Abstract
To find out the utility of the scalp flap based on the posterior branch of the superficial temporal artery in patients with head and neck mucormycosis and malignancy. This was a multi-institutional observational study conducted at a tertiary cancer centre in North East India and a super-speciality hospital in Maharashtra from January 2021 to June 2021. Patients with malignancy and mucormycosis were only considered. In our study, we have seven patients (n = 7), two of them had mucormycosis and 5 had squamous cell carcinoma of the head and neck region. Out of the 5 cases of the head and neck malignancy, two cases were recurrent ones, another two cases where primary flap failed and in the last case, the patient was unfit for free tissue transfer due to cardiac issues. The mean age in the series was 50.42 years and the average duration of raising the flap was 22.86 min. Average hospital stays for head and neck cancer patients are 4.6 days and for mucormycosis patients, it is 22.5 days. No flap related complications were noted during the series. Scalp flap based on the posterior branch of the superficial temporal artery is a useful option in recurrent malignancy cases, in primary cases as a salvage option and in patients where long duration surgery is not possible due to poor general condition like in critical mucormycosis. Post-operative hair growth at the flap site and alopecia at the donor scalp are concerns and therefore, careful patient selection is a must.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The scalp island flap based on the posterior branch of the superficial temporal artery is a very useful flap for facial reconstruction though there is not much description of this flap in the literature. The superficial temporal artery and vein have a constant anatomical course [1]. This vessel system is used as a vascular pedicle for the vast array of flaps including the temporoparietal fascial flap and cutaneous flaps like the total forehead flap and temporal skin island flap. At the level of the superior auriculo-cephalic groove, the superficial temporal artery divides into anterior and the posterior branches, the posterior branch courses upward into the scalp for a distance of approximately 12 cm within the temporoparietal fascia and near the vertex of the head, it joins the subdermal vascular plexus. With handheld doppler, it can be easily traced, but it can also be palpated manually.
Mucorales group of the opportunistic fungi causes mucormycosis (black fungus) [2, 3]. The predisposing factors are uncontrolled diabetes, long term steroid use, immunosuppressive therapy, malignancies, malnutrition and other conditions associated with the decreased immune response of the body [3]. Extensive use of the industrial oxygen for treatment of the COVID-19 patients is also attributed as the aetiology for the rising number of black fungus cases in covid patients [4]. Six categories of mucormycosis are being described, rhino cerebral, pulmonary, cutaneous, gastro-enteric, disseminated and miscellaneous. Covid related mucormycosis are mostly rhinomaxillary (a variety of rhino cerebral type), which involves the nose and maxilla and at the same time may spread to the orbit and brain. The mainstays of treatment of such infection are -eliminating the predisposing factors (control of hyperglycemia and ketoacidosis or boost up the immunity of the patients etc.), total radical debridement of all dead tissue and use of amphotericin B, if contraindicated then posaconazole [5, 6]. Early diagnosis and good general health are two important predictors for the outcome. Despite all positive factors, rhinomaxillary mucormycosis may result in excessive bone and soft tissue destruction leading to a compromised facial aesthetic and quality of life. The scalp island flap based on the posterior branch of the superficial temporal artery can be used easily for this group of patients due to the proximity of the flap to the area. The flap is very easy to harvest and it took only a few minutes to raise, make it a good option for patients with the poor general condition, where operative duration is crucial. This flap can also be used in head and neck malignancy as a salvage option or in recurrent cases where options are limited. In the past, it was used for the palate, buccal mucosa, cheek and upper lip reconstruction [7, 8]. This flap results in an alopecic patch at the scalp and is not suitable for younger patients.
Materials and Methods
This was a multi-institutional observational study conducted at a tertiary cancer centre in North East India and a super-speciality hospital in Maharashtra from January 2021 to June 2021. Patients with malignancy and mucormycosis were only considered. All the reconstructions are done with scalp island flaps based on the posterior branch of the superficial temporal artery. The postoperative outcome is assessed and data were collected from patient records and hospital online reporting system.
The planning of the surgery was performed according to the location of the defect. The length of hospitalization and the presence of local and systemic postoperative complications were assessed. A total of six(n = 7) patients were operated on, out of which four patients (n = 5) were male and two (n = 2) were female. All the patients are followed up minimum for two months.
Results and Observations
-
1.
Age Distribution:
The average mean age of the series is 50.42 years. The youngest patient is 40 years old and the oldest one is 65 years old.
-
2.
Type of Disease:
71% of patients(n = 5) with reconstruction with scalp island flap based on the posterior branch of the superficial temporal artery had head and neck malignancy and 28% (n = 2) had rhinomaxillary mucormycosis.
-
3.
Location of the Tumour/Mucormycosis:
Both the cases of mucormycosis were rhinomaxillary type (one on the right side and the other on the left side) needing removal of the maxilla and the orbital content. Out of the five patients with head and neck malignancy, four were seen at the buccal mucosa and the fifth one at the hard palate, all of them were squamous cell carcinomas. The two patients with buccal mucosa malignancies were recurrent ones and the other two were new (primary flap loss occurred in both the new patients), scalp island flap was done as a salvage option.
-
4.
Procedures Performed
-
a)
Mucormycosis
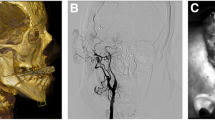
Case 1, a 42 years old male with a history of recent COVID-19 infection, known diabetic and use of steroids during treatment course developed redness around the left periorbital region and blood-tinged discharge from the left nostril. Radical debridement was done (maxillectomy and orbital exenteration) and the resulting defect was reconstructed with scalp island flap based on the posterior branch of the superficial temporal artery (Fig. 1).
Case 2, has a similar history to case 1, with involvement of the left-sided orbit and maxilla. This patient also had uncontrolled diabetes and received steroids during the previous hospital stay for the COVID-19 treatment.
-
b)
Head and Neck Malignancy
Case 1, a 59 years old lady presenting with a left buccal mucosal SCC underwent wide local excision + segmental mandibulectomy and modified radical neck dissection and the defect reconstructed with pectoralis major myocutaneous flap (PMMC). Postoperatively, the patient developed a large oro-cutaneous fistula due to flap necrosis. The large defect was reconstructed with a scalp island flap (Fig. 2).
Case 2, a 55 years old male presenting with a left buccal mucosal growth involving the retromolar trigone (RMT), underwent wide local excision of the tumour, segmental mandibulectomy, and left side neck dissection and reconstruction with the PMMC and deltopectoral (DP) flap. In the postoperative period, there was partial necrosis of the PMMC and DP flap, needing scalp flap for the final reconstruction (Fig. 3).
Case 3, a 40 years old male with a history of the right squamous cell carcinoma (SCC), underwent right hemi-glossectomy, segmental mandibulectomy and neck dissection and reconstruction with the PMMC flap in 2019. The patient developed recurrence again at the right buccal mucosa in 2021 for which he underwent wide local excision and scalp flap (Fig. 4).
Case 4, a 65 years old male developed squamous cell carcinoma of the right hard palate needing partial maxillectomy and reconstruction with scalp island flap. The free tissue transfer was avoided in this case due to cardiac issues (Fig. 5).
Case 5, a 45 years old male presenting with a recurrent left-sided buccal mucosal growth, where other reconstruction options are utilised in the previous surgery, this time, scalp flap was used (Fig. 6).
-
c)
Flap Harvesting Technique
Firstly, the posterior branch of the superficial temporal artery is identified with handheld doppler or palpated and mapped from its origin from the main trunk to the proximal margin of the designed flap. We don't do the pedicle dissection in the subdermal plan like most works of literature suggest, the dissection in the subdermal plane is a tedious job and it takes lots of time. As a simplified version, we take a strip of 2 cm skin paddle along with the pedicle (1 cm on each side of the vessels) that saves lots of time and later we close the defect primarily. The islanded scalp flap is raised in a loose areolar tissue plan and the same plane is followed till the adequate flap and pedicle length is achieved. During the dissection, the anterior branch of the superficial temporal artery is encountered midway and it is suture ligated. The pedicle dissection can be extended to the tragus to gain extra length of the pedicle. Lastly, the flap is transferred to the intraoral defect (via subcutaneous tunnel) or the external defect according to the need and a split-thickness skin graft is applied at the donor site.
-
5.
Duration of the Surgery
The average duration of raising the flap was 22.86 min.
-
6.
Complications
No flap related complications are noted during the series. One of the concerns of the flap is post-surgery hair growth. For intra-oral defects, hair inside the oral cavity can be managed with laser hair removal, but two of our patients opted for the frequent careful self-trimming, they didn’t complain of any discomfort. Donor site alopecia is also a concern of this flap.
-
7.
Hospital Stays
Average hospital stays for head and neck cancer patients are 4.6 days and for mucormycosis patients, it is 22.5 days. Patients with mucormycosis have more hospital stays as compared to the malignancy cases as they require serial debridement and both the patients were admitted at critical condition.
Discussion
Reconstructive Options for the Head and Neck Mucormycosis
A tissue diagnosis of mucormycosis is a must before starting treatment. Histopathological staining or direct smear with potassium hydroxide showing characteristic fungal hyphae is confirmatory of mucormycosis infection. A fungal culture is accurate in 30–50% of cases only while the accuracy of the molecular diagnosis by the PCR is 98%. The management of mucormycosis is categorised into four parts,
-
1)
rapid control of the underlying cause,
-
2)
early start of the lysosomal amphotericin B,
-
3)
early surgical debridement and
-
4)
appropriate reconstruction according to the defect and aggressive rehabilitation.
As surgical defects are extensive, reconstruction can be either prosthetic and autologous. Prosthetic reconstructions are easier, gives good cosmesis and it is ideal for older age patients and patients with the poor general condition. Other benefits are the possibility of dental rehabilitation and easy diagnosis of recurrent infection. The drawbacks of this procedure are static implants, cumbersome use at times, hygienic issues, inability to use when critical structures are exposed. There are additional hardware related issues, loss of adhesives, magnet related problems with these conventional prostheses. Osseo-integrated implants are also used nowadays in selected patients. Autologous reconstructions with the free tissue transfer and locoregional flaps are frequently performed in extensive facial defects. The frequently performed free tissue transfers are free fibular osteocutaneous flap, free anterolateral thigh flap, free radial forearm flap. The functional outcome of these free tissue transfers is excellent, but at times the cosmetic outcome may not be that good. Local flaps used in these reconstructions are PMMC flap in case of short neck and longer pedicle patients, total forehead flap, scalp island flaps based on the posterior branch of the superficial temporal artery. The expertise of the free tissue transfer is not always present in all the centres and these locoregional flaps are saviour there. These autologous reconstructions bring vascularized tissue to the native bed and fasten the healing, increases the resistance of the native tissue to the radiation-induced damage [9].
In our study, two patients presented with mucormycosis involving the rhinomaxillary region. Both the patients underwent thorough debridement, following which reconstruction was done using the scalp flap based on posterior branch of the superficial temporal artery. These defects weren’t isolated to the orbit but also involved the skin as well as the anterolateral surface of the maxilla. The ideal reconstructive option would have been a free flap, but the general condition of the patient warranted it. Hence, the scalp flap was chosen as an alternative. Often, a flap may be relatively bulky and fill or overfill the composite orbital defect. In such instances of extensive defects, an additional surgery may be required for debulking of the flap as well as to create an orbital rim. The debulking of the flap gives space for the orbital prosthesis while the rim serves as an inferior support and gives projection to the prosthesis. A large remaining socket, by contrast, can be filled postoperatively with a hollow prosthesis that is still light, easy to wear, and cosmetically pleasing. All these options need to be carefully explained to the patient prior to surgery. As far as this particular two patients are concerned, they have an option to undergo a revision surgery for a better aesthetic orbital prosthesis. If the patient decides against undergoing a second surgery, then a spectacle mounted or adhesive orbital prosthesis is always an acceptable option.
Reconstruction of the Head and Neck Malignancy Defects with Scalp Island Flap Based on the Posterior Branch of Superficial Temporal Artery
In 1985, Small et al. described a case report of 78 years old male with an exfoliative tumour of the buccal mucosa adjacent to and involving the left commissure which had been excised and later reconstructed with the scalp island flap based on the posterior branch of the superficial temporal artery. A subcutaneous tunnel was made through the check and flap brought to the oral cavity. The major drawback according to them was that utility of the flap limited to the bald scalp only [8].
In 1984, Freeman et al. published their article on head and neck reconstruction with hair-bearing flaps based on the posterior branch of the superficial temporal artery. They used to delay the flap after 2 weeks of transfer and insetting was done at the end of three weeks. In their series of 22 cases, complications were very minimal [10]
Aytemiz et al. in 1991, published their article on facial and upper lip reconstruction with this flap. In the first case, they have described a 20 years old male patient with scarring and lack of the beard around the commissure and check as a result of an extensive burn. After excision of the scarred tissue, they made a subcutaneous tunnel and passed the flap from the donor site to the recipient site. In the second case, they have described a 45 years old male with scarring around the right oral commissure and the right upper lip following burn injury. The third case was a 21 years old young adult who suffered a burn injury during childhood and now requires reconstruction of the right eyebrow and left cheek. The right and left temporoparietal flaps are used for eyebrow and cheek reconstruction. The authors concluded that this flap is an excellent option for midface defects requiring beard and moustache reconstruction [7]
In our series, 5 cases of the head and neck defects were reconstructed with this flap and locations of the defects were at the buccal mucosa (4 cases) and the palate (1 case). Out of the 5 cases, two cases were recurrent ones, another two cases where primary flap failed (and scalp flap was done as a salvage option) and in the last case, the patient was unfit for free tissue transfer due to cardiac issues.
Conclusion
Scalp flap based on the posterior branch of the superficial temporal artery is a reliable and versatile flap. It is a useful option in recurrent malignancy cases, as a salvage option and in patients where long duration surgery is not possible due to poor general condition. Post-operative alopecia at the scalp is a concern and therefore, careful patient selection is a must.
References
Washio H (1969) Retroauricular-temporal flap. Plast Reconstr Surg 43:162–166
Leitner C, Hoffman J, Zerfowski M, Reinert S (2003) Mucormycosis necrotizing soft tissue lesion of the face. J Oral MaxillofacSurg 61:1354–1358
Jones AC, Bensten TY, Fredman PD (1993) Mucormycosis of the oral cavity. Oral Surg Oral Med Oral Pathol 75:455–460
Intercepting the deadly trinity of mucormycosis, diabetes and COVID-19 in India: Mainak Banerjee, Rimesh Pal, Sanjay K Bhadada; Correspondence to Dr Sanjay K Bhadada, Endocrinology, Post Graduate Institute of Medical Education and Research, Chandigarh 160012, India; bhadadask@rediffmail.com; http://dx.doi.org/https://doi.org/10.1136/postgradmedj-2021-140537
Garlapati K, Chavva S, Vaddeswarupu RM, Surampudi J. Fulminant mucormycosis involving paranasal sinuses: a rare case report. 2014
Spellberg B, Edwards JJr, Ibrahim A (2005) Novel perspectives on mucormycosis: pathophysiology, presentation and management. Clin Microbiol Rev. 18:556–569
C. Aytemiz and M. Sengezer; Use of the superficial temporal artery island flap for facial and upper lip reconstruction; Gulhane Military Medical Academy and Medical School, Ankara, Turkey
J. 0. SMALL and A. G. LEONARD; Posterior superficial temporal artery island flap for intra-oral; reconstruction: a case report;; British Journal of Plastic Surgery (I 985), 38. 488491: ‘I 1985 The Trustees of British Association of Plastic Surgeons; Northern Ireland Plastic and Maxilla-Facial Service, The Ulster Hospital, Dundonald, Belfast, Northern Ireland
V. Srikanth1 & Kumar N. Pradeep1 & Y. N. Anantheswar1 & B. C. Ashok1 & Reddy Sudarsahn1 & Rittu Bhath1: Cranio-facial mucormycosis—the plastic surgeon’s perspective: European Journal of Plastic Surgery. https://doi.org/10.1007/s00238-019-01606-x:Received: 18 December 2018 /Accepted: 27 November 2019
Freeman JL, Noyek AM (1984) Hair-bearing flaps in head and neck reconstructive surgery. J Otolaryngol 13(2):105–108 (PMID: 6726842)
Funding
This study was not funded by any institution or organisation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The author declares that there is no conflict of interest.
Ethical Approval
The study has been done as per ethical guidelines and appropriate consent has been taken before publication of the study material.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hiremath, S., Boro, S.S. & Mathew, A.K. An Experience of Scalp Island Flap Based on the Posterior Branch of the Superficial Temporal Artery for Patients with Mucormycosis and Cancer. Indian J Otolaryngol Head Neck Surg 74 (Suppl 2), 3139–3144 (2022). https://doi.org/10.1007/s12070-021-02860-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-021-02860-x