Abstract
Objective
Fertility preservation in women with cancer is important for improving their quality of life. Successful ovarian transposition protects the ovary from radiation and preserves ovarian endocrine function and fertility. With the increasing use of 18F-FDG PET/CT in gynecologic malignancies, the findings of transposed ovaries sometimes vary. This study aimed to characterize the 18F-FDG PET/CT findings of surgically transposed ovaries among a large number of patients with various medical conditions.
Methods
We retrospectively reviewed the medical records, including surgical history, and analyzed the findings of the transposed ovaries of patients who underwent ovarian transposition. Quantitative analysis was performed, and the maximum standardized uptake values (SUVs) were recorded. The Hounsfield unit (HU) and size (measured using the long diameter on the axial image) of the transposed ovary were evaluated.
Results
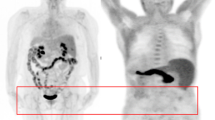
No significant change was found in the SUV of the transposed ovaries in relation to age and time after surgery. In two cases in which metastasis occurred in the transposed ovary, the lesions showed higher SUVs and HUs than did the other non-metastatic transposed ovaries. In several serial follow-up cases, varying 18F-FDG uptake was observed.
Conclusion
The 18F-FDG uptake pattern of the transposed ovary did not differ from that of the normal ovary. Misinterpretation should be avoided by considering surgical records, presence of surgical clips, and patients’ disease state. If there is a high uptake in the transposed ovary, it is necessary to check for soft tissue lesions and differentiate metastasis from the physiologic uptake.







Similar content being viewed by others
References
Angarita AM, Johnson CA, Fader AN, Christianson MS. Fertility preservation: a key survivorship issue for young women with cancer. Front Oncol. 2016;6:102.
Letourneau JM, Ebbel EE, Katz PP, Katz A, Ai WZ, Chien AJ, et al. Pretreatment fertility counseling and fertility preservation improve quality of life in reproductive age women with cancer. Cancer. 2012;118:1710–7.
Donnez J, Dolmans MM. Fertility preservation in women. N Engl J Med. 2018;378:400–1.
Wallace WH, Anderson RA, Irvine DS. Fertility preservation for young patients with cancer: who is at risk and what can be offered? Lancet Oncol. 2005;6:209–18.
Wallace WH, Thomson AB, Kelsey TW. The radiosensitivity of the human oocyte. Hum Reprod. 2003;18:117–21.
De Vos M, Smitz J, Woodruff TK. Fertility preservation in women with cancer. Lancet. 2014;384:1302–10.
Dursun P, Ayhan A, Yanik FB, Kuşçu E. Ovarian transposition for the preservation of ovarian function in young patients with cervical carcinoma. Eur J Gynaecol Oncol. 2009;30:13–5.
Morice P, Juncker L, Rey A, El-Hassan J, Haie-Meder C, Castaigne D. Ovarian transposition for patients with cervical carcinoma treated by radiosurgical combination. Fertil Steril. 2000;74:743–8.
Narayanan P, Sahdev A. The role of (18)F-FDG PET CT in common gynaecological malignancies. Br J Radiol. 2017;90:20170283.
Rockall AG, Cross S, Flanagan S, Moore E, Avril N. The role of FDG-PET/CT in gynaecological cancers. Cancer Imaging. 2012;12:49–65.
Akin EA, Kuhl ES, Zeman RK. The role of FDG-PET/CT in gynecologic imaging: an updated guide to interpretation and challenges. Abdom Radiol (NY). 2018;43:2474–86.
Liu Y. Benign ovarian and endometrial uptake on FDG PET-CT: patterns and pitfalls. Ann Nucl Med. 2009;23:107–12.
Nishizawa S, Inubushi M, Okada H. Physiological 18F-FDG uptake in the ovaries and uterus of healthy female volunteers. Eur J Nucl Med Mol Imaging. 2005;32:549–56.
Lerman H, Metser U, Grisaru D, Fishman A, Lievshitz G, Even-Sapir E. Normal and abnormal 18F-FDG endometrial and ovarian uptake in pre- and postmenopausal patients: assessment by PET/CT. J Nucl Med. 2004;45:266–71.
Chung HH, Kang WJ, Kim JW, Park NH, Song YS, Chung JK, et al. Characterization of surgically transposed ovaries in integrated PET/CT scan in patients with cervical cancer. Acta Obstet Gynecol Scand. 2007;86:88–93.
Zissin R, Metser U, Lerman H, Lievshitz G, Safra T, Even-Sapir E. PET-CT findings in surgically transposed ovaries. Br J Radiol. 2006;79:110–5.
Davidson T, Komisar O, Korach J, Felder S, Apter S, Ben-Haim S, et al. Physiologic uptake of 18F-FDG in transposed ovaries may mimic metastasis on 18F-FDG PET/CT imaging. Nucl Med Commun. 2018;39:171–8.
Agrawal K, Sajjan RS, Saad ZZ, Groves A, Bomanji J, Syed R. Transposed ovary mimicking a peritoneal implant on FDG PET/CT in a patient with carcinoma of the rectum. Eur J Nucl Med Mol Imaging. 2014;41:1642–3.
Morice P, Haie-Meder C, Pautier P, Lhomme C, Castaigne D. Ovarian metastasis on transposed ovary in patients treated for squamous cell carcinoma of the uterine cervix: report of two cases and surgical implications. Gynecol Oncol. 2001;83:605–7.
Janse JA, Sie-Go DM, Schreuder HW. Ovarian metastasis in a transposed ovary 10 years after primary cervical cancer: the importance of histologic examination and review of literature. BMJ Case Rep. 2011;2011:0420114155.
Chambers SK, Chambers JT, Kier R, Peschel RE. Sequelae of lateral ovarian transposition in irradiated cervical cancer patients. Int J Radiat Oncol Biol Phys. 1991;20:1305–8.
Feeney DD, Moore DH, Look KY, Stehman FB, Sutton GP. The fate of the ovaries after radical hysterectomy and ovarian transposition. Gynecol Oncol. 1995;56:3–7.
Pahisa J, Martínez-Román S, Martínez-Zamora MA, Torné A, Caparrós X, Sanjuán A, et al. Laparoscopic ovarian transposition in patients with early cervical cancer. Int J Gynecol Cancer. 2008;18:584–9.
Hoekman EJ, Knoester D, Peters AAW, Jansen FW, de Kroon CD, Hilders C. Ovarian survival after pelvic radiation: transposition until the age of 35 years. Arch Gynecol Obstet. 2018;298:1001–7.
Lee P, Greenfield JR, Ho KK, Fulham MJ. A critical appraisal of the prevalence and metabolic significance of brown adipose tissue in adult humans. Am J Physiol Endocrinol Metab. 2010;299:E601–6.
Cronin CG, Prakash P, Daniels GH, Boland GW, Kalra MK, Halpern EF, et al. Brown fat at PET/CT: correlation with patient characteristics. Radiology. 2012;263:836–42.
Steinberg JD, Vogel W, Vegt E. Factors influencing brown fat activation in FDG PET/CT: a retrospective analysis of 15,000+ cases. Br J Radiol. 2017;90:20170093.
Brendle C, Werner MK, Schmadl M, la Fougère C, Nikolaou K, Stefan N, et al. Correlation of brown adipose tissue with other body fat compartments and patient characteristics: a retrospective analysis in a large patient cohort using PET/CT. Acad Radiol. 2018;25:102–10.
Acknowledgements
This work was supported by the National Research Foundation of Korea (NRF) Grant funded by the Korea government (MSIT) (No. 2020M2D9A1093991).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest.
Ethical approval
Ethical approval was obtained from Severance Hospital Institutional Review Board (Approval number: 4-2020-1085).
Informed consent
The need of informed consent was waived by the IRB committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jo, K.H., Kim, S., Hwang, S.H. et al. Characteristics of surgically transposed ovaries on 18F-FDG PET/CT among patients with cancer. Ann Nucl Med 35, 1100–1108 (2021). https://doi.org/10.1007/s12149-021-01645-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-021-01645-0