Abstract
Purpose
Selecting patients with coronary multivessel disease (MVD) or no stenosis using myocardial perfusion imaging (MPI) is challenging. We aimed to create a model to predict MVD using a combination of quantitative MPI values and background factors of patients. We also assessed whether patients in the same database could be selected who do not require rest studies (stress-only imaging).
Methods
We analyzed data from 1001 patients who had been assessed by stress MPI at 12 centers and 463 patients who had not undergone revascularization in Japan. Quantitative values based on MPI were obtained using cardioREPO software, which included myocardial perfusion defect scores, left ventricular ejection fractions and volumes. Factors in MPI and clinical backgrounds that could predict MVD were investigated using univariate and multivariate analyses. We also investigated whether stress data alone could predict patients without coronary stenosis to identify candidates for stress-only imaging.
Results
We selected summed stress score (SSS), rest end-diastolic volume, and hypertension to create a predictive model for MVD. A logistic regression model was created with an area under the receiver operating characteristics curve (AUC) of 0.825. To more specifically predict coronary three-vessel disease, the AUC was 0.847 when SSS, diabetes, and hypertension were selected. The mean probabilities of abnormality based on the MVD prediction model were 12%, 24%, 40%, and 51% for no-, one-, two-, and three-vessel disease, respectively (p < 0.0001). For the model to select patients with stress-only imaging, the AUC was 0.78 when the model was created using SSS, stress end-systolic volume and the number of risk factors (diabetes, hypertension, chronic kidney disease, and a history of smoking).
Conclusion
A model analysis combining myocardial SPECT and clinical data can predict MVD, and can select patients for stress-only tests. Our models should prove useful for clinical applications.
Similar content being viewed by others
Introduction
Visual evaluation among nuclear cardiology examinations is the first-line assessment of myocardial perfusion defects and abnormalities. However, quantitative evaluations using indices calculated from ungated and gated myocardial perfusion imaging (MPI) have recently become prevalent and are used to treat coronary artery disease (CAD) [1]. Quantitative analyses using dedicated software and defect scoring have become popular for diagnosing myocardial ischemia, as well as ischemia or infarction from stress and rest data. These quantitative methods are effective for diagnostic and prognostic evaluation [2,3,4].
However, conventional single-photon emission computed tomography (SPECT) can accurately detect localized ischemia of one-vessel disease, but its ability to estimate multivessel (MVD), especially three-vessel (3VD) disease is limited. That is, even in patients with MVD, only an area with the most severe stenosis might be detected as a culprit lesion, or the phenomenon of balanced ischemia could result in no discernible perfusion defect. One way to compensate for this is to detect left ventricular functional abnormalities after stress tests, such as transient ischemic dilation and reduced left ventricular contractility after stress [5,6,7]. However, how to integrate and apply these data has not been investigated in detail.
Stress-only tests have been recommended to reduce the radiation dose and frequency of SPECT examinations [8]. However, how to select patients who do not require rest tests is also important to consider in clinical practice.
Here, we aimed to create models with which to predict patients with MVD and to select patients who need only stress tests based on their background and quantitative values derived from myocardial perfusion SPECT images.
Methods
Demographics
We selected data from a multicenter database of 1001 patients who had been evaluated by MPI at 12 centers in Japan. Our previous findings using this database are published elsewhere [9, 10]. The database includes age, sex, height, weight, gated SPECT data such as summed stress/rest/difference scores (SSS/SRS/SDS), left ventricular ejection fraction (EF), end-diastolic and end-systolic volumes (EDV and ESV, respectively), risk factors of CAD, degree of coronary artery narrowing on selective coronary angiography (CAG) or coronary CT angiography (CCTA), and a history of percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG). Data based on gated SPECT were analyzed using cardioREPO software, which we developed in collaboration with FUJIFILM Toyama Chemical, Co, Ltd. (Tokyo, Japan) and EXINI Diagnostics (Lund, Sweden).
The database consisted of 1,001 patients (male, n = 750; and female, n = 251), with a mean age of 69 ± 10 (range 21–98) years (Table 1). To increase the reliability of detecting CAD, we excluded 430 patients who had undergone coronary revascularization and 108 with no vessel disease (0VD) despite previous myocardial infarction with SRS ≥ 7. The latter patients were described as 0VD based on the latest CAG findings after coronary revascularization. We finally analyzed data from 463 patients of whom 324 (70%) were male.
Based on non-gated SPECT data, the means of SSS, SRS, and SDS, were 6.9 ± 8.2, 4.5 ± 7.2, and 2.9 ± 3.2. Gated SPECT data were calculated using cardioREPO software (FUJIFILM Toyama Chemical Co. Ltd., and EXINI Diagnostics AB). The left ventricular functional parameters were as follows: EDV at stress (sEDV) and at rest (rEDV), 101 ± 38 and 101 ± 36 mL, respectively; ESV at stress (sESV) and at rest (rESV), 36 ± 27 and 34 ± 26 mL, respectively; and EF at stress (sEF) and at rest (rEF), 67 ± 12 and 68 ± 12%, respectively.
The ratios of comorbidities were 45%, 73%, 64%, 34%, and 16% for diabetes mellitus (DM), hypertension (HT), dyslipidemia (DL), chronic kidney disease (CKD), and old myocardial infarction OMI.
Definition of coronary artery disease
We diagnosed CAD based on the American Heart Association (AHA) definition as significant (≥ 75%) stenosis of the coronary artery on coronary angiograms.
Myocardial perfusion imaging
Patients were assessed using a 1-day protocol of MPI with standard exercise (37%) or with pharmacological (63%, adenosine, 120 μg/mL × 6 min) stress and SPECT at the participating hospitals. All these institutions used 99mTc-labeled hexakis-2-methoxyisobutylisonitrile (MIBI), with a second injection dose that was 2–threefold more than the first dose. The total dose was 740–1110 MBq.
SPECT data acquisition and processing
SPECT data were acquired using a standard image acquisition protocol in each hospital [11, 12], but the precise methods were not regulated. The manufacturers of the SPECT equipment included Siemens, GE, Philips, Hitachi, and Picker companies. The energy setting was centered at 140 keV with a 15–20% window). Collimators were either low-energy high-resolution or cardiac high-resolution types. SPECT imaging duration ranged from 20 to 50 s per projection, and projection images were collected in a 64 \(\times\) 64 matrix. SPECT collection step angles ranged from 5° to 9°, with a rotational range of 180° or 360°. The ECG gating of the dual-head SPECT system was 16 or 8 frames per cardiac cycle. SPECT data were reconstructed using a filtered back projection method but one institution used a maximum-likelihood expectation maximization method. Attenuation and scatter correction were not applied. The image quality of the SEPCT data was confirmed in a core laboratory.
Artificial neural network
Left ventricular function was analyzed throughout the study using cardioREPO as described [9, 13]. Briefly, we determined the shape of the entire left ventricle using an active-shape model for left ventricular contour extraction. After extracting the contours of candidate regions with low accumulation, the probability of anomalies was determined using an artificial neural network (ANN). The method is based on features such as shape, extent, location, number, perfusion uniformity, local motion, wall thickening, and sex to comprehensively determine the presence or absence of ischemia as in clinical human diagnosis. The ANN was trained on a multicenter database of 99mTc-MIBI myocardial perfusion SPECT data derived from 1001 patients, and on interpretations by nuclear cardiology specialists.
Defect scoring
We assessed SPECT images by dividing the entire left ventricular myocardium into 17 segments, then scoring each segment from normal to complete defects as 0–5 and calculating total scores. The summed deficit scores in stress and rest segments on images were defined as SSS and SRS, respectively. Thereafter, cardioREPO automatically calculated SDS (ischemia scores) by subtracting the SRS from the SSS for each segment. A normal MPI database (JSNM standard) [14] created by a working group of Japanese Society of Nuclear Medicine (JSNM) is included in cardioREPO.
Statistics
Data are presented as means ± standard deviation (SD). Groups were compared using one-way analysis of variance (ANOVA) and t tests. Explanatory variables were analyzed using univariable and multivariable logistic regression models and receiver operating characteristics (ROC) analysis with areas under the ROC curves (AUC). The cutoff of the variables was set to the value that maximized (sensitivity + specificity − 1). Valid variables with < 0.10 in the univariate analyses were entered into a multivariate logistic regression analysis. Anomaly probabilities were calculated based on the variables as:
using JMP v. 14 (SAS Institute Inc., Cary, NC, USA) statistical software. Values with P < 0.05 were considered statistically significant.
Results
Univariate analysis to predict MVD
Coronary stenosis was estimated by logistic regression analysis including all variables and MVD was defined as coronary two- or three-vessel disease (Table 2). The results for SSS, SRS, SDS, sEDV, sEF, sESV, rEDV, rEF, and rESV based on non-gated and gated SPECT were significant. Among the factors associated with disease states, DM, HT, DL, CKD (defined as eGFR < 60 mL/min/1.73 m2), smoking history, angina pectoris (AP), and OMI were significant. However, neither of the sEDV/rEDV and sESV/rESV ratios that correspond to transient ischemic dilation, was significant.
Univariate analysis to predict 3VD
Three-vessel disease was also estimated using logistic regression analysis (Table 3).
Volume, disease status, and smoking history were significantly associated with defect score and cardiac function like MVD, whereas the sEDV/rEDV and sESV/rESV ratios were not.
Comparisons among groups with and without coronary stenosis
We compared variables for no-, one-, two-, and three- vessel disease (0, 1, 2, and 3VD, respectively) using one-way ANOVA (Table 4).
Differences among groups and factors associated with comorbidities were significant, whereas CKD and sEDV/rEDV were not.
Multivariate analysis to predict MVD
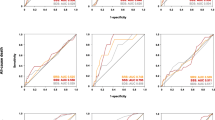
We attempted to create a predictive model for MVD by selecting clinically generalizable items that significantly differed (p < 0.1). Multivariate stepwise regression selected SSS, rEDV, and HT that might predict MVD. Table 5 shows estimates of these parameters, and the AUC was 0.825 (Fig. 1).
Multivariate analysis to predict 3VD
We created a model to predict 3VD by including SSS, DM, and HT in the multivariate analysis. Table 5 shows the parameter estimates and the AUC was 0.847 (Fig. 1).
Probability of MVD
We calculated the probability of 0, 1, 2, and 3VD using the model:
The average probabilities of abnormality in the MVD prediction model were 12%, 24%, 40%, and 51% for 0, 1, 2, and 3VD, respectively (p < 0.0001; Fig. 2).
Probability of 3VD
The probability of 3VD was calculated using the model:
A comparison of 0, 1, 2, and 3VD using this model revealed that the probabilities of abnormalities were 5.7%, 9.9%, 17.0%, and 33.0%, respectively (p < 0.0001; Fig. 2).
MVD vs. 3VD prediction models
We compared the two models using a bivariate analysis to determine which was more appropriate (Fig. 3). The predicted likelihood was higher, and the statistical significance of differences among groups was relatively higher for the MVD, than the 3VD model.
Comparison of MVD and 3VD prediction models. Probability in MVD and 3VD prediction models is shown in vertical and horizontal axes, respectively. Blue circles, green triangles, brown triangles, and red squares represent 0VD, 1VD, 2VD, and 3VD, respectively. MVD multivessel disease, VD vessel disease
Prediction of 0VD for stress-only imaging
We investigated whether MPI with exercise or adenosine stress alone can predict 0VD, that is, whether stress-only imaging can exclude significant coronary stenosis. We created a prediction model for 0VD based on quantitative values obtained from stress myocardial perfusion SPECT and patient background factors. The results of the stepwise regression showed that SSS contributed most to the creation of an accurate prediction model (AUC, 0.755), followed by sESV (AUC, 0.699) and the accumulation of multiple risk factors (AUC, 0.657). We calculated the number of risk factors using the sum of the factors (0–4) DM, HT, CKD, and a history of smoking.
The AUC of the model with SSS plus sESV was 0.759, and slightly improved over SSS alone. Adding more risk factors to SSS and sESV resulted in a more accurate prediction model with an AUC of 0.777 (Fig. 1).
Discussion
Although detecting MVD using MPI has been limited, the present study revealed that the probability of MVD can be estimated using a model that combines quantitative information from myocardial perfusion SPECT and the backgrounds of patients. Our model selected candidates appropriate for stress-only imaging,
Application of SPECT for MVD
Several reasons have been postulated to explain the limited ability of SPECT to diagnose MVD [15]. One is that 75% coronary artery stenosis might not result in significantly reduced perfusion. Furthermore, linearity between true myocardial blood flow and myocardial accumulation has been considered insufficient with single-photon radiopharmaceuticals [16, 17]. Lesions with the worst stenosis might be detected, whereas less severe areas might be overlooked, and 3VD might be undetectable due to balanced ischemia [18, 19], which is a limitation of SPECT based on relative count distribution. Therefore, we considered that myocardial perfusion combined with left ventricular function and patient background could predict MVD. We confirmed that a judgement of myocardial defects was insufficient, but adding cardiac function and clinical background surpassed the perfusion-only method. In fact, DM, HT and smoking were factors associated with CAD; thus having more than one factor might indicate a higher likelihood of CAD as shown in our models. We did not include DL in the list of multiple factors, because we found that the possibility of CAD was statistically lower when DL was included. This might be associated with the fact that the prevalent treatment of DL with statins also reduces the risk of all-cause mortality in patients with a medical history of CAD [20, 21].
Stress-only imaging
The stress-only SPECT concept is becoming widespread worldwide, because the burden on patients can be reduced by not having to endure the rest test when stress myocardial perfusion scintigraphy clearly shows no possibility of CAD [5, 6, 22]. This approach is also recommended by the International Atomic Energy Agency Nuclear Cardiology Protocols Study (INCAPS) [8]. However, stress tests under low-risk conditions have not been routinely applied in Japan. The conventional method of visual assessment based only on stress perfusion defects might not correctly assess CAD and overlook patients who should actually be indicated for further coronary artery assessments. Therefore, we also investigated whether myocardial perfusion, left ventricular function, and the backgrounds of patients can be used to discriminate candidates for stress-only imaging.
Selection of patients from the multicenter database
Quantitative and clinical data from a multicenter database were analyzed to create a model to predict MVD. We used information collected from several centers where patient background factors including the presence of CAD and myocardial perfusion were complete. Therefore, the selection of patients might have been more heterogeneous than in single-center studies. However, that the database reflected the average patient population indicated for MPI studies could be an advantage in Japan.
We excluded patients who had been treated by coronary revascularization. One reason was that post-treatment status was too confusing to accurately assess, even with contemporary CAG. Another reason was that such clinical predictions of MVD do not apply to patients after revascularization. Although the model was based on patients selected under these conditions, we generated accurate models with AUCs of 0.825 and 0.847 for MVD and 3VD, respectively, and the specificity and sensitivity of the models were both ~ 80%.
Comparison with conventional MVD detection
The indicators of high risk include MVD and left main trunk disease, decreased wall motion representing stunned myocardium with stress, LVEF < 45% at rest or stress, a decrease in LVEF of ≥ 5% after stress, left ventricular transient ischemic dilation (TID; ventricular cavitary enlargement > 10% compared with resting state), increased radioisotope accumulation in the lung field, and right ventricular delineation [23,24,25,26,27]. However, even if one of these factors indicated the possibility of MVD, the probability remained unknown due to the limitations of single factor estimation. The present results quantified the likelihood of MVD, which might provide more specific information than conventional methods. The results of our multivariate analysis showed that indices equivalent to TID and findings of post-stress dysfunction such as decreased EF after stress, were not significant beyond the combination of SSS and ESV. This does not imply that post-stress dysfunction has no value for individual patients, but rather that comprehensive judgment is still needed.
Roles of functional stress imaging and CCTA
In addition to MPI, coronary CT angiography (CCTA) is becoming more popular in routine clinical practice to non-invasively assess coronary arteries. Although CCTA provides a good morphological assessment of coronary artery stenosis and plaque, it is not necessarily suitable for evaluating actual myocardial ischemia [28,29,30]. In addition, CCTA might not be sufficient for patients with arrhythmia and/or severe calcification, and the side effects of radiation exposure, and the effects of contrast media in patients with CKD need to be understood and considered. However, both MPI and CCTA are useful tests for diagnosing CAD, and complementary roles for the diagnosis of CAD should be emphasized [31]. In general, CCTA and MPI are often the imaging modalities of choice for predicting the pre-test likelihood of moderate CAD. Therefore, if patients are initially assessed using MPI, the probability of MVD will help to select subsequent diagnostic procedures. If patients initially assessed using CCTA have no obvious stenosis, the possibility of CAD is considered low. However, when the culprit coronary arteries and the degree of ischemia cannot be fully evaluated because of issues such as calcification, or several coronary arteries with similar degrees of stenosis, SPECT should be considered to estimate the possibility of MVD from the viewpoint of perfusion and function.
Japanese Circulation Society’s guideline focused update (2022) on diagnosis and treatment in patients with stable CAD advocate the use of functional stress imaging and CCTA as follows [32]. In institutions where a CT scanner is the only imaging device, it is suggested that CCTA first rule out non-obstructive coronary artery. If the institution is experienced with functional stress imaging including myocardial SPECT, it is suitable to mainly apply those imaging techniques for diagnosis and risk stratification. In institutions capable of performing multimodal imaging, CCTA is the preferred imaging to rule out the presence of CAD. On the other hand, stress imaging is preferred as an initial imaging test in patients with a high pre-test probability or known history of CAD for risk assessment. This approach can be summarized as “rule-out dominant” and “rule-in dominant” strategies for CCTA and myocardial perfusion SPECT, respectively.
Candidate patients for stress-only imaging
We also developed a model to predict candidates for stress-only imaging, and the AUC was ~ 0.8. Although the model can be clinically applied, the AUC indicated that some patients with coronary stenosis might be overlooked. When we confirmed stenosis in patients despite a high probability of 0VD, ischemia and post-stress dysfunction were not evident, and functional status was good. This could mean that the study included patients whose status had reached the limitations of SPECT imaging. Therefore, patients with significant anginal symptoms or suspected coronary stenosis based on overall clinical factors should be evaluated by stress and rest tests even if the model-based risk is low.
Model-based approach
The prognostic value of MPI in the absence of ischemia has been confirmed by national and international multicenter studies [3, 4, 33, 34]. However, the model-based approach might enhance the possibility of MVD even in patients diagnosed with MPI in the absence of perfusion defects and ischemia, by combining cardiac function and clinical factors, indicating further examinations for CAD. Another possible option is to use a model for selecting patients for stress-only test by omitting the rest test. Ultimately, prognosis together with such predictions will require evaluation, but since the database did not include prognostic information, further studies will be required to determine the prognostic value of the model.
Whether or not MVD can be predicted by resting MPI alone needs to be discussed. First, a model including only resting MPI could be generated to predict MVD using quantitative values and clinical information obtained in the same manner as we analyzed in this study. However, we found that the SSS obtained by stress MPI was an indispensable factor for a highly accurate MVD prediction model. Since stress-induced ischemia has significant roles for the diagnosis of the severity of CAD and management strategy, the rest-only model might overlook the possibility of the MVD.
Limitations
Patients undergoing revascularization were excluded, because CAD had already been evaluated, which limited the number of patients. Therefore, in principle, our findings should be applied to patients who have not been evaluated by CAG.
This study included SPECT and partial CCTA information without stress myocardial perfusion magnetic resonance imaging (MRI), which a noninvasive method of coronary artery evaluation. A recent meta-analysis of stress myocardial perfusion MRI with gadolinium contrast media and pharmacological stress with adenosine has shown that the mean diagnostic sensitivity and specificity for coronary stenosis were 91% and 81%, respectively [35].
In addition, although we evaluated the possibility of MVD, the model does not determine which coronary artery is significantly stenosed. Further study is needed to accumulate more data.
Conclusion
Our predictive model created by combining myocardial SPECT and clinical information can predict MVD and should generate valuable additive information. We also created a model for selecting candidates for stress-only imaging. A database of many inter-institutional studies will be required to validate this model.
References
Dorbala S, Ananthasubramaniam K, Armstrong IS, Chareonthaitawee P, DePuey EG, Einstein AJ, et al. Single photon emission computed tomography (SPECT) myocardial perfusion imaging guidelines: instrumentation, acquisition, processing, and interpretation. J Nucl Cardiol. 2018;25:1784–846. https://doi.org/10.1007/s12350-018-1283-y.
Nakajima K, Kusuoka H, Nishimura S, Yamashina A, Nishimura T. Prognostic value of myocardial perfusion and ventricular function in a Japanese multicenter cohort study (J-ACCESS): the first-year total events and hard events. Ann Nucl Med. 2009;23:373–81. https://doi.org/10.1007/s12149-009-0248-2.
Hachamovitch R, Berman DS, Shaw LJ, Kiat H, Cohen I, Cabico JA, et al. Incremental prognostic value of myocardial perfusion single photon emission computed tomography for the prediction of cardiac death: differential stratification for risk of cardiac death and myocardial infarction. Circulation. 1998;97:535–43. https://doi.org/10.1161/01.cir.97.6.535.
Nishimura T, Nakajima K, Kusuoka H, Yamashina A, Nishimura S. Prognostic study of risk stratification among Japanese patients with ischemic heart disease using gated myocardial perfusion SPECT: J-ACCESS study. Eur J Nucl Med Mol Imaging. 2008;35:319–28. https://doi.org/10.1007/s00259-007-0608-x.
Gibson PB, Demus D, Noto R, Hudson W, Johnson LL. Low event rate for stress-only perfusion imaging in patients evaluated for chest pain. J Am Coll Cardiol. 2002;39:999–1004. https://doi.org/10.1016/s0735-1097(02)01720-5.
Ueyama T, Takehana K, Maeba H, Iwasaka T. Prognostic value of normal stress-only technetium-99m myocardial perfusion imaging protocol. Comparison with standard stress-rest protocol. Circ J. 2012;76:2386–91. https://doi.org/10.1253/circj.cj-12-0081.
Liu H, Wu J, Miller EJ, Liu C, Yaqiang L, et al. Diagnostic accuracy of stress-only myocardial perfusion SPECT improved by deep learning. Eur J Nucl Med Mol Imaging. 2021;48:2793–800. https://doi.org/10.1007/s00259-021-05202-9.
Lindner O, Pascual TN, Mercuri M, Acampa W, Burchert W, Flotats A, et al. Nuclear cardiology practice and associated radiation doses in Europe: results of the IAEA Nuclear Cardiology Protocols Study (INCAPS) for the 27 European countries. Eur J Nucl Med Mol Imaging. 2016;43:718–28. https://doi.org/10.1007/s00259-015-3270-8.
Nakajima K, Kudo T, Nakata T, Kiso K, Kasai T, Taniguchi Y, et al. Diagnostic accuracy of an artificial neural network compared with statistical quantitation of myocardial perfusion images: a Japanese multicenter study. Eur J Nucl Med Mol Imaging. 2017;44:2280–9. https://doi.org/10.1007/s00259-017-3834-x.
Nakajima K, Okuda K, Watanabe S, Matsuo S, Kinuya S, Toth K, et al. Artificial neural network retrained to detect myocardial ischemia using a Japanese multicenter database. Ann Nucl Med. 2018;32:303–10. https://doi.org/10.1007/s12149-018-1247-y.
Tilkemeier PL, Bourque J, Doukky R, Sanghani R, Weinberg RL. ASNC imaging guidelines for nuclear cardiology procedures: standardized reporting of nuclear cardiology procedures. J Nucl Cardiol. 2017;24:2064–128. https://doi.org/10.1007/s12350-017-1057-y.
Dorbala S, Di Carli MF, Delbeke D, Abbara S, DePuey EG, Dilsizian V, et al. SNMMI/ASNC/SCCT guideline for cardiac SPECT/CT and PET/CT 1.0. J Nucl Med. 2013;54:1485–507. https://doi.org/10.2967/jnumed.112.105155.
Nakajima K, Matsuo S, Wakabayashi H, Yokoyama K, Bunko H, Okuda K, et al. Diagnostic performance of artificial neural network for detecting ischemia in myocardial perfusion imaging. Circ J. 2015;79:1549–56. https://doi.org/10.1253/circj.CJ-15-0079.
Nakajima K, Kumita S, Ishida Y, Momose M, Hashimoto J, Morita K, et al. Creation and characterization of Japanese standards for myocardial perfusion SPECT: database from the Japanese Society of Nuclear Medicine Working Group. Ann Nucl Med. 2007;21:505–11. https://doi.org/10.1007/s12149-007-0059-2.
Arbab-Zadeh A, Di Carli MF, Cerci R, George RT, Chen MY, Dewey M, et al. Accuracy of computed tomographic angiography and single-photon emission computed tomography-acquired myocardial perfusion imaging for the diagnosis of coronary artery disease. Circ Cardiovasc Imaging. 2015;8: e003533. https://doi.org/10.1161/CIRCIMAGING.115.003533.
Saraste A, Kajander S, Han C, Nesterov SV, Knuuti J. PET: Is myocardial flow quantification a clinical reality? J Nucl Cardiol. 2012;19:1044–59. https://doi.org/10.1007/s12350-012-9588-8.
Sciagra R, Lubberink M, Hyafil F, Saraste A, Slart R, Agostini D, et al. EANM procedural guidelines for PET/CT quantitative myocardial perfusion imaging. Eur J Nucl Med Mol Imaging. 2021;48:1040–69. https://doi.org/10.1007/s00259-020-05046-9.
Yokota S, Mouden M, Ottervanger JP. High-risk coronary artery disease, but normal myocardial perfusion: a matter of concern? J Nucl Cardiol. 2016;23:542–5. https://doi.org/10.1007/s12350-015-0167-7.
Baqi A, Ahmed I, Nagher B. Multi vessel coronary artery disease presenting as a false negative myocardial perfusion imaging and true positive exercise tolerance test: a case of balanced ischemia. Cureus. 2020;12: e11321. https://doi.org/10.7759/cureus.11321.
Nakamura H, Arakawa K, Itakura H, Kitabatake A, Goto Y, Toyota T, et al. Primary prevention of cardiovascular disease with pravastatin in Japan (MEGA Study): a prospective randomised controlled trial. Lancet. 2006;368:1155–63. https://doi.org/10.1016/s0140-6736(06)69472-5.
Taguchi I, Iimuro S, Iwata H, Takashima H, Abe M, Amiya E, et al. High-dose versus low-dose pitavastatin in Japanese patients with stable coronary artery disease (REAL-CAD): a randomized superiority trial. Circulation. 2018;137:1997–2009. https://doi.org/10.1161/CIRCULATIONAHA.117.032615.
Gutstein A, Bental T, Solodky A, Mats I, Zafrir N. Prognosis of stress-only SPECT myocardial perfusion imaging with prone imaging. J Nucl Cardiol. 2018;25:809–16. https://doi.org/10.1007/s12350-016-0617-x.
Matsumoto N, Sato Y, Suzuki Y, Kasama S, Nakano Y, Kato M, et al. Incremental prognostic value of cardiac function assessed by ECG-gated myocardial perfusion SPECT for the prediction of future acute coronary syndrome. Circ J. 2008;72:2035–9. https://doi.org/10.1253/circj.cj-08-0488.
Berman DS, Kang X, Slomka PJ, Gerlach J, de Yang L, Hayes SW, et al. Underestimation of extent of ischemia by gated SPECT myocardial perfusion imaging in patients with left main coronary artery disease. J Nucl Cardiol. 2007;14:521–8. https://doi.org/10.1016/j.nuclcard.2007.05.008.
van der Veen BJ, Kuperij N, Stokkel MP. Transient ischemic dilatation ratio derived from myocardial perfusion scintigraphy: what are we looking at? J Nucl Cardiol. 2010;17:207–15. https://doi.org/10.1007/s12350-009-9180-z.
Nishimura S, Mahmarian JJ, Verani MS. Significance of increased lung thallium uptake during adenosine thallium-201 scintigraphy. J Nucl Med. 1992;33:1600–7.
Nishimura T, Uehara T, Hayashida K, Kozuka T, Saito M, Sumiyoshi T. Quantitative assessment of thallium myocardial washout rate: importance of peak heart rate and lung thallium uptake in defining normal values. Eur J Nucl Med. 1987;13:67–71. https://doi.org/10.1007/BF00256018.
Meijboom WB, Van Mieghem CA, van Pelt N, Weustink A, Pugliese F, Mollet NR, et al. Comprehensive assessment of coronary artery stenoses: computed tomography coronary angiography versus conventional coronary angiography and correlation with fractional flow reserve in patients with stable angina. J Am Coll Cardiol. 2008;52:636–43. https://doi.org/10.1016/j.jacc.2008.05.024.
Tanami Y, Miller JM, Vavere AL, Rochitte CE, Dewey M, Niinuma H, et al. Nuclear stress perfusion imaging versus computed tomography coronary angiography for identifying patients with obstructive coronary artery disease as defined by conventional angiography: insights from the CorE-64 multicenter study. Heart Int. 2014;9:1–6.
de Graaf MA, Roos CJ, Mansveld JM, Kharagjitsingh AV, Dibbets-Schneider P, Kroft LJ, et al. Changes in ischaemia as assessed with single-photon emission computed tomography myocardial perfusion imaging in high-risk patients with diabetes without cardiac symptoms: relation with coronary atherosclerosis on computed tomography coronary angiography. Eur Heart J Cardiovasc Imaging. 2015;16:863–70. https://doi.org/10.1093/ehjci/jev003.
Naya M, Tamaki N. Stress MPI, coronary CTA, and multimodality for subsequent risk analysis. J Nucl Cardiol. 2016;23:198–201. https://doi.org/10.1007/s12350-016-0400-z.
Nakano S, Kohsaka S, Chikamori T, Fukushima K, Kobayashi Y, Kozuma K, et al. JCS 2022 guideline focused update on diagnosis and treatment in patients with stable coronary artery disease. Circ J. 2022. https://doi.org/10.1253/circj.CJ-21-1041.
Imamura Y, Fukuyama T, Nishimura S, Nishimura T, Japanese Assessment of Cardiac E, Survival S. Normal myocardial perfusion scan portends a benign prognosis independent from the pretest probability of coronary artery disease Sub-analysis of the J-ACCESS study. J Cardiol. 2009;54:93–100. https://doi.org/10.1016/j.jjcc.2009.04.014.
Nanasato M, Matsumoto N, Nakajima K, Chikamori T, Moroi M, Takehana K, et al. Prognostic impact of reducing myocardial ischemia identified using ECG-gated myocardial perfusion SPECT in Japanese patients with coronary artery disease: J-ACCESS 4 study. Int J Cardiol. 2018;267:202–7. https://doi.org/10.1016/j.ijcard.2018.05.090.
Schwitter J, Wacker CM, van Rossum AC, Lombardi M, Al-Saadi N, Ahlstrom H, et al. MR-IMPACT: comparison of perfusion-cardiac magnetic resonance with single-photon emission computed tomography for the detection of coronary artery disease in a multicentre, multivendor, randomized trial. Eur Heart J. 2008;29:480–9. https://doi.org/10.1093/eurheartj/ehm617.
Acknowledgements
This study used multicenter database created for neural network algorithm for myocardial perfusion imaging [9]. We appreciate the editorial assistance of Norma Foster.
Funding
This work is partly funded by Grant-in-Aid for Scientific Research (Kakenhi), No. 20K07990 (PI: Kenichi Nakajima).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
KN collaborates with, and is funded by FUJIFILM Toyama Chemical Co. Ltd.
Ethics approval
The study was approved by Ethics Committee of Kanazawa University, and patients at the participating hospitals provided written, informed consent to create the database using their clinical records.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kunita, Y., Nakajima, K., Nakata, T. et al. Prediction of multivessel coronary artery disease and candidates for stress-only imaging using multivariable models with myocardial perfusion imaging. Ann Nucl Med 36, 674–683 (2022). https://doi.org/10.1007/s12149-022-01751-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-022-01751-7