Abstract
This study aims to examine premenstrual syndrome (PMS) in university students and their coping behaviors. 452 female students were included in this descriptive and correlational study. The data were collected using a descriptive information form, the Premenstrual Syndrome Scale (PMSS), and the Premenstrual Change Coping Inventory (PMS-Cope). PMS symptoms were found in 80.5% of students. Seeking positive affect-inducing activities to cope with PMS was found to be a significant predictor of reducing the severity of PMS (β =-0.265, p < .001). In coping with PMS, it is necessary to consider the perceptions of taking medication, seeking social support, or seeking positive affect-inducing activities as a coping method to determine the social and cultural beliefs of university students and control PMS. PMS is a significant health problem and raising awareness of the issue alone may not be enough. It should also be noted that the severity of PMS can vary markedly between ethnic groups, and women’s strategies for coping with symptoms and their effectiveness may differ between cultures. It is pivotal to develop strategies for university students to cope with PMS and provide personalized care.
Similar content being viewed by others
Premenstrual syndrome (PMS) is a common health issue characterized by physical, behavioral, and psychological symptoms that occur during the luteal phase of the menstrual cycle and disappear shortly after menstruation (Mumtaz et al., 2018; Dönmez & Gümüssoy, 2019) and can seriously affect the quality of life (Bhuvaneswari et al., 2019) and cause reduced performance and lack of concentration at work and school (Buddhabunyakan et al., 2017). Premenstrual dysphoric disorder (PMDD) is a more severe form of PMS, included as a psychiatric disorder in the fifth edition of the diagnostic and statistical manual for mental disorders (DSM-5) (Bhuvaneswari et al., 2019). Although the etiology of PMS is not exactly known, since its symptoms occur simultaneously with hormonal fluctuations of the menstrual cycle, it is reported to be associated with hormonal imbalances like estrogen excess and progesterone deficiency, some neurotransmitters like serotonin, GABA, opioids, and catecholamines (Stoner et al., 2017), age and genetic factors (Shrestha et al., 2019).
Clinical symptoms of PMS include changes in appetite, weight gain, abdominal pain, back pain, low back pain, headache, breast swelling and tenderness, nausea, constipation, anxiety, irritability, anger, fatigue, restlessness, and mood swings (Yesildere Saglam & Orsal, 2020). Irritability is the most prevalent mood symptom of PMDD, but depression, anxiety, and mood swings are also observed. Daily activities and interpersonal connections suffer as a result of physical and behavioral problems, including fatigue and difficulty concentrating (American Psychiatric Association, 2013; Yonkers & Simoni, 2018). PMDD symptoms are similar to PMS in that they emerge during the luteal phase and disappear once menstruation begins (Ryu & Kim, 2015; Petersen et al., 2016). But unlike PMS, PMDD frequently results in significant functional and social impairment, which harms one’s quality of life and overall well-being (Ryu & Kim, 2015).
The worldwide prevalence of women of reproductive age affected by PMS is 47.8% (Frey Nascimento et al., 2020). Premenstrual syndrome prevalence was found to be 53% in Ethiopia (Geta et al., 2020), 41.5% in Iran (Fatemi et al., 2019), 43% in India (Dutta & Sharma, 2021), and % 59, 50.3%, and 66% in high school, university students and married women in Turkey, respectively (Erbil & Yücesoy, 2021b). Up to 6% of reproductive-age women have PMDD (Yonkers & Simoni, 2018). Emotional dysregulation is a factor in both PMS and PMDD, and women with this condition have less effective coping mechanisms for stress (Wu et al., 2016). According to Forrester-Knauss et al. (2011), only 11.3% of women with moderate PMS and 24.6% of those with PMDD showed signs of significant depression. Evidence shows that women with PMS and PMDD have higher suicide rates than others (Pilver et al., 2013; Shams-Alizadeh et al., 2018).
Given that effective symptoms related to PMS and PMDD can make women more prone to suicidal thoughts, plans, and, in severe cases, attempts, this is an issue that needs to be addressed seriously by health professionals (Prasad et al., 2021). Women’s health-related quality of life is severely influenced by PMS, interfering with the development of nations by impairing daily activities (Tolossa & Bekele, 2014; Direkvand-Moghadam et al., 2014). PMS affects families, society, and the nation in general as well as women. Decreased work productivity due to school and work absenteeism is a potential economic burden for society (Kelderhouse & Taylor, 2013). Although PMS is a common public health problem, affecting more than half of women of reproductive age worldwide, including university students associated with poor quality of life and productivity, little is known about contributing factors and effective coping mechanisms (Eshetu et al., 2022).
In addition to pharmacological agents, non-pharmacological methods such as reflexology, acupuncture, acupressure, cognitive-behavioral approaches, and massage therapy are also employed to cope with PMS, which affects approximately one in every two women (Dadkhah et al., 2016; Cha & Nam, 2016; Izadi-Mazidi et al., 2016; Basogul et al. 2020). Raising awareness about the causes of PMS through health education is effective for women to take action to make changes in their lifestyles (Ramya et al. 2014). Eshetu et al. (2022) found that students mostly prefer rest and sleep as coping mechanisms. Bakır et al. (2021) demonstrate the efficacy of emotional freedom techniques in reducing students’ depressive affect, fatigue, nervousness, sleep-related changes, and swelling symptoms. Mizuta et al. (2022) suggested that exercise may reduce the severity of premenstrual symptoms. Belvederi Murri et al. (2019) found that exercise is useful in alleviating the signs of serious depression and lowering the death rate. Accordingly, exercising can contribute to managing PMS and PMDD.
It is essential to reduce symptoms, improve social and occupational functionality, prevent economic and psychological loss during the reproductive age, and improve the quality of life to cope with PMS. PMS and PMDD can lead to reduced quality of life and psychological problems, which is why the assessment of patients with PMS and PMDD premenstrual disorders should be more detailed. Given that PMS covers a significant period of a woman’s life and has many adverse effects, it is likely to negatively impact the development of individuals, their families, and community health. Therefore, interdisciplinary health support is necessary for women with PMS to improve their quality of life and cope with the adverse effects of PMS. An interdisciplinary approach is also essential for the effective and successful treatment of PMS and nurses, therapists, social workers, case managers, primary care physicians, and psychiatrists form an integral part of these disciplines and health services. It should be kept in mind that biological, psychological, and social factors have a significant effect on PMS and that everyone’s coping behavior with PMS may be different. It is important to prevent and manage PMS professionally and systematically. PMS affects not only the woman, but also the family, the community, and the nation at large, causing impaired work productivity, school, and work absenteeism, and creating a potential economic burden for society. Awareness should be raised about educating students about coping with PMS globally, developing positive attitudes, and improving PMS. This study was conducted to examine PMS and coping behaviors among university students.
The main hypothesis of the study is a relationship between coping behaviors with premenstrual syndrome and the severity of the premenstrual syndrome.
To achieve this aim, the study sought answers to the following questions.
-
1.
What is the frequency of premenstrual syndrome among university students?
-
2.
What are the coping behaviors with premenstrual syndrome?
-
3.
Does the severity of premenstrual symptoms affect coping behaviors?
Method
Study design and participants
This descriptive and correlational study was conducted between May-November 2020 at the School of Health and the Department of Nursing and Faculty of Arts and Sciences in a university located in the Black Sea region of Turkey.
The population consisted of female students studying in the Department of Nursing and the departments of Biology, Physics, English Language and Literature, Chemistry, Mathematics, History, and Turkish Language at the Literature of the Faculty of Arts and Sciences at a university located in the Black Sea region of Turkey. At the time of the research, there were a total of 1101 female students in these departments: 279 students in the nursing department, and 822 students in the Faculty of Arts and Sciences. It was planned to reach the entire population without making a sample selection, and 452 volunteer female students were recruited in the study sample: 194 in the nursing department and 258 in the Faculty of Arts and Sciences.
Female students who were over the age of 18, had no known physical and psychological disorders, and agreed to participate in the study were recruited for the study. Those with psychiatric diseases were excluded from the study. The data were collected using google forms sent to students’ e-mails due to the pandemic. Students could access the questions only after they were approved to participate in the study.
Data collection
The data were collected online using a descriptive information form, the Premenstrual Syndrome Scale (PMSS), and the Premenstrual Change Coping Inventory (PMS-Cope).
A descriptive information form
Developed in line with the literature (Kaiser et al., 2018), the form consists of 13 questions regarding socio-demographic data (age, university, place of residence, marital status, etc.), gynecological data, blood values, genetic factors of the students, their ability to cope with stress and the presence of anemia.
Premenstrual syndrome scale
The Premenstrual Syndrome Scale (PMSS) is a 44-item five-point Likert-type scale with 9 subscales developed by Gencdogan in 2006. Subscales of PMSS are depressive feelings, anxiety, fatigue, irritability, depressive thoughts, pain, changes in appetite, changes in sleeping habits and swelling (Gencdogan, 2006). PMSS items are scored as follows: 1: never, 2: rarely, 3: sometimes, 4: frequently, and 5: always. The lowest and the highest scores to be taken from the scale are 44 and 220. It is hypothesized that girls who receive a total PMSS score of 111 or higher have premenstrual syndromes. When analyzing the PMSS results, PMS is assumed to be present when more than 50% of the subscales have a high value (Gencdogan, 2006). In the original study, Cronbach’s Alpha coefficient of PMSS items was 0.75, while those of its subscales were between 0.75 and 0.91. In this study, Cronbach’s alpha coefficient is 0.96 for PMSS items and ranges between 0.76 and 0.91 for sub-scales.
Premenstrual change coping inventory
The “Premenstrual Change Coping Inventory” (PMS-Cope) scale was developed by Kaiser et al. (2018) and adapted for Turkish culture by Sarı Cetin and Erbil in 2020 and its validity and reliability study was conducted. The scale has 17 items and 3 subscales. Subscales are: “Seeking positive affect-inducing activities”, “Seeking support” and “Healthcare use behavior”. The scale is a 4-point Likert type and includes “strongly disagree” (1 point), “not sure” (2 points), “agree” (3 points), and “strongly agree” (4 points). The lowest and the highest scores to be obtained from the scale are 17 and 68 (Sarı Cetin & Erbil, 2020). In the Turkish original study, Cronbach alpha coefficients were found to be 0.86 for PMS-Cope, 0.84 for the Seeking positive affect-inducing activities subscale, 0.89 for Seeking support subscale, 0.78 for the healthcare use behavior subscale (Sarı Cetin & Erbil, 2020). In this study, Cronbach’s alpha coefficients were found to be 0.82, 0.75, 0.83, and 0.62, respectively.
Statistical analysis
After examining the normality distribution, descriptive statistical methods including frequency, percentage, mean, and standard deviation were used in the analysis of the data. Independent intergroup differences were analyzed with a t-test and One-Way ANOVA test. The fit of the data to normal distribution was evaluated using skewness and kurtosis tests with values of PMS-Cope − 0.324 and 0.172 and PSSS − 0.092 and − 0.397, respectively. Pearson correlation analysis was used to evaluate the relationship between the scale mean scores. Multiple linear regression analysis was used to evaluate the relationship between PMS-Cope and its subscales with PMSS. The reliability of the scales was evaluated with the Cronbach Alpha coefficient. The significance level was considered as p < .05.
Results
Sociodemographic and menstrual characteristics of university students
According to the results, the mean age of the participants was 20.79 ± 2.27, 62.8% were studying in the Faculty of Arts and Sciences, 37.2% were in the nursing department, and 29% were first-year students. 53.5% lived in the province, and 98.7% were single. The mean age of menarche was 13.31 ± 1.33, and the average duration of menstruation was 5.92 ± 2.09 days. 73.5% had a period every 21–35 days, 73% had regular menstrual periods, 82.3% had dysmenorrhea, 56.9% had premenstrual symptoms in their mother and sister, and 28.8% had anemia. PMSS scores were higher in those with irregular menses (p = .000), those with PMS problems in their mother and sister (p = .019), those with dysmenorrhea (p = .000), and those with anemia (p = .000), and the difference between groups was statistically significant.
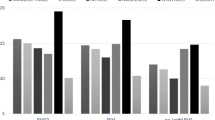
PMSS scores of university students
The total mean score of PMSS in the study was 140.68 ± 34.69, and the mean score of the subscales of PMSS are as follows: 24.54 ± 6.37 in depressive feelings, 18.89 ± 6.69 in anxiety, 20.91 ± 5.77 in fatigue, 17.54 ± 5.12 in irritability, 20.94 ± 7.32 in depressive thoughts, 9.46 ± 3.02 in pain, 9.73 ± 3.56 in changes in appetite, 8.96 ± 3.30 in changes in sleeping habits, 9.69 ± 3.57 in swelling (see Table 1).
PMS-Cope scores of university students
The total PMS-Cope mean score of the students in the study was 42.94 ± 8.72, and the mean scores from the PMS-Cope subscales were as follows: 17.67 ± 4.29 in “Seeking positive affect-inducing activities”, 13.21 ± 3.82 in “Seeking support” and 12.06 ± 3.30 in “Healthcare use behavior” (see Table 2).
Comparison of the PMS-Cope and subscale mean scores and PMSS and subscale scores of the university students
The proportions of university students experiencing premenstrual symptoms according to their scores higher than 50% in PMSS and its subscales are shown in Table 3. 80.5% of the students had depressive feelings, 59.5% anxiety, 83% fatigue, 82.5% irritability, 67.5% depressive thoughts, 74.8% pain, 71.5% changes in appetite, 68.9% changes in sleeping habits, and 70.1% swelling. According to the PMSS total score average (PMSS > 111 points), 80.5% of the students had severe premenstrual syndrome.
The comparison of the PMS-Cope total and sub-scales mean scores of university students with (PMSS > 111 points) and without PMS (PMSS < 110 points) revealed a statistically significant difference between the subscale of seeking positive affect-inducing activities and sub-scales of anxiety (p = .017), fatigue (p = .011), irritability (p = .002), depressive feelings (p = .000), pain (p = .029), and changes in sleeping habits (p = .023) (see Table 3). The difference between the sub-scale of seeking support and depressive thoughts (p = .002), fatigue (p = .032), irritability (p = .042), and total PMSS (p = .013) scores were also found to be statistically significant. There was a statistically significant difference between the mean scores of the sub-scale of healthcare use behavior and anxiety (p = .019) and pain (p = .015). However, no statistically significant difference was observed between the PMS-Cope total and the PMSS sub-scales (p > .05) (Table 3).
The students with lower anxiety, fatigue, irritability, depressive thoughts, pain, and sleep changes had lower mean scores for seeking positive affect-inducing activities, which were statistically significantly high (p < .05). Seeking support mean scores of those with higher depressive thoughts, fatigue, irritability, and higher PMSS total score were statistically significantly high (p < .05). Healthcare use behavior of students with higher anxiety and pain mean scores were also statistically significantly high (p < .05) (see Table 3).
Correlations between PMSS and PMS-Cope and Subscales
As shown in Table 4, there was a negative significant correlation between the PMSS total score and the PMS-Cope sub-scales of “Seeking positive affect-inducing activities” (r=-.210, p < .01), but no significant correlation was found between “Healthcare use behavior” and the total scores of “Seeking Support” and the PMS Cope Scale (p > .05).
The PMS-Cope total score was negatively and weakly correlated with the PMSS sub-scales of “fatigue” (r=-.099) and “depressive thoughts” (r=-.104), (p < .05). “Seeking positive affect-inducing activities”, a subscale of the PMS-Cope, was found to have negative and significant correlations with depressive feelings (r=-.196), anxiety (r=-.159), fatigue (r=-.229), irritability (r=-.205), depressive thoughts (r=-.222), pain (r=-.124), and changes in sleeping habits (r=-.141) (p < .01), sub-scales of PMSS scale, but no significant correlation was with changes in appetite and swelling sub-scales (p > .05) (see Table 4).
PMS-Cope predictors of premenstrual syndrome among university students
The results shown in Table 5 suggest that only one of three independent variables of PMS-Cope significantly predicted premenstrual syndrome, with all variables explaining 25.10% of its variance. Seeking positive affect-inducing activities of PMS-Cope was one predictor for premenstrual syndrome (β = − 0.265, p < .001).
Discussion
The study showed that the mean PMSS score of university students was 140.68 ± 34.69, and the frequency of PMS was 80.5%. The prevalence of PMS among students was found to be 62% by Bakır and Yangın (2019), 58.1% by Topatan and Kahraman (2020), 58.1% by Erbil and Yücesoy (2021a), 48.75% by Saglam and Basar (2019), 55.5% by Celik et al. (2019), and %50.7 by Erbas and Altunbas (2021), %77.9 by Yüksekol (2021). Raval et al. (2016) reported 18.4% PMS in students in a study in India. The prevalence of PMS in university students was determined to be 68% by Syed et al. (2020) and 29.8% by Buddhabunyakan et al. (2017). The overall prevalence of women of reproductive age affected by PMS was 47.8% worldwide (Frey et al. 2020).
In our study, 80.5% of the university students had depressive feelings, 59.5% had anxiety, 83% had fatigue, 82.5% had irritability, 67.5% had depressive thoughts, 74.8% had pain, 71.5% had changes in appetite, 68.9% had changes in sleeping habits, and 70.1% had swelling in the premenstrual period. Erbil and Yücesoy (2021a) used the same PMSS in our study and obtained the data on university students as follows; depressive feeling 62.6%, anxiety 28.4%, fatigue 64.2%, irritability 61.7%, depressive thoughts 39.6%, pain 59.1%, changes in appetite 72.8%, changes in sleeping habits 51.4%, and swelling 61%. Bakır and Kızılkaya Beji (2021) found 65.5% fatigue, 64.9% irritability, 63.1% changes in appetite, 60.1% depressive feelings, 59.5% pain, 58.0% swelling, 50.5% changes in sleeping habits, 44.7% depressive thoughts, 34.8% anxiety. Chumpalova et al. (2020) listed the top PMS symptoms as irritability, fatigue and appetite changes, depressive feelings, mood swings, and anxiety, respectively. Bilir et al. (2020) reported that more than 70% of university students experience PMS symptoms and the most common symptom is anger outburst, which negatively affects social life, and Deshpande et al. (2019) indicated that the most common PMS symptom was irritability with 60%. In this study, the rates of depressive feelings, depressive thoughts, and anxiety were higher than other study findings, which is thought to be due to the collection of data during the COVID-19 pandemic.
It was determined that the students’ PMS-Cope mean score was 42.94 ± 8.72, and the subscale of seeking positive affect-inducing activities was higher at 17.67 ± 4.29 (see Table 2). Positive affect-inducing activities in coping with PMS include personal orientations such as spending time with things they enjoy, distracting themselves, inducing positive feelings, making time for hobbies, exercising, applying a hot water bottle, and meeting friends. Cevik and Alan (2021) found that students exhibited positive behaviors to prevent PMS, while Erbas and Altunbas (2021) indicated that students used heat treatment and medication to cope with PMS symptoms. Obtaining significant results in different sub-scales of the PMS-Cope scale may be associated with students’ having different coping methods.
It was found that the students who experienced intense symptoms of anxiety, fatigue, irritability, depressive thoughts, pain, and sleep changes during the premenstrual period had a statistically significantly higher PMS-Cope mean score for seeking positive affect-inducing activities than other students. (p < .05), (see Table 3). Chae et al. (2017) found that students show more interest in coping methods and cope better with PMS when PMS symptoms are severe.
Our study showed that students with high rates of depressive affect, fatigue, irritability, and total PMS were more likely to seek support. Strategies for symptoms in the support-seeking subscale include talking with friends, looking for advice and support, seeking comfort and understanding, and exchanging views. On the other hand, Chae et al. (2017) detected a significant relationship between the increase in the social support network and PMS, but it does not have a significant effect on coping with PMS.
In this study, it was found that the depressive, tired and irritable nature of the students led them to seek social support. Buddhabunyakan et al. (2017) stated that the participants received advice from their friends (33.9%) and parents (22.8%) in coping with PMS symptoms. Aperribai and Alonso-Arbiol (2020) found that students with PMS showed more mood symptoms, and they coped with PMS by getting help and advice from the people around them. Studies suggest that social support may affect coping with PMS, and the relationship between social support, PMS, and coping with PMS needs to be clarified.
Unpleasant experiences related to PMS can negatively affect the behavioral dimension of coping with PMS and create an important cause of stress (Chae et al., 2017). In this study, students with higher anxiety and pain scores had significantly higher healthcare use behavior (P < .05). Students with anxiety and pain are more likely to look for information, try different alternative treatments, take medication, and avoid certain foods (see Table 3). In the study by Topatan and Kahraman (2020), 47.2% of the students experienced dysmenorrhea, 13.9% could not cope with dysmenorrhea, 37.1% could cope with it using analgesics, and 19.6% by keeping their feet warm. Findings for students to cope with pain by using analgesics are consistent with the literature (18.1%).
As the severity of PMS increases in young girls, negative attitudes toward coping may increase (Sonmezer & Yosmaoglu, 2014), and physiological factors can directly affect PMS (Chae et al., 2017). In this study, there was a negative significant correlation between the PMS-Cope total score average and the PMSS sub-scales of “fatigue” and “depressive thoughts” (p < .05), and there was a negative and significant correlation between the PMS total mean score and the PMS-Cope sub-scale “seeking positive affect-inducing activities” (p < .01) (see Table 4). Ascı et al. (2015) argued that more frequent symptoms of swelling, fatigue, irritability, depressive thoughts, and depressive feelings in the premenstrual period are associated with negative menstrual attitudes. It was observed in our study that as the fatigue and depressive thoughts of the students increased, their level of coping with PMS decreased, and the symptoms were more severe. The existence of fatigue and depressive thoughts negatively shapes the attitude towards menstruation in students and worsens PMS. Topatan and Kahraman (2020) stated that 46.4% of the students experienced symptoms of fatigue, 16.1% could not cope with this symptom, and 40.1% could cope with PMS by sleeping and 36.5% by resting. In this study, as the symptoms of depressive feelings, anxiety, fatigue, irritability, depressive thoughts, pain, and changes in sleeping habits increased, students’ practices for seeking positive affect-inducing activities coping with PMS decreased (see Table 4). Differences in coping strategies with PMS can be explained by university students’ different approaches to symptoms due to their social and cultural beliefs.
Seeking positive affect-inducing activities to cope with PMS according to the standardized regression coefficient (β) was found to be a significant predictor of premenstrual syndrome in our study (β=-0.265, p < .001) (see Table 5). Chae et al. (2017) identified the physiological factor as a significant predictor of premenstrual syndrome. Aperribai and Alonso-Arbiol (2020) determined depression and the use of social support as predictors in the linear regression analysis. Since few studies have investigated the relationship between coping with premenstrual syndrome and PMS, a direct comparison could not be made.
Limitations
Our study has several limitations. First, female students’ premenstrual symptoms were determined not by clinical examination, but by self-reported application of the PMSS scale. Retrospective surveys are not the most effective way to gather information on PMS symptoms. Second, students from only two faculties of the university were recruited for the study. Third, the data were collected online as universities shifted from onsite learning to online education during the COVID-19 pandemic, which had a significant somatic and psychological impact on the perceived stress of students in the study population. Therefore, it can complicate the relationship of perceived stress to PMS symptoms and socio-environmental conditions caused by the pandemic. Fourth, the PMS subgroup may be confused by students with similar conditions at other stages of the menstrual syndrome. Finally, there was a paucity of literature about the researched subject. Considering all these reasons, the results of the research are limited to the people participating in the research and cannot be generalized to the entire population.
Conclusion
Our study revealed evidence of premenstrual syndrome by identifying the frequency of PMS, the severity of PMS, the behaviors that positively affect coping mechanisms, and the symptoms it affects in female university students. The frequency of premenstrual syndrome was 80.5% in university students, and as seeking positive affect-inducing activities to cope with PMS decreased, depressive feelings, anxiety, fatigue, irritability, depressive thoughts, pain, and changes in sleeping habits increased. Students with high depressive thoughts, fatigue, irritability, and PMSS total score seek more support, and those with high anxiety and pain tend to use health care. Seeking positive affect-inducing activities to cope with PMS was determined to be a predictor of premenstrual syndrome.
PMS is a syndrome that needs to be handled meticulously, affecting the health and economy of not only individuals but also countries. Despite the remarkable prevalence of PMS, many professionals are still unaware of the impact it has on individuals, their families and communities, and the issue has little or no coverage by government bodies, particularly in developing countries. It is pivotal to develop strategies for university students to cope with PMS and provide personalized care. In coping with PMS, it is necessary to consider the perceptions of taking medication, seeking social support, or seeking positive affect-inducing activities as a coping method to determine the social and cultural beliefs of university students and to control PMS. As role models for various categories of people, health professionals are one of the most significant occupational groups in promoting community health.
Since PMS is a significant health problem, it is not enough to just raise awareness about the issue. Once health experts are informed about the issue, they should counsel women and educate university students. To provide quality treatment to society, nursing students, who are among the future health professionals, can also benefit the economy of their nation. The public benefits greatly from teaching students how to deal with PMS and promoting awareness and understanding of the onset and treatment of premenstrual distress. The health team can organize training for students on behaviors that positively affect coping with PMS, make suggestions, and offer counseling on how to make coping methods a lifestyle. Students can be advised on personal orientations and behaviors that positively affect PMSS such as spending time doing things they enjoy, distracting themselves, thinking positively, spending time on hobbies, increasing movement, creating exercise programs, applying heat in times of pain, and spending time with loved ones. University students with PMS and PMDD symptoms may be given exercise interventions by professionals from a variety of disciplinary backgrounds, including group exercise leaders, personal trainers, clinical exercise physiologists, healthcare professionals, and physical therapists. It should also be noted that the severity of PMS and women’s strategies for coping with symptoms and their effectiveness may differ between ethnic groups and cultures.
PMS is a global public health problem that adversely affects university students. As PMS and PMDD place a significant burden on women’s well-being, both are issues that require the intervention of healthcare professionals. It is recommended to determine the frequency of PMS in university students with PMS screening programs and carry out further research on the planning and implementation of attempts by healthcare professionals to cope with PMS.
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
References
American Psychiatric Association. (2013). Diagnostic and statistical Manual of Mental Disorders (5th ed.). Washington (DC): American Psychiatric Association.
Aperribai, L., & Alonso-Arbiol, I. (2020). The role of mental health variables and coping strategies in premenstrual syndrome. Health Care for Women International, 41(3), 368–379. https://doi.org/10.1080/07399332.2019.1663193
Aşcı, Ö., Gökdemir, F., Süt, K., H., & Payam, F. (2015). The relationship of Premenstrual syndrome symptoms with menstrual attitude and sleep quality in turkish nursing student. Journal of Caring Sciences, 4(3), 179–187. https://doi.org/10.15171/jcs.2015.018
Bakır, N., & Kızılkaya Beji, N. (2021). Premenstrual Syndrome Prevalence and affecting factors among University students. Journal of Vocational School of Health Service, 9(1), 264–277. https://doi.org/10.33715/inonusaglik.835785
Bakır, N., & Yangın, H. B. (2019). The relationship between premenstrual syndrome and healthy lifestyle among university students. Life Skills Journal of Psychology, 3(5), 39–51. https://doi.org/10.31461/ybpd.538946
Başoğul, C., Aydın Özkan, S., & Karaca, T. (2020). The effects of psychoeducation based on the cognitive-behavioral approach on premenstrual syndrome symptoms: a randomized controlled trial. Perspectives in Psychiatric Care, 56(3), 515–522. https://doi.org/10.1111/ppc.12460
Belvederi Murri, M., Ekkekakis, P., Magagnoli, M., Zampogna, D., Cattedra, S., Capobianco, L., Serafini, G., Calcagno, P., Zanetidou, S., & Amore, M. (2019). Physical Exercise in Major Depression: reducing the mortality gap while improving clinical outcomes. Frontiers in Psychiatry, 9, 762. https://doi.org/10.3389/fpsyt.2018.00762
Bilir, E., Yıldız, Ş., Yakın, K., & Ata, B. (2020). The impact of dysmenorrhea and premenstrual syndrome on academic performance of college students, and their willingness to seek help. Turkish Journal of Obstetrics and Gynecology, 17(3), 196–201. https://doi.org/10.4274/tjod.galenos.2020.97266
Buddhabunyakan, N., Kaewrudee, S., Chongsomchai, C., Soontrapa, S., Somboonporn, W., & Sothornwit, J. (2017). Premenstrual syndrome (PMS) among high school students. International Journal of Women’s Health, 9, 501–505. https://doi.org/10.2147/IJWH.S140679
Bhuvaneswari, K., Rabindran, P., & Bharadwaj, B. (2019). Prevalence of premenstrual syndrome and its impact on quality of life among selected college students in Puducherry. The National Medical Journal of India, 32(1), 17–19. https://doi.org/10.4103/0970-258X.272109
Cha, C., & Nam, S. J. (2016). Premenstrual symptom clusters and women’s coping style in Korea: happy healthy 20s application study. Journal of Psychosomatic Obstetrics and Gynaecology, 37(3), 91–100. https://doi.org/10.3109/0167482X.2016.1157159
Chae, M. O., Jeon, H. O., & Kim, A. (2017). A structural model for Premenstrual Coping in University students: based on Biopsychosocial Model. Journal of Korean Academy of Nursing, 47(2), 257–266. https://doi.org/10.4040/jkan.2017.47.2.257
Chumpalova, P., Iakimova, R., Stoimenova-Popova, M., Aptalidis, D., Pandova, M., Stoyanova, M., & Fountoulakis, K. N. (2020). Prevalence and clinical picture of premenstrual syndrome in females from Bulgaria. Annals of General Psychiatry, 19, 3. https://doi.org/10.1186/s12991-019-0255-1
Celik, M. Y., Polat, Y., & Yıldırım, A. D. (2019). Premenstrual syndrome prevalence in students and comparison of life satisfaction scale scores and premenstrual syndrome scale scores of students. Health and Society, 29(2), 50–57.
Cevik, A., & Alan, S. (2021). Determining the relationship between midwifery students’ frequency of experiencing Premenstrual syndrome and perceived stress level. Mersin University School of Medicine Lokman Hekim Journal of History of Medicine and Folk Medicine, 11(1), 104–113. https://doi.org/10.31020/mutftd.781048
Dadkhah, H., Ebrahimi, E., & Fathizadeh, N. (2016). Evaluating the effects of vitamin D and vitamin E supplement on premenstrual syndrome: a randomized, double-blind, controlled trial. Iranian Journal of Nursing and Midwifery Research, 21(2), 159–164. https://doi.org/10.4103/1735-9066.178237
Deshpande, S. R., Vaishampayan, N. R., Bevinamarad, S. B., & Patil, S. R. (2019). Assessment of prevalence and awareness regarding premenstrual syndrome and its coping techniques among the paramedical students–A research study. International Journal of Medical Science and Public Health, 8(11), 893–896. https://doi.org/10.5455/ijmsph.2019.0719801082019
Direkvand-Moghadam, A., Sayehmiri, K., Delpisheh, A., & Kaikhavandi, S. (2014). Epidemiology of premenstrual syndrome (PMS)-a systematic review and meta-analysis study. Journal of Clinical and Diagnostic Research, 8(2), 106–109. https://doi.org/10.7860/JCDR/2014/8024.4021
Dönmez, S., & Gümüssoy, S. (2019). Premenstrual Syndrome in Nursing Students and The Affecting Factors. Kocaeli Medical Journal, 8(2), 38–45. https://doi.org/10.5505/ktd. 2019.46873
Dutta, A., & Sharma, A. (2021). Prevalence of premenstrual syndrome and premenstrual dysphoric disorder in India: a systematic review and meta-analysis. Health Promotion Perspectives, 19(2), 161–170. https://doi.org/10.34172/hpp.2021.20
Erbas, N., & Altunbas, N. (2021). According to some variables in girls a high school determining the premenstrual syndrome violence and perceped stress level. Acıbadem University Health Sciences Journal, 2, 479–486. https://doi.org/10.31067/acusaglik.849971
Erbil, N., & Yücesoy, H. (2021a). Relationship between premenstrual syndrome and sleep quality among nursing and medical students. Perspective in Psychiatric Care, 58(2), 448–455. https://doi.org/10.1111/ppc.12628
Erbil, N., & Yücesoy, H. (2021b). Premenstrual syndrome prevalence in Turkey: a systematic review and meta-analysis. Psychology Health & Medicine, 1–11. https://doi.org/10.1080/13548506.2021.2013509. Advance online publication.
Eshetu, N., Abebe, H., Fikadu, E., Getaye, S., Jemal, S., Geze, S., Mesfin, Y., Abebe, S., Tsega, D., Tefera, B., & Tesfaye, W. (2022). Premenstrual syndrome, coping mechanisms and associated factors among Wolkite university female regular students, Ethiopia, 2021. BMC Women’s Health, 22(1), 88. https://doi.org/10.1186/s12905-022-01658-5
Fatemi, M., Allahdadian, M., & Bahadorani, M. (2019). Comparison of serum level of some trace elements and vitamin D between patients with premenstrual syndrome and normal controls: a cross-sectional study. International Journal of Reproductive Biomedicine, 17(9), 647–652. https://doi.org/10.18502/ijrm.v17i9.5100
Frey Nascimento, A., Gaab, J., Kirsch, I., Kossowsky, J., Meyer, A., & Locher, C. (2020). Open-label placebo treatment of women with premenstrual syndrome: study protocol of a randomised controlled trial. British Medical Journal Open, 10(2), e032868. https://doi.org/10.1136/bmjopen-2019-032868
Forrester-Knauss, C., Zemp Stutz, E., Weiss, C., & Tschudin, S. (2011). The interrelation between premenstrual syndrome and major depression: results from a population-based sample. Bmc Public Health, 11, 795. https://doi.org/10.1186/1471-2458-11-795
Gencdogan, B. A. (2006). New instrument for premenstrual syndrome. Psychiatry in Turkey, 8(2), 81–87.
Geta, T. G., Woldeamanuel, G. G., & Dassa, T. T. (2020). Prevalence and associated factors of premenstrual syndrome among women of the reproductive age group in Ethiopia: systematic review and meta-analysis. PloS One, 15(11), e0241702. https://doi.org/10.1371/journal.pone.0241702
Izadi-Mazidi, M., Davoudi, I., & Mehrabizadeh, M. (2016). Effect of Group cognitive-behavioral therapy on Health-Related quality of life in females with Premenstrual Syndrome. Iranian Journal of Psychiatry and Behavioral Sciences, 10(1), e4961. https://doi.org/10.17795/ijpbs-4961
Kaiser, G., Kues, J. N., Kleinstäuber, M., Andersson, G., & Weise, C. (2018). Methods for coping with premenstrual change: development and validation of the german Premenstrual Change Coping Inventory. Women & Health, 58(9), 1062–1079. https://doi.org/10.1080/03630242.2017.1377802
Kelderhouse, K., & Taylor, J. S. (2013). A review of treatment and management modalities for premenstrual dysphoric disorder. Nursing for Women’s Health, 17(4), 294–305. https://doi.org/10.1111/1751-486X.12048
Mizuta, R., Maeda, N., Komiya, M., Suzuki, Y., Tashiro, T., Kaneda, K., Tsutsumi, S., Ishihara, H., Kuroda, S., & Urabe, Y. (2022). The relationship between the severity of perimenstrual symptoms and a regular exercise habit in japanese young women: a cross-sectional online survey. BMC Women’s Health, 22(1), 200. https://doi.org/10.1186/s12905-022-01720-2
Mumtaz, T., Roohi, N., & Iqbal, M. A. (2018). A census of premenstrual syndrome in young adolescent girls: facts about women health in developing country. Medical Reports & Case Studies, 3(2), 1–5. https://doi.org/10.4172/2572-5130.1000159
Petersen, N., London, E. D., Liang, L., Ghahremani, D. G., Gerards, R., Goldman, L., & Rapkin, A. J. (2016). Emotion regulation in women with premenstrual dysphoric disorder. Archives of Women’s Mental Health, 19(5), 891–898. https://doi.org/10.1007/s00737-016-0634-4
Pilver, C. E., Libby, D. J., & Hoff, R. A. (2013). Premenstrual dysphoric disorder as a correlate of suicidal ideation, plans, and attempts among a nationally representative sample. Social Psychiatry and Psychiatric Epidemiology, 48(3), 437–446. https://doi.org/10.1007/s00127-012-0548-z
Prasad, D., Wollenhaupt-Aguiar, B., Kidd, K. N., de Azevedo Cardoso, T., & Frey, B. N. (2021). Suicidal risk in women with Premenstrual Syndrome and Premenstrual Dysphoric disorder: a systematic review and Meta-analysis. Journal of Women’s Health (2002), 30(12), 1693–1707. https://doi.org/10.1089/jwh.2021.0185
Ramya, S. K., & Bupathy, A. (2014). Effect of educational program on premenstrual syndrome in adolescent schoolgirls. International Journal of Reproduction Contraception Obstetrics and Gynecology, 3(1), 168–171. https://doi.org/10.5455/2320-1770.ijrcog20140333
Raval, C. M., Panchal, B. N., Tiwari, D. S., Vala, A. U., & Bhatt, R. B. (2016). Prevalence of premenstrual syndrome and premenstrual dysphoric disorder among college students of Bhavnagar, Gujarat. Indian Journal of Psychiatry, 58(2), 164–170. https://doi.org/10.4103/0019-5545.183796
Ryu, A., & Kim, T. H. (2015). Premenstrual syndrome: a mini review. Maturitas, 82(4), 436–440. https://doi.org/10.1016/j.maturitas.2015.08.010
Saglam, H. Y., & Basar, F. (2019). The relationship between premenstrual syndrome and anger. Pakistan Journal of Medical Sciences, 35(2), 515–520. https://doi.org/10.12669/pjms.35.2.232
Sarı Çetin, H., & Erbil, N. (2020). Turkish validity and reliability of the Premenstrual Change Coping Inventory. Virtual Congress Proceedings Book, 1st National Women Health Congress, Haliç University, İstanbul, Turkey.
Shams-Alizadeh, N., Maroufi, A., Rashidi, M., Roshani, D., Farhadifar, F., & Khazaie, H. (2018). Premenstrual dysphoric disorder and suicide attempts as a correlation among women in reproductive age. Asian Journal of Psychiatry, 31, 63–66. https://doi.org/10.1016/j.ajp.2018.01.003
Shrestha, D. B., Shrestha, S., Dangol, D., Aryal, B. B., Shrestha, S., Sapkota, B., & Rai, S. (2019). Premenstrual Syndrome in students of a Teaching Hospital. Journal of Nepal Health Research Council, 17(2), 253–257. https://doi.org/10.33314/jnhrc.v0i0.1213
Sonmezer, E., & Yosmaoglu, H. B. (2014). Changes of menstrual attitude and stress perception in women with dysmenorrheal. Turkish Journal of Physiotherapy and Rehabilitation, 25(2), 56–62. https://doi.org/10.21653/tfrd.156458
Stoner, R., Camilleri, V., Calleja-Agius, J., & Schembri-Wismayer, P. (2017). The cytokine-hormone axis - the link between premenstrual syndrome and postpartum depression. Gynecological endocrinology: the official journal of the International Society of Gynecological Endocrinology, 33(8), 588–592. https://doi.org/10.1080/09513590.2017.1318367
Syed, A., & Rao, S. B. (2020). Prevalence of premenstrual syndrome and dysmenorrhea among medical students and its impact on their college absenteeism. International Journal of Reproduction Contraception Obstetrics and Gynecology, 9(4), 1377–1382. https://doi.org/10.18203/2320-1770.ijrcog20201042
Tolossa, F. W., & Bekele, M. L. (2014). Prevalence, impacts and medical managements of premenstrual syndrome among female students: cross-sectional study in College of Health Sciences, Mekelle University, Mekelle, northern Ethiopia. BMC Women’s Health, 14, 52. https://doi.org/10.1186/1472-6874-14-52
Topatan, S., & Kahraman, Ş. (2020). The methods they applied for coping and the quality of life of university students living the premenstrual syndrome. Journal of Anatolia Nursing and Health Sciences, 23(1), 35–44. https://doi.org/10.17049/ataunihem.481238
Wu, M., Liang, Y., Wang, Q., Zhao, Y., & Zhou, R. (2016). Emotion dysregulation of women with Premenstrual Syndrome. Scientific Reports, 6, 38501. https://doi.org/10.1038/srep38501
Yesildere Saglam, H., & Orsal, O. (2020). Effect of exercise on premenstrual symptoms: a systematic review. Complementary Therapies in Medicine, 48, 102272. https://doi.org/10.1016/j.ctim.2019.102272
Yonkers, K. A., & Simoni, M. K. (2018). Premenstrual disorders. American Journal of Obstetrics and Gynecology, 218(1), 68–74. https://doi.org/10.1016/j.ajog.2017.05.045
Yüksekol, O. D., Kaya, Z., & Nazik, F. (2021). Investigation of the relationship between Premenstrual Syndrome and Covid-19 psychological distress in nursing students. Turkish Journal of Science and Health, 2(3), 45–55. https://doi.org/10.51972/tfsd.984461
Acknowledgements
The authors would like to thank all students participating in the study.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
Authors contributed the study conception and design. Material preparation, and analysis were performed by Özlem Akın and Nülüfer Erbil. Data collection was performed Özlem Akın. The manuscript was written by Özlem Akın and Nülüfer Erbil. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no actual or potential conflicts of interest.
Financial interests
The authors declare they have no financial interests.
Ethical approval
Permission was obtained from the authors who conducted the validity and reliability study of the scales used in the study. Written permission was received from the School of Health and the Faculty of Arts and Sciences, where the research was conducted. Ethics committee approval was obtained from the Recep Tayyip Erdogan University Faculty of Medicine Non-Interventional Clinical Research Ethics Committee for ethical compliance in the study (21/04/2020 dated 2020/42). Informed consent was obtained from the students who agreed to participate in the study. The principles of the Declaration of Helsinki were followed during the research.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Akın, Ö., Erbil, N. Investigation of coping behaviors and premenstrual syndrome among university students. Curr Psychol 43, 1685–1695 (2024). https://doi.org/10.1007/s12144-023-04419-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12144-023-04419-1