Abstract
Background
Triple therapy for the treatment of hepatitis C virus (HCV) with first-generation directly acting antiviral agents, the non-structural serine protease inhibitors boceprevir (BOC) and telaprevir have resulted in improved sustained virologic response (SVR) rates. However, a high incidence of adverse events (AEs), high pill burdens and drug interactions remain significant barriers to successful completion of therapy. The aim of this study was to evaluate the AEs observed with BOC triple therapy in comparison to IFN-free sofosbuvir/ribavirin (SOF/RBV) therapy in HCV monoinfected, genotype-1 (GT-1) individuals.
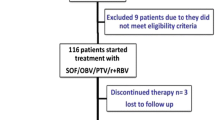
Methods
We retrospectively evaluated HCV monoinfected, treatment-naïve or -experienced, GT-1 individuals treated with either BOC/IFN/RBV at the Veterans Affairs Medical Center, Baltimore (n = 97) or SOF/RBV in the NIAID SPARE clinical trial (n = 60). AEs, namely hematologic (hemoglobin, neutrophil and platelet counts), hepatic (alanine transaminase or bilirubin) and renal (eGFR), were measured according to the DAIDS toxicity table (version 1.0).
Results
BOC/IFN/RBV was associated with significantly more AEs, most commonly neutropenia, anemia and thrombocytopenia. In the SOF/RBV cohort, five (8 %) patients discontinued treatment early, but none (0 %) were because of AEs, while 60 (62 %) patients on triple therapy discontinued treatment early, 34 (57 %) because of AEs. SVR24 rates were 68 versus 34 % with SOF/RBV versus BOC/IFN/RBV.
Conclusions
SOF/RBV treatment was associated with fewer side effects than BOC-based triple therapy, appearing to be a safer and more tolerable alternative for HCV GT-1 subjects. These results show that emerging IFN-free therapies may enhance patient adherence, allowing treatment of larger number of patients with improved efficacy.


Similar content being viewed by others
References
Alter HJ, Seeff LB. Recovery, persistence, and sequelae in hepatitis C virus infection: a perspective on long-term outcome. Semin Liver Dis 2000;20(1):17–35.
Kim WR. The burden of hepatitis C in the United States. Hepatology 2002;36(5 Suppl 1):S30–S34.
Ly KN, et al. The increasing burden of mortality from viral hepatitis in the United States between 1999 and 2007. Ann Intern Med 2012;156(4):271–278.
Mohd Hanafiah K, et al. Global epidemiology of hepatitis C virus infection: new estimates of age-specific antibody to HCV seroprevalence. Hepatology 2013;57(4):1333–1342.
Butt AA, Wang X, Moore CG. Effect of hepatitis C virus and its treatment on survival. Hepatology 2009;50(2):387–392.
Bacon BR, et al. Boceprevir for previously treated chronic HCV genotype 1 infection. N Engl J Med 2011;364(13):1207–1217.
Hezode C, et al. Telaprevir and peginterferon with or without ribavirin for chronic HCV infection. N Engl J Med 2009;360(18):1839–1850.
McHutchison JG, et al. Telaprevir with peginterferon and ribavirin for chronic HCV genotype 1 infection. N Engl J Med 2009;360(18):1827–1838.
Kwo PY, et al. Efficacy of boceprevir, an NS3 protease inhibitor, in combination with peginterferon alfa-2b and ribavirin in treatment-naive patients with genotype 1 hepatitis C infection (SPRINT-1): an open-label, randomised, multicentre phase 2 trial. Lancet 2010;376(9742):705–716.
Poordad F, et al. Boceprevir for untreated chronic HCV genotype 1 infection. N Engl J Med 2011;364(13):1195–1206.
Sherman KE, et al. Response-guided telaprevir combination treatment for hepatitis C virus infection. N Engl J Med 2011;365(11):1014–1024.
Fried MW, et al. Once-daily simeprevir (TMC435) with pegylated interferon and ribavirin in treatment-naive genotype 1 hepatitis C: The randomized PILLAR study. Hepatology. 2013;58(6):1918–1929.
Gane EJ, et al. Nucleotide polymerase inhibitor sofosbuvir plus ribavirin for hepatitis C. N Engl J Med 2013;368(1):34–44.
Osinusi A, et al. Sofosbuvir and ribavirin for hepatitis C genotype 1 in patients with unfavorable treatment characteristics: a randomized clinical trial. JAMA 2013;310(8):804–811.
Gane EJ, Stedman CA, Hyland RH, et al. Once daily sofosbuvir (GS-7977) plus ribavirin in patients with HCV genotypes 1, 2, and 3: the ELECTRON trial. Hepatology. 2012;56(suppl):306A–307A.
Lawitz E, Gane EJ. Sofosbuvir for previously untreated chronic hepatitis C infection. N Engl J Med 2013;369(7):678–679.
Sovaldi, Sovaldi (sofosbuvir) tablets: US prescribing information. http://www.sovaldi.com/, Dec 2013.
Division of AIDS table for grading the severity of adult and pediatric adverse events, December 2004. (http://www.niaid.nih.gov/LabsAndResources/resources/DAIDSClinRsrch/Documents/daidsaegradingtable.pdf).
Jacobson IM, Kowdley KV, Kwo PY. Anemia management in the era of triple combination therapy for chronic HCV. Gastroenterol Hepatol (N Y) 2012;8(9 Suppl 6):1–16.
Maasoumy B, et al. Eligibility and safety of triple therapy for hepatitis C: lessons learned from the first experience in a real world setting. PLoS One 2013;8(2):e55285.
Majid A, et al. Predictors of early treatment discontinuation in a cohort of patients treated with boceprevir-based therapy for hepatitis C infection. J Viral Hepat. 2014;21(8):585–589.
Lawitz E, et al. Sofosbuvir for previously untreated chronic hepatitis C infection. N Engl J Med 2013;368(20):1878–1887.
Naggie S, Sulkowski M, Lalezari J, et al. Sofosbuvir plus ribavirin for HCV genotype 1–3 infection in HIV coinfected patients (PHOTON-1). (Abstract 26) Presented at Conference on Retroviruses and Opportunistic Infections; 2014 March 4. Boston; 2014.
Schmidt-Martin D, Houlihan D, McCormick A. From the CUPIC study: great times are not coming(?). J Hepatol 2014;60(4):899–900.
Acknowledgements
We would like to acknowledge the contributions of the following individuals: Laura Heytens, who was the study coordinator on the SPARE study. This research was supported in part by the intramural program of the National Institute of Allergy and Infectious Diseases. The data from this study have been partially presented at The Conference for Retroviruses and Opportunistic Infections (CROI) 2014 in Boston, MA, USA.
Compliance with ethical requirements and Conflict of interest
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. Informed consent was obtained from all patients for being included in the study. Rohit Talwani has served as a speaker for Merck and performs research funded by Vertex Pharmaceuticals. Shivakumar Narayanan, Kerry Townsend, Thomas Macharia, Adrian Majid, Amy Nelson, Robert Redfield, Shyam Kottilil, Rohit Talwani and Anu Osinusi have no conflicts of interest to report.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclaimer: The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products or organizations imply endorsement by the US Government.
Shivakumar Narayanan and Kerry Townsend contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Narayanan, S., Townsend, K., Macharia, T. et al. Favorable adverse event profile of sofosbuvir/ribavirin compared to boceprevir/interferon/ribavirin for treatment of hepatitis C. Hepatol Int 8, 560–566 (2014). https://doi.org/10.1007/s12072-014-9574-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-014-9574-0