.00007.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Sai K. Devana, Carlos Solorzano, Benedict Nwachukwu, and Kristofer J. Jones declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
All authors have no financial relationships to disclose
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Gender and Racial Disparities
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Devana, S.K., Solorzano, C., Nwachukwu, B. et al. Disparities in ACL Reconstruction: the Influence of Gender and Race on Incidence, Treatment, and Outcomes. Curr Rev Musculoskelet Med 15, 1–9 (2022). https://doi.org/10.1007/s12178-021-09736-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12178-021-09736-1