Abstract
Objective
To estimate the burden of undernutrition and its association with rotavirus positivity among under-five children admitted with diarrhea.
Methods
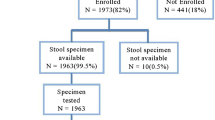
This prospective observational study was carried out in hospital-setting from February 2016 to January 2020. For all cases who met the eligibility criteria, an informed written consent was obtained from parents/caregivers. A case report form was used to collect sociodemographic, anthropometric and clinical data. The anthropometric measurements of children were performed according to World Health Organization (WHO) guidelines.
Results
Nutritional assessment revealed that 74.1% study subjects were underweight [Weight-for-Age (WAZ) < −2], 59% were stunted [Height-for-Age (HAZ), < −2] and 52.3% were wasted Body Mass Index (BMIZ) < −2]. Stunting was found to be significantly higher among boys as compared to girls and rotavirus positive diarrhea was significantly less prevalent among stunted children.
Conclusion
There exists a very high prevalence of underweight, stunting, and wasting among hospitalized children with diarrhea. As the better nutrition has not been shown to guard against rotavirus diarrhea, coverage scale-up of rotavirus vaccination, improved hygiene and sanitation, and focussed nutrition programmes are the need of the hour in India.
Similar content being viewed by others
References
Walker CL, Rudan I, Liu L, et al. Global burden of child- hood pneumonia and diarrhoea. Lancet. 2013;381:1405–16. https://doi.org/10.1016/S0140-6736(13)60222-6 PMID: 23582727
United Nations Children’s Fund. Levels and trends in child mortality, 2011 report. [Internet] New York: UNICEF; 2011. Available at: https://www.unicef.org/media/files/Child_Mortality_Report_2011_Final.pdf. Accessed 16 Nov 2020.
Liu L, Johnson HL, Cousens S, et al. Child Health Epidemiology Reference Group of WHO and UNICEF. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet. 2012;379(9832):2151–61. doi: https://doi.org/10.1016/S0140-6736(12)60560-1. Epub 2012 May 11. Erratum in: Lancet. 2012;380(9850):1308.
World Health Organization. World health statistics 2018: monitoring health for the SDGs. [Internet] Geneva: World Health Organization; 2018. Available at: http://apps.who.int/iris/bitstream/handle/10665/272596/9789241565585-eng.pdf?ua=1. Accessed 26 Oct 2020.
Tate JE, Burton AH, Boschi-Pinto C, Parashar UD. Global, regional, and national estimates of rotavirus mortality in children <5 years of age, 2000-2013. Clin Infect Dis. 2016;62:S96–105.
Black RE, Victora CG, Walker SP, et al. Maternal and child malnutrition and overweight in low-income and middle- income countries. Lancet. 2013;382:427–51. https://doi.org/10.1016/S0140-6736(13)60937-X.
Guerrant RL, Oria RB, Moore SR, Oria MO, Lima AA. Malnutrition as an enteric infectious disease with long-term effects on child development. Nutr Rev. 2008;66:487–505. https://doi.org/10.1111/j.1753-4887.2008.00082.x PMID: 18752473
International Institute for Population Sciences. National Family Health Survey (NFHS-4), 2015–16, India Fact Sheet. [Internet] Mumbai: IIPS; 2017. Available at: http://rchiips.org/nfhs/factsheet_NFHS-4.shtml. Accessed 05 Jul 2020.
International Institute for Population Sciences. National Family Health Survey (NFHS-3), 2005–06, India Fact Sheet. [Internet] Mumbai: IIPS; 2007. Available at: http://www.rchiips.org/nfhs/report.shtml. Accessed 05 Jul 2020.
Neumann CG, Gewa C, Bwibo NO. Child nutrition in developing countries. Pediatr Ann. 2004;33:658–674. PMID: 15515353
Martorell R, Yarbrough C, Yarbrough S, Klein RE. The impact of ordinary illnesses on the dietary intakes of mal-nourished children. Am J Clin Nutr. 1980;33:345–50. https://doi.org/10.1093/ajcn/33.2.345.
Verkerke H, Sobuz S, Ma JZ, et al. Malnutrition is associated with protection from rotavirus diarrhea: evidence from a longitudinal birth cohort study in Bangladesh. J Clin Microbiol. 2016;54:2568–74. https://doi.org/10.1128/JCM.00916-16.
Nair NP, Reddy NS, Giri S, et al. Rotavirus vaccine impact assessment surveillance in India: protocol and methods. BMJ Open. 2019;9(4):e024840. doi: https://doi.org/10.1136/bmjopen-2018-024840. PMID: 31028037; PMCID: PMC6502045.
Kliegman R, Behrman RE, Nelson WE. Nelson Textbook of Pediatrics, Vol 2, 20th ed. Philadelphia, PA: Elsevier; 2016.
World Health Organization. Expert committee on nutrition and physical status: uses and interpretation of anthropometry. Geneva: World Health Organization; 1995.
World Health Organization. The WHO Anthro Survey Analyser Tool. Geneva: WHO; 2019. Available at: https://worldhealthorg.shinyapps.io/anthro/. Accessed 21 Nov 2020.
NITI Aayog, Government of India. Deep Dive: Insights from Champions of Change, the Aspirational Districts Dashboard. [Internet] New Delhi: NITI Aayog, Government of India; 2018. Available at: http://niti.gov.in/writereaddata/files/FirstDeltaRanking-May2018-AspirationalRanking.pdf. Accessed 27 Jan 2020.
United Nations Children’s Fund. The state of the world’s children 2014 in numbers every child counts. [Internet] New York: UNICEF; 2014. Available at: https://www.unicef.org/publications/files/SOWC2014_In_Numbers_28_Jan.pdf. Accessed 11 Nov 2020.
International Institute for Population Sciences. National Family Health Survey-4, 2015–16: District Fact Sheet Mewat Haryana. [Internet] Mumbai: IIPS; 2017. Available at: http://rchiips.org/nfhs/FCTS/HR/HR_FactSheet_87_Mewat.pdf. Accessed 05 Nov 2020.
Bisai S, Bose K, Ghosh A. Nutritional status of Lodha children in a village of Paschim Medinipur district, West Bengal. Indian J Public Health. 2008;52(4):203–6.
Marcoux A. Sex differentials in undernutrition: a look at survey evidence. Popul Dev Rev. 2002;28(2):275–84.
Gupta V, Chawla S, Mohapatra D. Nutritional assessment among children (1–5 years of age) using various anthropometric indices in a rural area of Haryana, India. Indian J Community Fam Med. 2019;5:39–43.
Koyuncu A, Simuyandi M, Bosomprah S, Chilengi R. Nutritional status, environmental enteric dysfunction, and prevalence of rotavirus diarrhoea among children in Zambia. PLoS One. 2020;15(10):e0240258. https://doi.org/10.1371/journal.pone.0240258.
Mpabalwani M, Oshitani H, Kasolo F, et al. Rotavirus gastro-enteritis in hospitalized children with acute diarrhoea in Zambia. Ann Trop Paediatr. 1995;15:39–43. https://doi.org/10.1080/02724936.1995.11747747 PMID: 7598436
Das SK, Chisti MJ, Huq S, et al. Clinical characteristics, etiology and antimicrobial susceptibility among overweight and obese individuals with diarrhea: observed at a large diarrheal disease hospital, Bangladesh. PLoS One. 2013;8:e70402. https://doi.org/10.1371/journal.pone.0070402.
Kotloff KL, Nataro JP, Blackwelder WC, et al. Burden and aetiology of diarrhoeal disease in infants and young children in developing countries (the global enteric multicenter study, GEMS): a prospective, case-control study. Lancet. 2013;382(9888):209–22. https://doi.org/10.1016/S0140-6736(13)60844-2 Epub 2013 May 14.
Tickell KD, Sharmin R, Deichsel EL, et al. The effect of acute malnutrition on enteric pathogens, moderate-to-severe diarrhoea, and associated mortality in the Global Enteric Multicenter Study cohort: a post-hoc analysis. Lancet Glob Health. 2020;8(2):e215–24. doi: https://doi.org/10.1016/S2214-109X(19)30498-X. PMID: 31981554; PMCID: PMC7025322.
Acknowledgments
The authors acknowledge the support of Indian Council of Medical Research, New Delhi; Ministry of Health and Family Welfare, Government of India and the Government of Haryana. The authors thank the team at Christian Medical College, Vellore for support, and the children and families for participation.
Funding
This project was funded by grants from the Bill and Melinda Gates Foundation to the Centers for Disease Control and Prevention (CDC), Atlanta, USA (subcontract to Christian Medical College, Vellore grant no MOA#871-15SC) and the Translational Health Science and Technology Institute, Faridabad, India (grant no OPP1165083).
Author information
Authors and Affiliations
Contributions
SC and AKG conceptualized and designed the study; SC and AKG collected the data and drafted the paper; AKG supervized the laboratory work and provided critical inputs; VT and NPN cleaned and analyzed the data. All authors approved the final manuscript. SC will act as guarantor for this paper.
Corresponding author
Ethics declarations
Ethical Clearance
The study was approved by institutional ethics committee of SHKM Government Medical College, Nalhar, Nuh, Haryana.
Conflict of Interest
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chawla, S., Goel, A.K., Thiyagarajan, V. et al. Nutritional Assessment and its Association with Rotavirus Positivity Among Under Five Children Admitted with Diarrhea in a Tertiary Care Hospital of Southern Haryana, India. Indian J Pediatr 88 (Suppl 1), 138–143 (2021). https://doi.org/10.1007/s12098-020-03611-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-020-03611-6