Abstract
Introduction
Mitral valve repair is the accepted treatment for mitral regurgitation (MR) but lack of resources and socioeconomic concerns delay surgical referral and intervention in developing countries. We evaluated immediate and short-term results of mitral valve repair for non-ischemic MR at our centre and aimed to identify the predictors of in-hospital and follow-up mortality.
Materials and methods
The study was conducted at a tertiary-level hospital in South India. All patients >18 years with severe non-ischemic MR who underwent mitral valve repair over a period of 6 years were included. Perioperative data was collected from hospital records and follow-up data was obtained by prospective methods.
Results
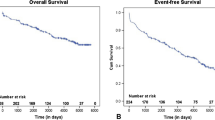
There were 244 patients (170 males). Most of the patients were in the age group 31–60 years (76.6%). Aetiology of MR was degenerative (n = 159; 65.2%), rheumatic (n = 34; 13.9%), structural (n = 42; 17.2%), or miscellaneous (n = 9; 3.7%). All patients underwent ring annuloplasty with various valve repair techniques. One hundred patients (44.7%) underwent additional cardiac procedures. At discharge, MR was moderate in 4 patients; the rest had no or mild MR. The mean hospital stay of survivors was 7.1 days (SD 2.52, range 5–25 days). There were 9 in-hospital deaths (3.68%) and 10 deaths during follow-up (4.2%). The mean follow-up period was 1.39 years, complete for 87.6%. Pre-operative left ventricle ejection fraction (LVEF) <60% (p = 0.04) was found to be significantly associated with immediate mortality. Logistic regression analysis detected age (p = 0.019), female sex (p = 0.015), and left ventricular (LV) dysfunction at discharge (p = 0.025) to be significantly associated with follow-up mortality.
Conclusion
Pre-operative LV dysfunction was identified as a significant risk factor for in-hospital mortality. Female sex, age greater than 45 years, and LV dysfunction at discharge were found to be significantly associated with follow-up mortality. Hence, it is important to perform mitral valve repair in severe regurgitation patients before significant LV dysfunction sets in for a better outcome.
Similar content being viewed by others
References
Howell EJ, Butcher JT. Valvular heart diseases in the developing world: developmental biology takes centre stage. J Heart Valve Dis. 2012;21:234–40.
Chen Y, Yiu K-H. Growing importance of valvular heart disease in the elderly. J Thorac Dis. 2016;8:E1701–E1703.
Moore M, Chen J, Mallow PJ, Rizzo JA. The direct health-care burden of valvular heart disease: evidence from US national survey data. Clinicoecon Outcomes Res. 2016;8:613–27.
Manjunath CN, Srinivas P, Ravindranath KS, Dhanalakshmi C. Incidence and patterns of valvular heart disease in a tertiary care high-volume cardiac center: a single centre experience. Indian Heart J. 2014;66:320–6.
Matiasz R, Rigolin VH. 2017 Focused update for management of patients with valvular heart disease: summary of new recommendations. J Am Heart Assoc. 2018;7:e007596. https://doi.org/10.1161/JAHA.117.007596.
Kumar AS, Talwar S, Saxena A, Singh R, Velayoudam D. Results of mitral valve repair in rheumatic mitral regurgitation. Interact Cardiovasc Thorac Surg. 2006;5:356–61.
Gardner MA, Hossack KF, Smith IR. Long-term results following repair for degenerative mitral regurgitation - analysis of factors influencing durability. Heart Lung Circ. 2019;28:1852–65.
Rey Meyer MA, von Segesser LK, Hurni M, Stumpe F, Eisa K, Ruchat P. Long-term outcome after mitral valve repair: a risk factor analysis. Eur J Cardiothorac Surg. 2007;32:301–7.
Heikkinen J, Biancari F, Satta J, et al. Predicting immediate and late outcome after surgery for mitral valve regurgitation with EuroSCORE. J Heart Valve Dis. 2007;16:116–21.
David TE, Armstrong S, McCrindle BW, Manlhiot C. Late outcomes of mitral valve repair for mitral regurgitation due to degenerative disease. Circulation. 2013;127:1485–92.
Baumgartner H, Falk V, Bax JJ, et al. 2017 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2017;38:2739–91.
Quintana E, Suri RM, Thalji NM, et al. Left ventricular dysfunction after mitral valve repair—the fallacy of “normal” preoperative myocardial function. J Thorac Cardiovasc Surg. 2014;148:2752–62.
Kang D-H, Park S-J, Sun BJ, et al. Early surgery versus conventional treatment for asymptomatic severe mitral regurgitation: a propensity analysis. J Am Coll Cardiol. 2014;63:2398–407.
Zhou T, Li J, Lai H, et al. Benefits of early surgery on clinical outcomes after degenerative mitral valve repair: Ann Thorac Surg. 2018;106:1063–70.
Tribouilloy C, Rusinaru D, Szymanski C, et al. Predicting left ventricular dysfunction after valve repair for mitral regurgitation due to leaflet prolapse: additive value of left ventricular end-systolic dimension to ejection fraction. Eur J Echocardiogr. 2011;12:702–10.
da Rocha ASC, de Novaes da Rocha N, de Cassia Villela Soares R, et al. Improvement in left ventricular dysfunction after surgical correction of mitral regurgitation. Arq Bras Cardiol. 2003. https://doi.org/10.1590/s0066-782x2003000100002.
Suri RM, Schaff HV, Dearani JA. et al. J Recovery of left ventricular function after surgical correction of mitral regurgitation caused by leaflet prolapse. J Thorac Cardiovasc Surg. 2009;137:1071-6.
Witkowski TG, Thomas JD, Delgado V, et al. Changes in left ventricular function after mitral valve repair for severe organic mitral regurgitation. Ann Thorac Surg. 2012;93:754–60.
Shafii AE, Gillinov AM, Mihaljevic T, Stewart W, Batizy LH, Blackstone EH. Changes in left ventricular morphology and function after mitral valve surgery. Am J Cardiol. 2012;110:403-408.e3.
Dupuis M, Mahjoub H, Clavel MA, et al. Forward left ventricular ejection fraction: a simple risk marker in patients with primary mitral regurgitation. J Am Heart Assoc. 2017;6:e006309.
Enriquez-Sarano M, Suri RM, Clavel MA, et al. Is there an outcome penalty linked to guideline- based indications for valvular surgery? Early and long-term analysis of patients with organic mitral regurgitation. J Thorac Cardiovasc Surg. 2015;150:50–58.
Mehta RH, Eagle KA, Coombs LP, et al. Influence of age on outcomes in patients undergoing mitral valve replacement on behalf of the Society of Thoracic Surgeons National Cardiac Registry. Ann Thorac Surg. 2002;74:1459–67.
Song HK, Grab JD, O’Brien SM, Welke KF, Edwards F, Ungerleider RM. Gender differences in mortality after mitral valve operation: evidence for higher mortality in perimenopausal women .Ann Thorac Surg. 2008;85:2040–4.
Acknowledgements
We thank Mr. Arun, Office Assistant, for the help rendered in collecting follow-up data.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Informed consent
The study started after obtaining clearance from the Ethics committee. As this was a retrospective analysis , informed consent was obtained from the patients during follow up echocardiography.
Ethics Committee approval
No. SBMR IRC:03/2016 - Institutional Research Committee, Government Medical College, Kottayam, dated 29/01/2016.
Statement on human and animal rights
The research was conducted in accordance with the ethical standards of the institutional research committee( Kottayam Medical College) on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008(5). No laboratory animals were involved in the study and no intervention involved on humans or animals during the process of conduct of the research.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nair, V.V., Das, S., Nair, R.B. et al. Mitral valve repair in chronic severe mitral regurgitation: short-term results and analysis of mortality predictors. Indian J Thorac Cardiovasc Surg 37, 506–513 (2021). https://doi.org/10.1007/s12055-021-01160-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-021-01160-x