Abstract
Objective
To identify baseline risk factors for prolonged diarrheal duration and subsequent complications in children aged 6 to 59 mo with acute diarrhea who participated in a micronutrient clinical trial in a tertiary care hospital.
Methods
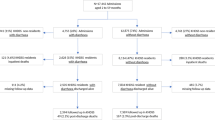
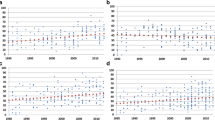
The adjusted odds ratio or incidence risk ratios (IRR) of the baseline variables for prolongation of diarrheal duration (cox proportional hazard model), diarrhea >7 d (multiple logistic regressions), severe dehydration experienced after hospitalization (poisson regression models) was estimated.
Results
Fever (OR 1.10, 95% CI 1.02–1.19, p = 0.02), dehydration (OR 1.32, 95% CI 1.10–1.59, p = 0.003), dysentery (OR 1.41 95% CI 1.09–1.82, p = 0.008), those who received medications (OR 1.19, 95% CI 1.03–1.39, p = 0.02), and weight for age Z-score ≤2 (OR 1.25, 95% CI 1.07–1.46, p = 0.004) were at a greater risk of prolonged diarrhea. Diarrhea >7 d was associated with younger age (OR 1.08, 95% CI 1.03–1.14, p = 0.003), female child (OR 2.33, 95% CI 1.19–4.55, p = 0.013), diarrheal duration before enrolment (OR 1.06, 95% CI 1.04–1.09, p < 0.001), fever (OR 1.7, 95% CI 1.23–2.49, p = 0.002) and the weight for age Z-score ≤2 (OR 4.32, 95% CI 2.03–9.16, p < 0.001). Severe dehydration after hospitalization was associated with dehydration at baseline (OR 6.7, 95% CI 2–3.0, p < 0.001), incomplete immunization (OR 3.33, 95% CI 1.5–7.69, p < 0.001), failure to receive any medication(OR 3.03, 95% CI 1.26–7.14, p = 0.01).
Conclusions
Few studies assess risk factors for diarrheal morbidity prospectively. The present study showed that children of acute diarrhea with above risk factors need stricter monitoring for complications to reduce diarrheal mortality.
Similar content being viewed by others
Abbreviations
- IV:
-
Intravenous
- ORS:
-
Oral rehydration solution
- Pl:
-
Placebo
- RH:
-
Relative hazards
- WHO:
-
World Health Organization
- Zn:
-
Zinc
- Zn+Cu:
-
Zinc and copper
References
Bryce J, Boschi-Pinto C, Shibuya K, Black RE, WHO Child Health Epidemiology Reference Group. WHO estimates of the causes of death in children. Lancet. 2005;365:1147–52.
Kosek M, Bern C, Guerrant RL. The global burden of diarrheal disease, as estimated from studies published between 1992 and 2000. Bull World Health Organ. 2003;81:197–204.
Keusch GT, Fontaine O, Boschi-Pinto C, Bhutta ZA, Gotuzzo E. Diarrheal diseases. In: Jamison JT, Measham AR, Alleyne G, et al., editors. Disease control priorities in developing countries. 2nd ed. Washington: World Bank; 2006. p. 371–87.
World Health Organization. Persistent diarrhea in children in developing countries: memoranda from a WHO meeting. Bull WHO. 1988;66:709–27.
World Health Organization WHO. Division of diarrheal and acute respiratory disease control. Rational management of diarrhea in children. Essent Drugs Monit. 1991;11:10–1.
International Institute for Population Sciences (IIPS) and ORC Macro. National Family Health Survey (NFHS-3), 2005–06: India. Mumbai: IIPS; 2006.
Gyimah S. Interaction effects of maternal education and household facilities on childhood diarrhea in Sub-Saharan Africa. J Health Popul Dev Ctries. 2003 (13 November, 2003).
Patel A, Dibley MJ, Mamtani M, Badhoniya N, Kulkarni H. Zinc and copper supplementation in acute diarrhea in children: a double-blind randomized controlled trial. BMC Med. 2009;7:22.
WHO. The treatment of diarrhea: a manual for physicians and other senior health workers. Vol. WHO/CDD/SER/80.2. Geneva: World Health Organization; 2005.
HemoCue Blood Hemoglobin Photometer Operating Manual. [http://www.hemocue.com/files/900138_GB.pdf].
Filmer D, Pritchett LH. Estimating wealth effects without expenditure data or tears: an application to educational enrolments in States of India. Demography. 2001;38:115–32.
WHO. WHO Anthro. 2005: Geneva, Switzerland.
Karim AS, Akhter S, Rahman MA, Nazir MF. Risk factors of persistent diarrhea in children below five years of age. Indian J Gastroenterol. 2001;20:59–61.
Façanha MC, Pinheiro AC. Acute diarrhea treated by health care services in Fortaleza, Ceará State, Brazil, from 1996 to 2001. Cad Saude Publica. 2005;21:49–54.
Thapa BR, Ventkateswarlu K, Malik AK, Panigrahi D. Shigellosis in children from north India: a clinicopathological study. J Trop Pediatr. 1995;41:303–7.
Uhnoo I, Olding-Stenkvist E, Kreuger A. Clinical features of acute gastroenteritis associated with rotavirus, enteric adenoviruses, and bacteria. Arch Dis Child. 1986;61:732–8.
Lins MD, Silva GA. Diarrheal disease in hospitalized children—importance of the persistent diarrhea. J Pediatr (Rio J). 2000;76:37–43.
Mach O, Lu L, Creek T, et al. Population-based study of a widespread outbreak of diarrhea associated with increased mortality and malnutrition in Botswana, January–March, 2006. Am J Trop Med Hyg. 2009;80:812–8.
Schmidt WP, Cairncross S, Barreto ML, Clasen T, Genser B. Recent diarrheal illness and risk of lower respiratory infections in children under the age of 5 years. Int J Epidemiol. 2009;38:766–72.
Riveron Corteguera R. Persistent diarrhea. Arch Domin Pediatr. 1993;29:58–62.
Patel AB, Dhande LA, Rawat MS. Therapeutic evaluation of zinc and copper supplementation in acute diarrhea in children: double blind randomized trial. Indian Pediatr. 2005;42:433–42.
Bhattacharya SK, Bhattacharya MK, Manna B, et al. Risk factors for development of dehydration in young children with acute watery diarrhea: a case-control study. Acta Paediatr. 1995;84:160–4.
Banerjee B, Hazra S, Bandyopadhyay D. Diarrhea management among under fives. Indian Pediatr. 2004;41:255–60.
Staat MA, Morrow AL, Reves RR, Bartlett AV, Pickering LK. Diarrhea in children newly enrolled in day-care centers in Houston. Pediatr Infect Dis J. 1991;10:282–6.
Cruz JR, Bartlett AV, Mendez H, Sibrian R. Epidemiology of persistent diarrhea among Guatemalan rural children. Acta Paediatr Suppl. 1992;381:22–6.
Zodpey SP, Deshpande SG, Ughade SN, Hinge AV, Shirikhande SN. Risk factors for development of dehydration in children aged under five who have acute watery diarrhea: a case-control study. Public Health. 1998;112:233–6.
El Samani FZ, Willett WC, Ware JH. Predictors of simple diarrhea in children under 5 years—a study of a Sudanese rural community. Soc Sci Med. 1989;29:1065–70.
Ahmed M, Billoo AG, Murtaza G. Risk factors of persistent diarrhea in children below five years of age. J Pak Med Assoc. 1995;45:290–2.
Acknowledgements
The authors extend their thanks to all the women, children and their families who participated in the trial, also thank the following members of the research team who contributed to the successful implementation of the study: Mr. Hussaini Ali and Mr. Gadkari (Universal Medicaments Pharmacists), Ms. Smita Puppulwar and Ms. Shubhangi Puranik. Authors are grateful to Prof. Catherine D’Este, Dr. AV Shrikhande and Dr. Nitin Kimmatkar, the members of the treatment effects monitoring committee, who reviewed the unexpected trial events and conducted an interim analysis. The project was supported by a Wellcome Trust Collaborative Research Initiative Grant (number 068664/Z/02/Z).
Contributions
AP:developed the study protocol, questionnaires and clinical trial procedures, directed the conduct of the trial, data analysis, data interpretation and wrote the first draft of the paper; RO: helped in reviewing literature, drafting and editing the paper; NB: helped with data analysis and editing the manuscript; MJD: contributed to the development of the protocol, helped in the development of study questionnaires and trial procedures, contributed to the data analysis, data interpretation and edited the paper. All authors reviewed drafts of the manuscript, read and approved the final draft.
Conflict of Interest
None.
Role of Funding Source
Wellcome Trust Collaborative Research Initiative Grant.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Patel, A.B., Ovung, R., Badhoniya, N.B. et al. Risk Factors for Predicting Diarrheal Duration and Morbidity in Children with Acute Diarrhea. Indian J Pediatr 79, 472–477 (2012). https://doi.org/10.1007/s12098-011-0561-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-011-0561-3