Abstract
Healthy diets have been demonstrated to complement benefits of physical activity, physical condition and mental wellbeing, all of them being important factors influencing the quality of life of elderly. Unfortunately malnutrition is a serious threat and an increasingly prevalent condition among the fast-growing elderly population. The present work addresses the identification of important factors contributing to decreased appetite and food intake as well as the development of approaches towards a healthy diet and personalised nutrition in elderly. Within the present study semi-structured interviews with elderly and elderly suffering from swallowing and mastication difficulties have been performed, results being used for the development of food provision modules and the corresponding recipes addressing the nutritional requirements of elderly. The social context and the swallowing and mastication difficulties influence the eating behaviour as well as the motivation to eat. On the other hand, it was found that texture modified foods (food which texture is adapted to the need of people with swallowing and mastication problems) could act as motivational aspect. With regard to food personalisation in the elderly the consideration of three different case scenarios based on individual independency and the degree of oral impairment seemed to be appropriate. Different aspects such as gender weight, physical activity level as well as high protein demand are important influential factors in the development of personalised recipes in elderly. In addition to the above, a conversational agent was developed as behaviour change module and can be successfully used as smart personal assistant in helping the users to understand their eating habits and adopt healthier nutrition over the long term.
Similar content being viewed by others
Introduction
Oral ingestion (drinking, eating) is one of the most important actions of the day during ageing. Thus, it also contributes to good health as well as representing a limiting factor of suffering from chronical diseases. In contrast, malnutrition in the elderly favours the risk of chronical diseases such as Sarcopenia (the loss of muscle mass during ageing) which in fact leads to a decrease / absence of physical activity (Corcoran et al. 2019). In relation to this, the European Society of Clinical Nutrition and Metabolism (ESPEN) defines malnutrition due to ageing as “a state resulting from lack of uptake or intake of nutrition leading to altered body composition (decreased fat free mass) and body cell mass leading to diminished physical and mental function and impaired clinical outcome from disease” (Cederholm et al. 2015). Up to 85% of elderly long-term-care home residents are malnourished (Nieuwenhuizen et al. 2010). Besides, there is an association between chewing and swallowing disorder and the nutritional status of older adults. The fear of eating properly, of choking and the decreased palatability of texture-modified food could lead to unwillingness to eat and as a result it may lead to deficient nutrient intake (Foley et al. 2009). In 2005 Wright et al. reported that only 45% of long term care patients, suffering from swallowing and mastication problems, meet their energy requirements. Other reasons negatively affecting the motivation to eat and thus being possible causes of malnutrition within elderly population have been found to be: i) psychological aspects such us depression, leaving the usual environment (e.g. moving into a nursing home etc.), loss of relatives / friends and consequently social interaction; ii) physiological factors such as the inability to prepare the meals, the dependency on caregivers (Donini et al. 2003), impaired physiologic functions (limitation of sensory abilities) (Engelheart et al. 2006) as well as iii) pathological reasons related to e.g. several medications (Donini et al. 2003). Under this context, food recommender systems have received increasing attention to help people adopting healthier eating habits, but the number of existing systems is relatively low (Trattner and Elsweiler 2019). These systems mainly focus on suggesting proper food items based on individuals’ preferences and health conditions (Burke et al. 2011). Nevertheless, despite the extensive research and the existing nutrition applications, food recommender systems are still facing many challenges in terms of nutrition habits tracking and delivering proper recommendations (Mika 2011). Furthermore, they also do not consider the use of texture modified food (food which texture is adapted to the need of people with swallowing and mastication problems) products. Additionally, the users often find it difficult and time consuming to enter manually their food every day in the system. Actually many studies are also facing the uncertainty of the information given by the users as they may not know or tend to forget what they have eaten. This makes it more challenging for the system to recommend the correct food item. Studies have shown that generally the food recommendation provided by the majority of such systems is not followed necessarily by the user in terms of change in its eating behaviour (Konstan and Riedl 2012). Beside this, dietary recommendations mostly aim to decrease the occurrence of malnutrition in the general population and do not consider the individual nutritional needs (Celis-Morales et al. 2016). In addition, aside from dietary recommender systems there is also a need to adopt behaviour change techniques with regard to the elderlies eating behaviour.
Under this context, within the REACH project the nutrition is seen, as fundamental aspect in elderly, not only justified by the high rate of malnutrition among this population group, but also by its relation with physical activity. Thus, within the present study insights on aspects influencing food intake have been collected through semi-structured interview with elderly citizen (>60 years) and used as starting point for the development of a scenario-based personalised food provision module. Additionally behaviour change aspects have been addressed through the development of a smart personal food assistant.
Qualitative Analysis of Semi-Structured Interviews: Detecting Motivational Aspects Influencing elderly’s Food Intake
Semi-structured interviews comprising 63 elderly (40.5% male and 59.5% female; 50% > 80 years, 42.1% 71–80 years, and 7.9% 60–70 years) capable of eating regular food and 92 elderly (69% female and 31% male; 5.6% 60–70 years, 20.2% 71–80 years 73.3% > 80 years) affected by swallowing and mastication disorders have been conducted in three different European countries (Germany, The Netherlands and Denmark). Specific questionnaires have been used for each of the two elderly groups aiming to collect insights and opinions on aspects such as healthy nutrition, food, eating habits as well their states of mind and how these possibly affect their eating behaviour.
Elderly Eating Regular Food
59.4% of the interviewed consider food and/or eating important or very important while 16.2% stated that eating is not important or not important at all. The majority (89,5%) of the participants are able to eat by their own, while 10.5% need help from care personnel or relatives. Only 31.4% are able to eat entirely their meals. This leaves an enormous percentage of elderly (68.6%) which are not able to finish their meals, the main reason indicated (50%) being that “it is simply too much food”. Beside this, 43.2% of the participants reported that their current situation (e.g. living in a nursing home) affects their mood negatively and decrease their appetite (18, 9%). Sadness (27.3%), loneliness (24.2%), annoyance or dejection (15.2%) and depression or boredom (6.1%) were the major reported feelings. In line with that, 55.3% of the interviewed consider important to eat their meals together with other people. With regard to nutrient supplementation of the food, 50% want to know what nutrients are added to their food. 15.8% of the participants consider that is a good idea to incorporate the supplements directly in their food and/or drink without knowing what nutrients are supplemented.
Concerning the importance of sensory properties of the food (taste, smell and appearance), taste has been reported as the most important aspects by the respondents. Smell and appearance are also of high consideration. However, it has been found that the importance of smell decreases by increasing age, while opposite results have been obtain when analysing the importance of taste. Elderly respondents over 80 years stated that appearance is more important than smell. 65.8% indicated that this also applies in the case of pureed food thus, appearance of the food being perceived as a strong motivational aspect to eat. 63.2% of participants indicated that they would accept food with different taste as they might be used to, if this food would answer their nutritional needs.
Concerning nutritional knowledge, 34.3% of participants stated that they are not or not at all informed about healthy nutrition. 40% considered to be good or very good informed about healthy nutrition and 25.7% indicated that they have average knowledge on healthy nutrition. Besides, 14.3% of the interviewed considered important or very important to receive information (either by caregivers or by an App) about the benefits that a certain diet or certain food may provide them. In contrast, 45.7% considered it not important at all. However despite the above, nearly 90% of the participants did not receive any food intake documentation or are following a specific diet while 71.1% stated that they are not willing to track their diet. It has been found that 36.1% of the respondents think that tailor made food (food made specifically to the person’s needs) are important or very important for their health; 30.6% do not think that it is important for their health and 33.3% are on average level. Finally, more than one third of the interviewed highlighted that they expect to “eat healthy” when following a tailor made food diet.
Regarding the frequency of their general nutritional related check-ups (including weight or body values such as muscle or fat percentage), 26.3% of the participants revealed that they are never checked-up, 44.7% undergo a monthly check-up and 7.9% have weekly or daily (5.3%) check-ups. Additionally, 65.8% of the participants stated that they received the relevant information regarding the results obtained within the check-ups.
Elderly Suffering from Swallowing and/or Mastication Disorders
77.8% of the elderly reported that food is important or very important in their life. Only 20.7% of the participants are still able to eat on their own, the rest of them needing help during eating. A high percentage of the interviewed (55.6%) stated that they are not looking forward to eat due to aspects related to their chewing and swallowing disabilities (e.g. pain while eating normal food, choking). Even more, it has been found that only one third of the respondents usually finish their meal as the portion served is too big (55.6% of the respondents) or they do not like the appearance (11.1%). In addition, 60% of the participants indicated that their motivation to eat is affected or strongly affected by their swallowing and / or mastication disorders. All the respondents reported that their disability to eat normal food affects their overall mood, while 60% reported that it affects their mood but also their appetite. The most common feelings while eating have been indicated to be depression (22.2%), indifference (11.1%), loneliness (33.3%), dejection (11.1%) and shamed (22.2%). Furthermore, none of the elderly has ever had measurements of their degree / impairment of swallowing. Additionally, 55.6% the participants consider important to eat together with other people, 33.3% of the respondents reporting an increased food intake under these conditions. Over half (55.6%) of the interviewed need to take nutritional supplements. One third of the respondents would like to directly incorporate these supplements into their food and / or drink as they think the less pills, the better while one third would like to see what is added to their food and / or drink.
Regarding the sensorial attributes of the pureed food, 62.5% of the participants reported that the appearance of food is the most or a very important sensorial aspect of the food. 87.5% of the respondents mentioned that the taste is important or very important while only 37.5% attributes the same importance to the smell. Besides the taste, the serving of the meals have been found to be the most important quality factor. 75% of respondents consider this attribute significant. 58% of the affected elderly are served by shapeless purees while 42% are served with shaped puree (e.g. by a scoop). In relation to the possibility of reshaping the pureed food into their original shape (e.g. smoothfood® components) as a mean to increase its appearance and attractiveness, 33.3% of the interviewed stated to be looking forward for such food as they will be able to identify the single components. 8.3% of the participants indicated “it tastes better” when reshaped while another 8.3% mentioned that they eat more when the food is reshaped. With regard to the preferences of different food categories, 77.8% of respondents mostly like / like a lot the serving of vegetables. 22.2% neither like, nor dislike vegetables. Analogous answers have been found with regard to meat category. Carbohydrate based foods did not register negative opinion. 55.6% of the respondents indicated that they would accept food with different taste, if the food would answer their nutritional needs completely.
77.8% of the interviewed are not following a special diet. None of the elderly think that the communication of the benefits for eating certain foods or following a certain diet is important. Food intake is not documented in the majority of elderly (approx. 80%) while 77.8% stated that they do not want to track their diet. 33.3% of the interviewed think that tailor made food is important or very important, 11.1% think that is not important, while the rest of the respondents have a neutral opinion. “Eat healthy” is the main reported reason why personalised food would be important.
55.6% of the respondents are undergoing monthly nutritional related check-ups (including weight or body values such as muscle or fat percentage). Approximatively a quarter of the elderly answered “weekly” or “never” while, 77.8% of the elderly interviewed are also informed about the results of their status check-ups.
Personalised Food Provision Module
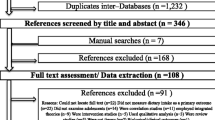
Prototype personalised food provision module (MS Excel based programme), which consider among others the individual independency (with regard to food preparation) and the degree of oral impairments was developed within REACH context. Thus personalised recipes and culinary guidelines as well as specific products and applications have been created (on a four meal / day base: breakfast, lunch, dessert / snack and dinner) addressing the specific needs and requirements of the individual elderly. These guidelines address the different aspects of the individual such as physical activity level, special dietary recommendations (e.g. higher protein content), weight, gender etc. As the performed interviews showed that elderly often do not consume their entire meals, strategies such as food fortification and supplementation were also implemented. Two different possibilities have been taken into account within the food provision module: elderly able to consume regular food and elderly requiring texture modified food (due to different oral impairments). Further, the option of cooking by themselves or catered by centralised cooking (e.g. nursing homes) has been taken into account for elderly able to consume regular food. This option was not considered for the elderly requiring specific texture modified food, as in their large majority such individuals are not able to cook by themselves. Thereby, three main scenarios have resulted and implemented within the food provision module (Fig.1):
In the first Scenario (S1), the elderlies are living independently at home and are self-supplied with food. They are cooking by themselves and can also eat with a friend/partner or family. Scenario 2 (S2) and Scenario 3 (S3) separate the people with regard to the eating capability -normal food or smoothfood® (texture modified food)-, both being supported by centralised cooking. These elderly are for example living in a nursing home or a hospital and the food is provided directly to the rooms / bed or a group hall. While in S2 people are able to consume the usual food, S3 represents a special case, as they need pureed food and thus texture modified menus have been developed and used specifically for elderly with Dysphagia (swallowing and mastication problems) or other oral impairments. It already became clear, based on the interviews performed, that for this specific group (elderly within S3 Scenario) a high supplementation as well as the development of such texture modified menus with increased visual appearance, as nutrient enriched alternatives to the standard puree food, were necessary to be implemented within the food provision module. For example, it is worth to mention the development of gelled bread, such product being the first of its kind on the market. One of the biggest advantage of such gelled sliceable bread is that it is offering a real breakfast experience (e.g. spreading marmalade or butter on a slice of bread) to people which normally could not have such experience anymore (due to the impossibility of chewing respectively swallowing normal bread).
Nutritional values from different ingredients together with up to entire meals have been identified based on the German Society of Nutrition (DGE; DGExpert database), serving as basis for calculating the nutritional data of the meals and the respective development of personalised recipes. The individual nutritional needs were calculated using specific data such as weight, sex, age and specific dietary requirements. Furthermore, the developed recipes have been tested and an initial 28-day meal menu (four weeks) was built according to the usual practice within nursing homes (four-weeks-rotation-principles). Recipes were designed to be easy to prepare and to decrease the workload of a chef (or kitchen team) in centralised cooking. In order to create usable data, general information from DGE was used in order to calculate the appropriate demands of energy, carbohydrates, protein and fat. Thus, the Resting Energy Expenditure [kcal/day], meaning the lowest need of energy without any movement, fulfil the basis of the calculation. By enclosing the “physical activity level” (PAL = a measurement for the physical activity with a range from 1.2 (e.g. bedridden people) up to 2.4 (e.g. athletes)), the precise needs and requirements of the individual elderly could be identified.
Scenario 1
Scenario 1 includes elderly living independent at home and able to take care of themselves (e.g. grocery shopping, cooking). As loneliness was one of the main feelings reported during the interviews within the food provision module it has been included the option to invite for eating and cooking up to three people. This enables the elderly to cooking and eating together, as a mean for motivation and socialising.
For this group of elderly, the goal is to motivate them towards a personalised nutrition by cooking and providing personalised easy but tasteful recipes over the whole day. Therefore, the recipes are written in such way that single steps could be attributed to each individual (e.g. while person 1 is cutting potatoes, person 2 is boiling the meat). As a consequence every individual, attending the meal, can directly take part to the recipe preparation, presenting thus more attention to the socializing aspect. Official guidelines and practices within elderly nutrition (e.g. DGE practical knowledge – eating and drinking in old age), have been considered during the recipes development following as well a food cycle approach.
The Scenario 1 food provision module has been called FIRE- ‘Food Ideas & Recipes for the Elderly’ and has been developed, integrating all previously created recipes. FIRE is suggesting meals ideas and recipes, considering the individual nutritional needs, and parameters such as body weight, and gender. Furthermore, the physical activity level is included within the nutritional calculations for each individual. Elderly are able to choose from 28 different designed meal plan for each day and get recipes for breakfast, lunch, dessert/snacks and dinner (from now onwards noted as BLDSD) with the individualized/ personalised amount of ingredients for each person. Within the ‘User Interface’ (Fig. 2), the user is required to input on physical data: gender, bodyweight and physical activity level (PAL) for each person attending the meal. For providing a better understanding, the physical activity level is explained in a separated frame and visible while entering the details. The parameters ‘gender’, ‘PAL’ and ‘number of persons’ is included in a dropdown menu, in order to avoid incorrect entries such as multiple answers for the gender (man, male, masculine, etc.), PAL which is too high etc. The necessary nutrient requirements, specifically for each individual, are assured independent of the day / meal preferences chosen.
Based on data provided in ‘User Interface’, the individual requirements in terms of energy intake as well as macronutrients are calculated automatically and displayed. Each meal included within FIRE, has been developed in such a way to fulfil the official macronutrients recommendations for elderly nutrition, namely 55% carbohydrates, 30% fat and 15% protein (DGE-key). These percentages were used as main requirement and basis for the macronutrients calculations & algorithms interconnections with ingredients used and consequently recipes been established. Once the DGE-key has been fulfilled, the individual meal sizes are calculated and adapted to each individual requirement. A large amount of ingredients (e.g. chicken, egg, cow milk, pork meat etc.) together with their respective energy as well as all macro- and micronutrients details have been included in FIRE. Ingredients have been listed in English, as common international language. Once a certain ingredient is used within a recipe the respective energy together with the macro (and micronutrients) appears automatically, such information being further used by the programme background calculations. Depending on the overall energy content per meal, the macronutrients are calculated in percentage. Beside this, in order to simplify the fulfilment of DGE-key, a colour code has been establish so that the values are coloured in red if the requirements are not fulfilled and in green if they are fulfilled. At the end of a day, values (in percentage) will be summarised and displayed. However, it has to be highlighted that it is more important, to achieve the DGE-key at the end of the day, rather than for every single meal.
Beside this, FIRE calculates and provides information to the user with regard to the amounts of ingredients needed for preparing the meal, values being also automatically rounded. Further, the calculated meals are summarised and highlighted as a pie chart (Fig. 3), to visualize the size, every individual shall eat (in case more elderly eating at the same time and using FIRE). The pie charts are dynamics and react automatically to all entered details, including the amount of persons.
Final recipes, significant calculations and instructions are highlighted into a user-friendly understandable format. The recipes are ordered per day from left to right (BLDSD) and below each other. They are written in a simple way using bullet points and require only basic cooking knowledge. In order to consider individual preferences, each recipe includes personalized suggestions (e.g.: Enjoy the ingredients as you wish).
Scenario 2
As similar to Scenario 1, within Scenario 2 also a 28-day meal plan consisting of 4–5 meal per day was created in collaboration with high experienced chefs in the area. Concerning the menu, different categories were established (meat, fish, potatoes, pasta, rice, vegan/vegetarian, sweet) and used roughly for the recipe application. Thus, a balanced diversity in meals was ensured, the maximum amount of recipes of one kind (e.g.: pork meals) being limited, while at the same time recipes of another kind (e.g.: vegan) were also created. The recipes were defined in accordance with BLDSD. An additional food provision module have been created specific for Scenario 2 and was named Food for elderly people- FEP, incorporating all above mentioned recipes and providing a full personalised nutrition for up to 20 people at the same time with access to centralised cooking conditions. Based on the individual data entered by the staff (name, gender, weight, PAL and possible higher protein demand), FEP calculates and displays the nutritional data for each individual (energy demand, carbohydrates, protein, fat) for a week, separated into single days, divided by meals (BLDSD) (Fig. 4).
In order to develop personalised recipes and culinary guidelines (on a 4–5 meal/ day base: breakfast, lunch, snack/dessert and dinner) addressing the specific needs and requirements of the individual elderly, the basic idea was to support also the chef (or kitchen team) in centralised cooking. For this reason it was decided that as fundamental approach the meals have to be equal for every individual while higher nutrition requirements being completed through fortification of specific meal components (e.g. liquids like sauces, to blend the fortification properly), if needed. Thus, a chef will need lower time for producing the personalised menus. Specific formulas and algorithms have been developed and integrated in the FEP, calculating the nutritional needs (kcal, carbohydrates, protein, and fat) for each individual and further, based on the defined recipes providing in accordance the meal together with the necessary fortifications. At the end of a day, the status of the nutritional data for the single meals (BLDSD) and the consumed amount in percentage for each person is summarised and highlighted, based on the same calculations approach as explained in Scenario 1. A colour code has been used for providing the nutritional status. Namely, if a previously calculated specific limit is exceeded, the value is displayed green, otherwise it is displayed red. This allows a fast and simple overview. When creating the menus the financial represented a decisive aspect, considering that the overall cost/meal/day/person are maximum 5 Euros. As a result, the menu was created in a compressed way, so that with a relatively limited number of ingredients a high number of meal possibilities can be assured, while keeping the overall menu appealing without creating a meal satiety feeling. As an example: ham as breakfast on bread, in the pasta sauce for lunch and under the fried egg for dinner. At the same time, there is a boiled egg provided within the breakfast and for dinner a fried egg, all in one day. By this approach a high amount of single ordered products accompanied by a lower price (high order amounts result in lower prices), with saving in overall storage space and with a simplified working task for the kitchen team can be achieved. This minimise the food waste generation and the risk of food microbial spoilage. Elderly people are more vulnerable to microorganisms and their metabolic products, due to their frail immune system. To avoid spoilage threads, storage time for sensitive ingredients is minimised. Thus within the menu planning such ingredients are reused within a maximum of 4 days. In this way, possible resulting hazards are excluded.
For the first attempt in developing a 28-day menu, an average simulation environment was created, containing previously defined ranges for single parameters. The PAL was estimated with 1.2 up to 1.6 to include elderly with a high movement (Table 1).
Initially the consumed amount was estimated with 60% - 140% to simulate the case, that the portion is too big or that some of the residents may require a second serving. After first simulation and evaluation with high experienced chefs within the area it was found, that PAL value was stated unrealistic high (such situation being not normal within nursing homes), resulting in a low accuracy. There was a fluctuation in nutritional need between different simulations of up to 1500 kcal (example: People with a high weight and high PAL were supposed to eat more than 100% more food, compared to lightweight people or people with a lower PAL). The fluctuation was too high and it was considered, that a consumed amount of more than 100% is unusual, this being supported also by the interviews gathered. As a result, the consumed amount was decreased from 140% to 100%. Within the second running simulation, the PAL was set to a range of 1.2–1.4. Beside this, it was figured out, that the overall amount of food per serving was too high (e.g.: 750 g of pasta bake), an average of 475 g per serving (this suits the most people) being established. Even more, instead of three meals per day (as in the initial simulation) 4–5 meals per day have been considered more appropriate. Thus, the servings could be reduced to an edible size, optimisations of the FEP program being implemented accordingly. Under these conditions the span of the overall consumed amount of the dishes was changed to 85% - 100%. Furthermore, an upper limit in the case of exceeded nutritional values was necessary to be defined. For example, even so, an average for fat to be consumed, during programme simulation run, was 61.4 g/day, it was noticed that for some weekdays, this limit was exceeded by more than 100%. For providing an upper limit for orientation, a simulation resident was created: a man of 120 kg, with a PAL of 1.6 and an always consumed amount of 100%. Further, based on body mass index (BMI), a value for the nutritional average was designed as a point of orientation (PO). The BMI is a value for the description of weight, in dependence of a rough calculated body surface. The formula used for calculating the BMI is:
A BMI between 20 and 24 states a “normal weight” (a state where the possibility of weight-caused diseases is the lowest) while between 25 and 30 states “overweight” (a state where diseases of the metabolic syndrome become possible). Further different PAL levels had to be considered within the PO. By choosing the calculated POs 1762 kcal/ 1740 kcal for both men and woman, it was ensured the provision of sufficient amount of nutrients by the programme calculations. At the same time, the work of the kitchen chef with regard to the necessary fortifications for completing the individual nutritional needs can be eased. Further as an additional principle, a meal component specific fortification limit (nutrient supplementation) was defined. Thus, sensorial test with different food components as well as supplements were performed. For example, maltodextrin, dissolved in mashed potatoes, tastes sweeter compared to maltodextrin dissolved in goulash sauce. As a result a specific food fortification limit was identified and incorporated in FEP, assuring the maintenance of similar sensorial attributes as the initial meal components.
Scenario 3
Within Scenario 3, the already defined features of the previously developed Food for elderly people- FEP programme of Scenario 2 have been used, with the exception that modified texture food recipes had to be developed and replace the regular food recipes. Menu was created in addition to the Scenario 2 and has a parallel order and comparable or equal meals, considering residents suffering from dysphagia. Such residents are requiring texture modified food. It was taken care, that most of the meals are prepared as usual and pureed and reshaped afterwards, thus considerably improving their overall appearance. By preparing texture modified food, 25–50% of the component has to be stock up with water, which can result in a lower (weight to weight) the nutritional value. However, this is not having a strong influence, as it is known that elderly suffering from Dysphagia usually possess a lower PAL in comparison to other elderly, which results into a lower energy demand. As similar to Scenario 2, a fortification-step was enclosed to the recipe development. However, within this Scenario the fortification has a stronger impact especially that, as demonstrated by the interviews performed, a high percent of elderly are not consuming entirely their meals. The programme FEP allows seeing the difference between nutrient requirements and possible nutrient intake of a certain menu, providing at the same time a simply to choose appropriate nutrient fortification. In addition to developments of gelled food, also foamed food recipes have been created and included within Scenario 3 (FEP) (Fig. 5). Actually, initially all developed recipes of Scenario 2 were analysed with regard to the possibility of texture modifications. Several meals for which texture modification could not be implemented (e.g. negative sensorial attributes) have been rejected / replaced with new defined ones. Generally cheese based recipes (e.g. gratins) were not suitable for texture modifications. However, those represented a relatively low amount, the majority of the meals being successfully gelled and / or foamed. Thus, within Scenario 3, innovative recipes/ meals with superior features (e.g. special texture, high solubility (for fortification purposes) etc.) were successfully developed. Unlike current dysphagia diets, which are mostly based on purée and pre-mashed food and result in loss of appetite, eventually leading to severe malnutrition, the final modified texture recipes/ meals developed within REACH are replicating the look and taste of” real” food. Additionally, gelled bread has been developed. Serving normal bread to Dysphagia patients is not possible; due to small crumbs and the solid crust which cannot being chewed and swallowed properly. Thus, special modified texture bread (smoothBrot) has been developed and included into the FEP, serving a real breakfast experience. It has the taste of the bread, from which it is made of. It is firm and cut resistant, in contrast to already existing pureed bread. Spreadable sausages, creams and purees can be applied fresh. It can be squeezed between tongue and palate and be held in the hand, without losing its shape.
The personalised food provision module of Scenario 3 comprises a 28-days full menu plan. Within the FEP, up to 20 persons can be included; name, gender, weight, PAL as well as the additional question if a higher protein demand is necessary have to be entered by the personnel accordingly. After entering the personal data, the energy demand/ day/ individual is automatically calculated and separated into the macronutrients: carbohydrates, fat and proteins. These represent the necessary personalised nutrient requirements as well as the basis information for the further FEP calculations for portions and nutrient fortifications. All the modified texture recipes developed for Scenario 3 have been included in the FEP and linked with the already existing ingredients list (based on Scenario 2). As to Scenario 2 the ingredients are listed with all the amounts of macro- and micronutrients, nutrient calculations being performed automatically. However, adaptation steps with regard to recipe data (name of the recipe as well as energy demand, carbohydrates, fat and protein) and its necessary links to the input interface were necessary to be performed. For each menu (and the respective recipe links), same order as in Scenario 2 was kept, namely breakfast, snack, lunch, dessert, dinner. As interviews performed revealed that food intake is usually not recorded, the opportunity for the nursing home staff to input in FEP the approximate amount (in percent) eaten by each individual, has been included. By this, a further nutrient adaptation can be implemented within the program. At the end of each day the daily intake is calculated on the basis of actual consumed amount of the meals. The nutritional status is calculating the differences between the actual daily intake and the recommended daily intake, necessary nutrient fortifications being also calculated. By using FEP the kitchen staff knows in advance how much a meal needs to be enriched (plus the nutrient) to meet the nutritional needs of an individual. It has been demonstrated through the trials performed that all types of sauces, curd and soups are suitable for fortification. Even so it is not feasible to personalise every individual meal without additional workload for the chefs, by using the FEP a high personalisation can be achieved while keeping a minimum workload for the kitchen staff.
Within REACH, 3D printing tests have been performed in order to identify its feasibility for producing modified texture foods, complementing the classical reshaped mould based procedure (used in Scenario 3). Such technology represents the first steps towards the future automation of modified texture food production systems. Within this context, fused deposition modelling is the most commonly used technology of 3D food printing. Within this technology, an extruder is building a selected shape by squeezing a defined amount of puree at a defined place- layer by layer. During the project, feasibility of texture modified 3D food printing could have been confirmed, printing different main meal (pureed and texture modified) components (peas, carrots, potatoes, chicken, pork) back into their original shape. Additionally, desserts (apple puree, chocolate mousse) printing feasibility could have been confirmed, too.
Sensing Module: MiranaBot
Further, the REACH approaches towards personalising nutrition have been commented by the development of a conversational agent called “MiranaBot”. MiranaBot aims in helping the elderly to be aware of their eating habits in terms of variety and regularity. This is especially important for elderly included in Scenario 1. Rather than focusing on food quantity and nutritional value, the system targets the variety of the individuals’ diet. From a regular description of the elderlies’ meals during a certain period, MiranaBot is able to assess the quality of their nutrition, identify the foods they need to consume less and explain why and how to replace them. The system proposes personalised solutions tailored to the older adults’ needs and context. It can also represent a useful tool in behaviour change, especially through several aspects included such as self-monitoring, personalised visual feedback, goal setting, self-awareness and personalised education. (Fig. 6)
Self-Monitoring
MiranaBot allows the users to track their nutrition easily by asking them to describe briefly, what they ate after each meal in terms of portions. The system will initially train the users on the portion size to help them describe their meals as best as possible.
Personalised Visual Feedback
MiranaBot provides visual feedback every day regarding nutrition variety and regularity. Food variety is illustrated on a plate showing the ratio of proteins, carbohydrates and vegetables consumed by the user versus the optimal plate suggested by the Swiss Society of Nutrition (Swiss Society of Nutrition). A visual watch resuming the elderlies eating times is intended to encourage self-reflection on their nutrition regularity.
Goal setting: Following a training period analysing the eating habits of the users, MiranaBot allows them to set personal goals, such as “eating three meals a day” or reducing “bread” and to define a timeline to reach their goals. Prompt reminder and useful information are pushed to help users reach their goal.
Self-awareness: MiranaBot raises awareness of real physical hunger by asking users how they are feeling before and after each meal.
Personalised Education
MiranaBot is developed to be continuously available to answer users’ questions during the process of change. Advice on food item alternatives, benefits of healthy nutrition behaviour and promptly reminders towards their personal goals are delivered frequently.
MiranaBot is composed of four main components: the speech to text module, the text analysis module, the natural conversation module and the graphical user interface. Additionally it contains an extra component called “Nuggets” which represent the results of analysis after a certain period. For example, a Nugget could refer to bread consumption, then the recommendation of the natural conversation module or the Graphic User Interface Module would be: “let’s reduce bread consumption by ¼ for a week. Here is what you can eat instead of bread” (Fig. 7).
Speech to Text Module
Users can easily describe, vocally, what they have eaten after each meal. This voice description is then converted in real time into text using DialogFlow, Google’s human–computer interaction technologies based on natural language conversations. MiranaBot is available in English as international language.
Text Analysis Module
MiranaBot analyses users’ every day food data to provide them with daily and weekly visual feedbacks. MiranaBot also detects frequencies, varieties, and quantities (in terms of portions) of a specific food (or category of food). It uses a food database classified by different food categories. Rules have been set for each category which are then used by the algorithm to identify recurring patterns (e.g.: too much bread = more than the required consumption defined by the rules).
Natural Conversation Module
An important functionality of MiranaBot is its ability to discuss, have a conversation and answer the questions from the user. As mentioned previously, the conversational module is built upon DialogFlow. This module uses machine learning for small talk conversations to recognize user basic questions. In addition, case specific intents were developed (or functions) enabling the MiranaBot to answer specific nutrition related questions.
Graphical User Interface
To maximize the output provided to the user, MiranaBot uses the screen of the host device (phone, tablet, and computer) to display graphical feedback in addition to the vocal answers. The regularity of the nutrition and the variety of the food eaten by the users are displayed on the screen to induce better self-reflection. While describing the food, the user can also check, in real time, if what he said was transcribed correctly. In case of error, the user has the possibility to edit the entry through the graphical user interface. The user interface is also used to share articles, tips or to send useful notifications to the user.
Conclusions
Within this study, specific insights on motivation, action and patterns regarding food intake in elderly have been gained. The research revealed the strong influence that the social context has on the eating behaviour and that eating in groups might be a good motivational strategy for the majority of elderly. It highlights the importance of supplementing the meals in order to avoid prevalence of malnutrition. The majority of elderly are not able to consume the entire portions, which are usually served, which results in a diminished intake of nutrients. This might be one of the basal reasons in the prevalence of malnutrition. Results also show the strong necessity of decreasing the meal volume while increasing nutrients through supplementation. It also highlighted the necessity of frequently monitoring the general nutritional status (e.g. body weight, lean body mass, etc.) as well as properly communicating the necessary of nutrient supplementation to each consumer. Furthermore, the study confirmed the influence that the meals sensory aspects have on food acceptance as well as their relation with aging. On this respect, it can be stated, that the importance of taste and appearance are higher with increasing age, while the importance of smell is decreasing. The research outlined a strong connection between suffering from eating difficulties (mastication and swallowing disorders) and decrease of food intake. The majority of the respondents feel that their motivation to eat is greatly affected by their difficulties while eating as well as their mood. Moreover, high percentage of elderly with swallowing and mastication problems is not looking forward to eat because of their mastication and swallowing difficulties. This highlights the importance of serving special developed tailor-made texture food for meeting their needs. Beside this, results have shown that texture modified food (such as smoothfood®) can be the solution to increase nutrient intake and serve as motivational aspect to eating behaviour of elderly. Thus, nutrient personalisation concepts shall also consider its use to a larger extent. Such foods register high appreciation among this population group, considerably improving their eating experience. Even more, due to its improved visual and appetising appearance such food can be seen as a strong motivational aspect for eating. Food personalization in elderly is possible and feasible but has to rise in priority within elderly diets. Due to different requirements (e.g. special texture food, incapacity of cooking) approaches in food personalisation has to consider various scenarios. Extensive nutritional differences can be recorded between different elderly; therefore, an individual base nutrition approach as FIRE and FEP could represent a suitable approach for assuring appropriate nutrient intake. It is also clear that independently living elderly have different requirements and purposes to use personalised nutrition as elderly living in nursing homes and/or hospitals. It has to be taken into account, that feasibility and practicability is always of highest importance, especially for personalised nutrition concepts addressing to institutionalised elderly (centralised kitchen). Even more as physical activity is interconnected to nutrient requirements, this parameter is essential for the successful implementation of a personalised nutrition concept. The different personalised food provision modules described in this paper, give adaptable suggestions and assistance dealing with elderly nutrition, incorporating three different possible simulation cases. Further clinical intervention studies are necessary to be performed in order to demonstrate the exact influence of the different personalised nutrition strategies with regard to their influence at individual level and in prevalence of malnutrition. Overall limitation in the development of food related recommending systems is the inability to identify the exact nutrient intake, when the meal is not completely consumed. The leftover food components are usually mixed on the plate, and therefore the remaining nutrients cannot be estimated accurately. This limits the efficiency of further nutrient corrections. Especially for independently living elderly, but not limited to, an improved understanding of diet and related nutritional aspects, as well as behaviour change strategies has to be implemented for successful food personalisation. MiranaBot has the potential to answer such needs of a descriptive nutritional assessment for the elderly and also to act as a recommendation and behaviour change system to promote healthy eating. Nevertheless, this domain is still in its nascent age. The efficacy of such tools to identify users’ nutritional habits and assist the user in the process of behaviour change would require further investigations. There is still a lack of understanding in how to incorporate efficiently behaviour change techniques into a food recommender system.
References
Burke, R., Felfernig, A., & Goker, M. H. (2011). Recommender systems: An overview. AI Magazine, 32, 13–18.
Cederholm, T., Bosaeus, I., Barazzoni, R., Bauer, J., van Gossum, A., Klek S., Muscaritoli, Nyulasi, I., Ockenga, J., Schneider (2015). Diagnostic criteria for malnutrition- an ESPEN consensus statement, Clinical Nutrition, 34, 335–340.
Celis-Morales, C., Livingstone, K. M., Marsaux, C. F. M., et al. (2016). Effect of personalized nutrition on health-related behaviour change: Evidence from the Food4Me European randomized controlled trial. International Journal of Epidemiology, 46(2), 578–588.
Corcoran, C., Murphy, C., Culligan, E. P., Walton, J., & Sleator, R. D. (2019). Malnutrition in the elderly. Science Progress, 102(2), 171–180.
Donini, L. M., Savina, C., & Cannella, C. (2003). Eating habits and appetite control in the elderly: The anorexia of aging. International Psychogeriatrics, 15(1), 73–87.
Engelheart, S., Lammes, E., & Akner, G. (2006). Elderly peoples’ meals. A comparative study between elderly living in a nursing home and frail, self-managing elderly. The Journal of Nutrition, Health and Aging, 10(2), 96–102.
Foley, N. C., Martin, R. E., Salter, K. L., & Reasell, R. W. (2009). A review of the relationship between dysphagia and malnutrition following stroke. Journal of Rehabilitation Medicine, 41, 707–713.
D-A-CH-German, Austrian and Swiss Society of Nutrition, (2000):D-A-CH- c (reference values for nutrient intake), Umschau/ Braus, 1. Edition.
Konstan, J. A., & Riedl, J. (2012). Recommender systems: From algorithms to user experience. User Modeling and User-Adapted Interaction., 22(1–2), 101–123.
Mika, S. (2011). Challenges for nutrition recommender systems. Proceedings of the 2nd workshop on context awareness in retrieval and recommendation.
Nieuwenhuizen, W. F., Weenen, H., Rigby, P., & Hetherington, M. M. (2010). Older adults and patients in need of nutritional support: Review of current treatment options and factors influencing nutritional intake. Clinical Nutrition, 29, 160–169.
Swiss Society of Nutrition: Balanced Diet- Optimum Plate [online] http://www.sge-ssn.ch/fr/toi-et-moi/boire-et-manger/equilibre-alimentaire/assiette-optimale/ [13.09.2019].
Trattner, D. & Elsweiler, D. (2019). Food recommender systems: Important contributions, challenges and future research directions. In collaborative recommendations: Algorithms, practical challenges and applications, Shlomo Berkovsky, Iván Cantador and Domonkos Tikk (Eds.). World scientific publishing.
Wright, L., Cotter, D., Hickson, M., & Frost, G. (2005). Comparison of energy and protein intakes of older people consuming a texture modified diet with a normal hospital diet. Journal of Human Nutrition and Dietetics, 18, 2013–2019.
Acknowledgements
The research leading to these results has received funding from the European Union’s.
Horizon 2020 research and innovation programme under grant agreement No 690425 and from the European.
Union’s Seventh Framework Programme under grant agreement No FP7-312092.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rusu, A., Randriambelonoro, M., Perrin, C. et al. Aspects Influencing Food Intake and Approaches towards Personalising Nutrition in the Elderly. Population Ageing 13, 239–256 (2020). https://doi.org/10.1007/s12062-019-09259-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12062-019-09259-1