Abstract
Purpose
To better define outcome and prognostic factors in primary pineal tumors.
Materials and methods
Thirty-five consecutive patients from seven academic centers of the Rare Cancer Network diagnosed between 1988 and 2006 were included. Median age was 36 years. Surgical resection consisted of biopsy in 12 cases and resection in 21 (2 cases with unknown resection). All patients underwent radiotherapy and 12 patients received also chemotherapy.
Results
Histological subtypes were pineoblastoma (PNB) in 21 patients, pineocytoma (PC) in 8 patients and pineocytoma with intermediate differentiation in 6 patients. Six patients with PNB had evidence of spinal seeding. Fifteen patients relapsed (14 PNB and 1 PC) with PNB cases at higher risk (p = 0.031). Median survival time was not reached. Median disease-free survival was 82 months (CI 50 % 28–275). In univariate analysis, age younger than 36 years was an unfavorable prognostic factor (p = 0.003). Patients with metastases at diagnosis had poorer survival (p = 0.048). Late side effects related to radiotherapy were dementia, leukoencephalopathy or memory loss in seven cases, occipital ischemia in one, and grade 3 seizures in two cases. Side effects related to chemotherapy were grade 3–4 leucopenia in five cases, grade 4 thrombocytopenia in three cases, grade 2 anemia in two cases, grade 4 pancytopenia in one case, grade 4 vomiting in one case and renal failure in one case.
Conclusions
Age and dissemination at diagnosis influenced survival in our series. The prevalence of chronic toxicity suggests that new adjuvant strategies are advisable.
Similar content being viewed by others
Introduction
Pineal regional tumors account for <1 % of primary brain tumors, and primary tumors of the pineal gland (PPTs) represent <30 % of all pineal neoplasms [1, 2]. They are more frequent in the middle-eastern populations in the USA [3].
PPTs are a heterogeneous group of mass lesions originating in or adjacent to the pineal gland located on the diencephalic roof at the posterior extremity of the third ventricle [4] and represent a spectrum of neoplasms ranging from benign to malignant. Approximately, three-fourth of the tumors of the pineal region is malignant with a propensity of seeding in cerebral space fluid (CSF). PPTs have their origin in the pineocyte, a cell with photosensory and neuroendocrine functions. PPTs are classified as pineocytoma (PC) (WHO grade II), pineocytoma with intermediate differentiation (PID) (provisional WHO grade II–III) and pineoblastoma (PNB) (WHO grade IV) [2]. A fourth entity has been described recently: the so-called papillary tumor of the pineal region which has a higher risk of local recurrence [5]. PNB can arise at any age, but occurs most often in children. PC is most frequently encountered in adults [4, 6] Clinically, it is not possible to differentiate PC from other pineal region lesions. The clinical signs and symptoms relate to increased intracranial pressure, neuro-ophthalmologic dysfunction (particularly Parinaud’s syndrome), changes in mental status, dysfunction of the brain stem and cerebellum and, sometimes, hypothalamic-based endocrine abnormalities [5].
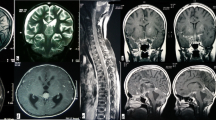
Because of the rarity of these tumors, the study of their biological characteristics and clinical outcome is difficult. The outcome may depend on several factors including histological subtype, staging at diagnosis and type of surgery, type and dose of radiotherapy, and administration of chemotherapy. For all pineal tumors, histologic subtype had the greatest impact on outcome [7]. The Rare Cancer Network (RCN) (http//www.rarecancer.net) has the aim to collect, analyze and publish data on either rare types of cancers or rare presentations of common cancers. We present a multicentric retrospective study on PPTs. The purpose of this report is to better define outcome and possible prognostic factors in the era of modern imagery (magnetic resonance imaging), surgery and adjuvant treatment of PPTs.
Patients and methods
This is a multicentric retrospective study of the RCN. All consecutive patients affected with PPTs from seven academic centers were analyzed following local ethics board approval. A questionnaire for recording clinical, treatment and outcome data was sent to participating centers. There were 35 patients with PPTs diagnosed between 1988 and 2006. All diagnoses were histopathologically confirmed and treated in the era of magnetic resonance imaging. The patients’ workups are displayed in Table 1.
Overall survival and disease-free survival rates were calculated from the date of histological diagnosis by the Kaplan–Meier method [8]. The log-rank test was used to compare different survival functions according to clinical (age, gender, duration of symptoms, metastatic disease at diagnosis) and therapeutic factors (type of resection, radiotherapy, chemotherapy). A Cox model was used for continuous variables. Multivariate analysis was performed by Cox stepwise regression analysis to define the independent contribution of each factor [9]. All p values were derived from log-rank tests: a p value of ≤0.05 was considered to indicate statistical significance.
Results
There were 23 females and 12 males (F/M ratio 2:1). The median age was 36 years (range 2–76 years). Duration of symptoms ranged from 2 days to 5 years (median of 60 days) (Table 2). Two patients were corticosteroid dependant during all adjuvant treatment and at follow-up. At diagnosis, six patients with PNB had evidence of central nervous system seeding. In one patient, MRI showed synchronous brain metastases and leptomeningeal seeding. MRI of the spine was positive for metastatic disease in four patients with PNB. In addition, malignant cells in CSF were found in three patients with PNB, and one of them had evidence of leptomeningeal implants. Histological subtypes were PNB in 21 patients, PC in 8 patients and PID in 6 patients. One patient with definitive PNB at relapse was initially diagnosed with a pure germinoma. In 15 cases, immuno-histochemical analysis was available (10 PNB, 2 PC, 3 PID). All samples showed positivity for synaptophysin, five (3 PNB, 1 PC, and 1 PID) for neuron-specific enolase and three for glial fibrilary acidic protein (GFAP), cd5leu7 and Ulex europaeus lectin, respectively. In 11 cases, the tissue was reviewed by a neuropathologist (SB).
The type of surgical resection is displayed in Table 1. In a case without upfront surgery, pathology diagnosis was established at tumor relapse. In 15 cases, postoperative imaging was available within the first 72 h (in 20 patients within the first 29 days). All patients underwent RT. In nine cases, RT doses to the tumor bed were lower than 54 Gy (median 54 Gy, range 7–59.4). One patient (PNB) only received 7 Gy because of early progression. In 13 patients, RT was only focal to the primary tumor site; 10 of them had PC (6) or PID (4) histology. Only a patient received tetra-ventricular RT (VRT) (PNB case), without whole brain irradiation (WBI) (50 Gy in 25 fractions). WBI was delivered to 16 patients (range 25–45 Gy), 13 with PNB and 3 with PID. Craniospinal irradiation (CSI) was delivered to 13 patients (all with PNB) (range 25–43 Gy). The median daily dose was 1.8 Gy (range 1.5–2.0 Gy) for all volumes treated. Five patients received fractionated radiotherapy with stereotactic conditions.
Chemotherapy was administered in 12 patients (platinum-based in 8 patients) and was prescribed to PNB patients (11 cases) and for 1 case of PID.
For all patients, the median follow-up was 44 months (range 2.4–275), and for alive patients 68.2 moths (range 7–275). Two patients with disease (one PC and one PNB) were lost of follow-up at 7 months and 23 years, respectively. Fifteen patients relapsed (14 PNB and 1 PC) with a median time of 18 moths (range 1–82). Sites of relapse were inside RT volumes in 16 locations, outside in 6 locations and both in 3 locations. Three of them received <54 Gy on GTV, but total dose did not result as a significant prognostic factor for tumor relapse. Significantly, patients with PNB were more prone to relapse (p = 0.031). At the time of analysis, 13 patients were alive without evidence of disease, 9 patients were alive with stable disease, 11 patients died because of tumor progression and 2 patients died without evidence of disease. Median survival time for patients who died from disease was 25 months (range 2–138). The overall median survival time was not reached. The median of disease-free survival was 82 months (CI 50 %, 28–275).
In univariate analysis, age younger than 36 years was an unfavorable prognostic factor (log rank = 8.49, p = 0.003) (Fig. 1). Furthermore, patients with metastases at diagnosis had poorer survival (log rank = 3.88, p = 0.048) (Fig. 2). A trend for poorer survival was seen in patients with PNB. In multivariate analyses, no variable resulted as independent prognostic factor.
The most severe late effects possibly related to radiotherapy were dementia, leukoencephalopathy and memory loss in seven cases, grade 3 seizures in two cases, occipital ischemia in one case, long-term leucopenia in one case and grade 4 thrombocytopenia in one case (this case was only treated with RT). No relation with RT volumes could be established with toxicity. More serious late effects probably related to chemotherapy were grade 3 neutropenia in four cases, grade 4 pancytopenia in one case, grade 4 vomiting in one case and renal failure in one case.
Discussion
PPTs are rare in the context of clinical oncology. Modern series using MRI, immunohistochemistry, more advanced surgical techniques and more precise radiotherapy are more illustrative to demonstrate the real current outcome of these tumors [1, 10–16]. However, the rarity of PPTs makes the possibility of conducting prospective clinical trials a very difficult task. Our RCN series is subject to the same limitations of any retrospective study. However, we intended this study for increasing knowledge of these patients in the modern era.
The gender ratio of 2:1 in our study is in favor of female patients which confirm data initially reported by Fauchon et al. [1].
On the other hand, age seems to be significantly linked to the degree of malignancy and is related to the different histologies [1, 4].
Completeness of staging is crucial to define prognosis for these patients. In the CCG trial, four children with PNB had disseminated disease at diagnosis and developed progression of disease with a median of 4 months, in contrast to higher significant overall survival in patients with localized disease [17]. Currently, initial staging should include MRI of the spinal cord [1] and CSF cytology [18]. Both procedures were performed in 33 cases of our series. This figure is higher than those of previous series [1]. Meningeal spread was observed in six patients (17 %), all with PNB. In previous pediatric series, 16–45 % of patients presented with spinal spread [18–21].
Different surgical approaches [15, 22] and aggressiveness of surgery did not improve survival significantly in our study, as reported by others [1]. Consequently, residual disease after surgery does not adversely affect outcome, although its presence can be used to monitor response to treatment [12]. Of our 35 patients, 20 (57 %) in contrast to 77 % in the French series [1] had postoperative neuroimaging, but information regarding the extent of residual disease was incomplete.
The knowledge of histological subtypes should allow us to determine the guidelines for adjuvant therapy because of the varying level of aggressiveness of such lesions, but the literature is scarce regarding this.
No prospective series have addressed the issues of different RT techniques and dose levels for PPTs treatment. In the 1990s [23], most patients receiving <50 Gy to the primary tumor (86 %) developed a local failure. In contrast, no patient receiving 50 Gy or more developed local relapse. Local failure occurred in one of four and four of nine in PC and PNB patients, respectively. Of the patients with potentially seeding tumors who received local-field or only WBI, four of eight had leptomeningeal failures, as opposed to patients who received CSI (14 %). The same group later defined volumes and doses of radiotherapy [21]. Patients with no risk of spinal metastases can be given WBI, because the spinal seeding appears to be no greater than after CSI. The primary tumor should receive 50.4–54 Gy, and spinal metastases should receive 45 Gy, in 1.8 Gy fractions. Prophylactic radiotherapy should deliver 30–45 Gy to uninvolved high-risk areas. Patients with PC can be irradiated to the local tumor alone. Furthermore, the CCG-921 trial report is the only one which suggests that CSI has a significant impact on survival, with a 3-year event-free survival of 61 % [17]. The authors stressed, however, the early delayed toxicity of the CSI. Changes of fractionation did not improve results [24]. In general, our radiation approach was similar to the reported series using higher doses than 50 Gy to the tumoral bed and CSI for patients with histologies of high-risk dissemination. Conventional techniques were the rule. However, five patients received radiotherapy with stereotactic conditions that could reduce late toxicity. Leptomeningeal seeding was observed in PNB cases, like other series [11, 13].
The role of chemotherapy is still very controversial. It seems to be indicated in high-risk patients. All but one patient of our series who received chemotherapy had PNB. Although some series reported promising results in few cases [23, 25], this perspective was not confirmed by prospective clinical trials. In the Pediatric Oncology Group (POG) trial [20], postoperative chemotherapy delaying CSI ultimately failed for all children. A similar lack of efficacy of chemotherapy was seen in the CCG trial [17] for children younger than 18 months. The delay of radiotherapy seemed to yield worse results than the combination of radiotherapy and chemotherapy, as demonstrated by Hinkes et al. [26]. Their results showed that the five older patients who received chemotherapy and CSI were still alive (median overall and progression-free survival of 7.9 years). In contrast, all five children younger than 3 years, who deferred CSI, died of tumor progression (median overall survival of 0.9). In our series, no patient was scheduled to receive delayed radiotherapy. On the other hand, adding chemotherapy to radiotherapy was not more advantageous in the PNETs SIOP trial [27]. Specifically, however, for pineal region tumors, a better overall survival was observed compared to other locations. In a more recent series of 13 PNB patients [28], adequate surgery combined with CSI and chemotherapy appeared to be correlated with improved survival and event-free survival (p = 0.05 and p = 0.03, respectively). Event-free survival and overall survival rates for pineal tumors were 92.9 and 71.4 % at 3 and 5 years, respectively, but for non-pineal primary they were both 40.7 %, at 3 and 5 years.
Anecdotal reports have been observed in the literature concerning late side effects. In the series of Schild et al. [23], two patients were noted to have an impaired memory after only focal irradiation. In the French series [1], one case of radiation necrosis and one case of encephalitis were observed. In the CCG-921 trial [17], all patients had significant neurocognitive deficits, and two of them were considered as profoundly neurologically devastated. We consider that side effects in our series can also be related to other treatment options (surgery, radiotherapy and chemotherapy) and the sequelae of the tumor itself. However, side effects likely related to radiotherapy (dementia, leukoencephalopathy, memory loss, occipital ischemia, seizures) reported in our study are not negligible. Late side effects due to chemotherapy (severe pancytopenia, renal failure) are also noteworthy.
The site of relapse is closely related to the tumor grade [1]. Spinal deposits are common with PNB [17, 20, 21]. In the POG experience [20], all 11 reported children ultimately failed after chemotherapy, and all but one who had complete metastatic assessment presented with distant seeding at progression. In the French series [1], combining adult and pediatric PNB patients, spinal relapses were more frequent than previously reported [7]. In contrast, in our experience, in only one patient PC recurred, as in the French series [1]. This is an indication for primary surgical approach alone [1, 23]. Our series points out that the risk of local recurrence in PID patients and CSF metastases occurs in a minority, in contrast to others [29, 30]. In our series 15 patients relapsed (14 PNB cases, 1PC case). All these relapses occurred inside the radiotherapy fields. Significantly, patients with PNB were more relapse prone.
Given the paucity of series, survival data on PPT patients are scarce. Table 3 shows the main series reported in the literature and their patients’ outcome. In our series, the results are comparable. The median follow-up of patients alive was almost 6 years, probably not enough to define very late relapses.
In conclusion, the combined treatments for PPTs in this series achieved good overall survival. Age, dissemination at diagnosis and, probably, histological subtypes influenced survival in our series. The prevalence of chronic toxicity suggests that new strategies in radiotherapy and chemotherapy are advisable. Further studies are needed to really define different diseases of PPTs concerning histological subtypes and individualized therapeutic strategies.
References
Fauchon F, Jouvet A, Paquis P et al (2000) Parenchymal pineal tumors: a clinicopathological study of 76 cases. Int J Radiat Oncol Biol Phys 46:959–968
Nakazato Y, Jouvet A, Scheithauer BW (2007) Tumours of the pineal region. In: Louis DN, Ohgaki H, Wiestler OD, Cavenee WK (eds) WHO classification of tumours of the central nervous system, 4th edn. International Agency for Research on Cancer, Lyon, pp 121–129
Nasseri K, Mills JR (2009) Epidemiology of primary brain tumors in the Middle Eastern population in California, USA 2001–2005. Cancer Detect Prev 32:363–371
Tsumanuma I, Tanaka R, Washiyama K (1999) Clinicopathological study of pineal parenchymal tumors: correlation between histopathological features, proliferative potential, and prognosis. Brain Tumor Pathol 16:61–68
Jouvet A, Fauchon F, Liberski P et al (2003) Papillary tumor of the pineal region. Am J Surg Pathol 27:505–512
Shibui S, Nomura K (2009) Statistical analysis of pineal tumors based on the data of Brain Tumor Registry of Japan. Prog Neurol Surg 23:1–11. doi:10.1159/000210049
Fuller BG, Kapp DS, Cox R (1994) Radiation therapy of pineal region tumors: 25 new cases and a review of 208 previously reported cases. Int J Radiat Oncol Biol Phys 28:229–245
Kaplan EL, Meier P (1958) Nonparametric estimation from incomplete observations. J Am Stat Assoc 53:457–481
Cox DR (1972) Regression models and life-tables. J R Stat Soc Ser B (Methodol) 34:187–220
Timmermann B, Kortmann RD, Kuhl J et al (2002) Role of radiotherapy in the treatment of supratentorial primitive neuroectodermal tumors in childhood: results of the prospective German brain tumor trials HIT 88/89 and 91. J Clin Oncol 20:842–849
Hasegawa T, Kondziolka D, Hadjipanayis CG et al (2002) The role of radiosurgery for the treatment of pineal parenchymal tumors. Neurosurgery 51:880–889
Lutterbach J, Fauchon F, Schild SE et al (2002) Malignant pineal parenchymal tumors in adult patients: patterns of care and prognostic factors. Neurosurgery 51:44–55 (discussion 55–56)
Reyns N, Hayashi M, Chinot O et al (2006) The role of Gamma Knife radiosurgery in the treatment of pineal parenchymal tumours. Acta Neurochir (Wien) 148:5–11 (discussion 11). doi:10.1007/s00701-005-0626-z
Timmermann B, Kortmann RD, Kuhl J et al (2006) Role of radiotherapy in supratentorial primitive neuroectodermal tumor in young children: results of the German HIT-SKK87 and HIT-SKK92 trials. J Clin Oncol 24:1554–1560. doi:10.1200/JCO.2005.04.8074
Hernesniemi J, Romani R, Albayrak BS et al (2008) Microsurgical management of pineal region lesions: personal experience with 119 patients. Surg Neurol 70:576–583. doi:10.1016/j.surneu.2008.07.019
Stoiber EM, Schaible B, Herfarth K et al (2010) Long term outcome of adolescent and adult patients with pineal parenchymal tumors treated with fractionated radiotherapy between 1982 and 2003—a single institution’s experience. Radiat Oncol 5:122. doi:10.1186/1748-717X-5-122
Jakacki RI, Zeltzer PM, Boyett JM et al (1995) Survival and prognostic factors following radiation and/or chemotherapy for primitive neuroectodermal tumors of the pineal region in infants and children: a report of the Childrens Cancer Group. J Clin Oncol 13:1377–1383
Chang SM, Lillis-Hearne PK, Larson DA et al (1995) Pineoblastoma in adults. Neurosurgery 37:383–390 (discussion 390–391)
Donat JF, Okazaki H, Gomez MR et al (1978) Pineal tumors. A 53-year experience. Arch Neurol 35:736–740
Duffner PK, Cohen ME, Sanford RA et al (1995) Lack of efficacy of postoperative chemotherapy and delayed radiation in very young children with pineoblastoma. Pediatric Oncology Group. Med Pediatr Oncol 25:38–44
Schild SE, Scheithauer BW, Haddock MG et al (1996) Histologically confirmed pineal tumors and other germ cell tumors of the brain. Cancer 78:2564–2571
Tsumanuma I, Tanaka R, Fujii Y (2009) Occipital transtentorial approach and combined treatments for pineal parenchymal tumors. Prog Neurol Surg 23:26–43. doi:10.1159/000210051
Schild SE, Scheithauer BW, Schomberg PJ et al (1993) Pineal parenchymal tumors. Clinical, pathologic, and therapeutic aspects. Cancer 72:870–880
Prados MD, Edwards MS, Chang SM et al (1999) Hyperfractionated craniospinal radiation therapy for primitive neuroectodermal tumors: results of a Phase II study. Int J Radiat Oncol Biol Phys 43:279–285
Ghim TT, Davis P, Seo JJ et al (1993) Response to neoadjuvant chemotherapy in children with pineoblastoma. Cancer 72:1795–1800
Hinkes BG, von Hoff K, Deinlein F et al (2007) Childhood pineoblastoma: experiences from the prospective multicenter trials HIT-SKK87, HIT-SKK92 and HIT91. J Neurooncol 81:217–223. doi:10.1007/s11060-006-9221-2
Pizer BL, Weston CL, Robinson KJ et al (2006) Analysis of patients with supratentorial primitive neuro-ectodermal tumours entered into the SIOP/UKCCSG PNET 3 study. Eur J Cancer 42:1120–1128. doi:10.1016/j.ejca.2006.01.039
Gilheeney SW, Saad A, Chi S et al (2008) Outcome of pediatric pineoblastoma after surgery, radiation and chemotherapy. J Neurooncol 89:89–95. doi:10.1007/s11060-008-9589-2
Pusztaszeri M, Pica A, Janzer R (2006) Pineal parenchymal tumors of intermediate differentiation in adults: case report and literature review. Neuropathology 26:153–157
Kim BS, Kim DK, Park SH (2009) Pineal parenchymal tumor of intermediate differentiation showing malignant progression at relapse. Neuropathology 29:602–608. doi:10.1111/j.1440-1789.2008.00994.x
Acknowledgments
We thank Mrs. Marta Jordan for her administrative support of the article.
Conflict of interest
The authors declare that they have no conflict of interest relating to the publication of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Villà, S., Miller, R.C., Krengli, M. et al. Primary pineal tumors: outcome and prognostic factors—a study from the Rare Cancer Network (RCN). Clin Transl Oncol 14, 827–834 (2012). https://doi.org/10.1007/s12094-012-0869-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-012-0869-0