Abstract
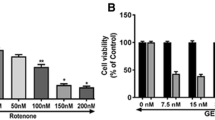
Parkinson’s disease (PD) is the second most common multifactorial neurodegenerative disorder caused by several genetics and environmental factors. Rotenone a pesticide with mitotoxicity causes cytosolic proteopathy resulting in PD-associated apoptosis and modulations in cell survival pathways. Shikonin, a naphthoquinone compound extracted from the Lithospermum erythrorhizon herb, was investigated in this study for its neuroprotective properties and underlying molecular mechanisms against rotenone-induced cellular apoptosis and survival in SH-SY5Y cells. The molecular docking analysis of apoptotic proteins against Shikonin revealed that they showed a binding affinity with BAD. Shikonin effectively countered the loss of cell viability induced by rotenone, rescued annexin-positive apoptotic cells, and dose-dependently suppressed the generation of reactive oxygen species. Pre-treatment with Shikonin prevented the morphological aberrations like shrining of neurites leading to decreased LDH leakage and NO release caused due to the rotenone treatment. The α-synucleinopathy is a prime hallmark of PD, Shikonin mitigated the rotenone-induced aggregation of α-synuclein as seen from confocal imaging. Furthermore, Shikonin treatment reversed the rotenone-induced excessive production of reactive oxygen species, activation of caspases (-8 and -3), and mitochondrial dysfunction, as evidenced by the restoration of mitochondrial membrane potential and cellular ATP levels. Western blot and qPCR analysis revealed that Shikonin heightened the IGF1R/PI3K/AKT signaling associated with cell survival while concurrently downregulating rotenone-induced intrinsic apoptotic pathways. These findings underscore Shikonin as a promising candidate to prevent the onset of pesticide-induced Parkinson’s disease and potentially other oxidative stress-related neurodegenerative disorders.















Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.Data Availability
No datasets were generated or analysed during the current study.
References
Ahuja M, Kaidery NA, Dutta D, Attucks OC, Kazakov EH, Gazaryan I, Matsumoto M, Igarashi K, Sharma SM, Thomas B (2022) Harnessing the therapeutic potential of the Nrf2/Bach1 signaling pathway in Parkinson’s disease. Antioxidants 11(9):1780. https://doi.org/10.3390/antiox11091780
Antonsson B, Montessuit S, Sanchez B, Martinou J-C (2001) Bax is present as a high molecular weight oligomer/complex in the mitochondrial membrane of apoptotic cells. J Biol Chem 276(15):11615–11623. https://doi.org/10.1074/jbc.M010810200
Barzilai A, Melamed E (2003) Molecular mechanisms of selective dopaminergic neuronal death in Parkinson’s disease. Trends Mol Med 9(3):126–132. https://doi.org/10.1016/S1471-4914(03)00020-0
Ben-Shlomo Y, Darweesh S, Llibre-Guerra J, Marras C, Luciano MS, Tanner C (2024) The epidemiology of Parkinson’s disease. The Lancet 403(10423):283–292. https://doi.org/10.1016/S0140-6736(23)01419-8
Egilmez CB, Pazarlar BA, Erdogan MA, Erbas O (2024) Neuroprotective effect of dexpanthenol on rotenone-induced Parkinson’s disease model in rats. Neurosci Lett 818(January):137575. https://doi.org/10.1016/j.neulet.2023.137575
Brunelle JK, Letai A (2009) Control of mitochondrial apoptosis by the Bcl-2 family. J Cell Sci 122(4):437–441. https://doi.org/10.1242/jcs.031682
Denault J-B, Salvesen GS (2002) Caspases: keys in the ignition of cell death. Chem Rev 102(12):4489–4500. https://doi.org/10.1021/cr010183n
Dhanalakshmi C, Manivasagam T, Nataraj J, Thenmozhi AJ, Essa MM (2015) Neurosupportive role of vanillin, a natural phenolic compound, on rotenone induced neurotoxicity in SH-SY5Y neuroblastoma cells. Evid Based Complementary Altern Med 2015:1–11. https://doi.org/10.1155/2015/626028
Dionísio PA, Amaral JD, Rodrigues CMP (2021) Oxidative stress and regulated cell death in Parkinson’s disease. Ageing Res Rev 67(May):101263. https://doi.org/10.1016/j.arr.2021.101263
Dorsey ER, Bloem BR (2024) Parkinson’s disease is predominantly an environmental disease. J Parkinson’s Dis, January, 1–15.https://doi.org/10.3233/JPD-230357
Farahani MS, Bahramsoltani R, Farzaei MH, Abdollahi M, Rahimi R (2015) Plant-derived natural medicines for the management of depression: an overview of mechanisms of action. Rev Neurosci 26(3). https://doi.org/10.1515/revneuro-2014-0058
Guo L, Li Y, Li W, Qiu J, Juan Du, Wang L, Zhang T (2022) Shikonin ameliorates oxidative stress and neuroinflammation via the Akt/ <scp>ERK</Scp> / <scp>JNK</Scp> / <scp>NF-κB</Scp> signalling pathways in a model of Parkinson’s disease. Clin Exp Pharmacol Physiol 49(11):1221–1231. https://doi.org/10.1111/1440-1681.13709
Hao X-M, Li L-D, Duan C-L, Li Y-J (2017) Neuroprotective effect of α-mangostin on mitochondrial dysfunction and α-synuclein aggregation in rotenone-induced model of Parkinson’s disease in differentiated SH-SY5Y cells. J Asian Nat Prod Res 19(8):833–845. https://doi.org/10.1080/10286020.2017.1339349
Ibarra-Gutiérrez MT, Serrano-García N, Orozco-Ibarra M (2023) Rotenone-induced model of Parkinson’s disease: beyond mitochondrial complex I inhibition. Mol Neurobiol 60(4):1929–1948. https://doi.org/10.1007/s12035-022-03193-8
Jiang M, Qi L, Li L, Li Y (2020) The caspase-3/GSDME signal pathway as a switch between apoptosis and pyroptosis in cancer. Cell Death Discovery 6(1):112. https://doi.org/10.1038/s41420-020-00349-0
Jiang X, Wang X (2004) Cytochrome C -mediated apoptosis. Annu Rev Biochem 73(1):87–106. https://doi.org/10.1146/annurev.biochem.73.011303.073706
Ju D-T, Sivalingam K, Kuo W-W, Ho T-J, Chang R-L, Chung L-C, Day CH, Viswanadha VP, Liao P-H, Huang C-Y (2019) Effect of vasicinone against paraquat-induced MAPK/P53-mediated apoptosis via the IGF-1R/PI3K/AKT pathway in a Parkinson’s disease-associated SH-SY5Y cell model. Nutrients 11(7):1655. https://doi.org/10.3390/nu11071655
Kandil EA, Abdelkader NF, El-Sayeh BM, Saleh S (2016) Imipramine and amitriptyline ameliorate the rotenone model of Parkinson’s disease in rats. Neuroscience 332(September):26–37. https://doi.org/10.1016/j.neuroscience.2016.06.040
Kavitha M, Manivasagam T, Essa MM, Tamilselvam K, Selvakumar GP, Karthikeyan S, Thenmozhi JA, Subash S (2014) Mangiferin antagonizes rotenone: induced apoptosis through attenuating mitochondrial dysfunction and oxidative stress in SK-N-SH neuroblastoma cells. Neurochem Res 39(4):668–676. https://doi.org/10.1007/s11064-014-1249-7
Kourounakis AP, Assimopoulou AN, Papageorgiou VP, Gavalas A, Kourounakis PN (2002) Alkannin and Shikonin: effect on free radical processes and on inflammation - a preliminary pharmacochemical investigation. Arch Pharm 335(6):262. https://doi.org/10.1002/1521-4184(200208)335:6%3c262::AID-ARDP262%3e3.0.CO;2-Y
Krishna A, Biryukov M, Trefois C, Antony PMA, Hussong R, Lin J, Heinäniemi M et al (2014) Systems genomics evaluation of the SH-SY5Y neuroblastoma cell line as a model for Parkinson’s disease. BMC Genomics 15(1):1154. https://doi.org/10.1186/1471-2164-15-1154
Lawana V, Cannon JR (2020) Rotenone neurotoxicity: relevance to Parkinson’s disease. In: 209–54. https://doi.org/10.1016/bs.ant.2019.11.004
LeBel CP, Ischiropoulos H, Bondy SC (1992) Evaluation of the probe 2’,7’-dichlorofluorescin as an indicator of reactive oxygen species formation and oxidative stress. Chem Res Toxicol 5(2):227–231. https://doi.org/10.1021/tx00026a012
Lemasters JJ (2005) Selective mitochondrial autophagy, or mitophagy, as a targeted defense against oxidative stress, mitochondrial dysfunction, and aging. Rejuvenation Res 8(1):3–5. https://doi.org/10.1089/rej.2005.8.3
Lu L, Tang LE, Wei W, Hong Y, Chen H, Ying W, Chen S (2014) Nicotinamide mononucleotide improves energy activity and survival rate in an in vitro model of Parkinson’s disease. Exp Ther Med 8(3):943–950. https://doi.org/10.3892/etm.2014.1842
Mogi M, Togari A, Kondo T, Mizuno Y, Komure O, Kuno S, Ichinose H, Nagatsu T (2000) Caspase activities and tumor necrosis factor receptor R1 (P55) level are elevated in the substantia nigra from parkinsonian brain. J Neural Transm 107(3):335–341. https://doi.org/10.1007/s007020050028
Morén C, Mary R, deSouza D, Giraldo M, Uff C (2022) Antioxidant therapeutic strategies in neurodegenerative diseases. Int J Mol Sci 23(16):9328. https://doi.org/10.3390/ijms23169328
Morris HR, Spillantini MG, Sue CM, Williams-Gray CH (2024) The pathogenesis of Parkinson’s disease. The Lancet 403(10423):293–304. https://doi.org/10.1016/S0140-6736(23)01478-2
Mosmann T (1983) Rapid colorimetric assay for cellular growth and survival: application to proliferation and cytotoxicity assays. J Immunol Methods 65(1–2):55–63. https://doi.org/10.1016/0022-1759(83)90303-4
Nandipati S, Litvan I (2016) Environmental exposures and Parkinson’s disease. Int J Environ Res Public Health 13(9):881. https://doi.org/10.3390/ijerph13090881
Ojha S, Javed H, Azimullah S, Abul Khair SB, Haque ME (2016) Glycyrrhizic acid attenuates neuroinflammation and oxidative stress in rotenone model of Parkinson’s disease. Neurotox Res 29(2):275–287. https://doi.org/10.1007/s12640-015-9579-z
Ojha S, Javed H, Azimullah S, Haque ME (2016) β-Caryophyllene, a phytocannabinoid attenuates oxidative stress, neuroinflammation, glial activation, and salvages dopaminergic neurons in a rat model of Parkinson disease. Mol Cell Biochem 418(1–2):59–70. https://doi.org/10.1007/s11010-016-2733-y
Priya LB, Baskaran R, Huang C-Y, Padma VV (2017) Neferine ameliorates cardiomyoblast apoptosis induced by doxorubicin: possible role in modulating NADPH oxidase/ROS-mediated NFκB redox signaling cascade. Sci Rep 7(1):12283. https://doi.org/10.1038/s41598-017-12060-9
Priyadarshi R, Rhim J-W (2022) Shikonin: extraction, properties and applications in active and intelligent packaging. Packag Technol Sci 35(12):863–877. https://doi.org/10.1002/pts.2687
Ramalingam M, Huh YJ, Lee YI (2019) The impairments of α-synuclein and mechanistic target of rapamycin in rotenone-induced SH-SY5Y cells and mice model of Parkinson’s disease. Front Neurosci 13(September). https://doi.org/10.3389/fnins.2019.01028
Ratan Y, Rajput A, Pareek A, Pareek A, Jain V, Sonia S, Farooqui Z, Kaur R, Singh G (2024) Advancements in genetic and biochemical insights: unraveling the etiopathogenesis of neurodegeneration in Parkinson’s disease. Biomolecules 14(1):73. https://doi.org/10.3390/biom14010073
Reed JC (2000) Mechanisms of apoptosis. Am J Pathol 157(5):1415–1430. https://doi.org/10.1016/S0002-9440(10)64779-7
Roy T, Chatterjee A, Swarnakar S (2023) Rotenone induced neurodegeneration is mediated via cytoskeleton degradation and necroptosis. Biochimica et Biophysica Acta (BBA) - Mol Cell Res 1870(3):119417. https://doi.org/10.1016/j.bbamcr.2022.119417
Shahpiri Z, Bahramsoltani R, Farzaei MH, Farzaei F, Rahimi R (2016) Phytochemicals as future drugs for Parkinson’s disease: a comprehensive review. Rev Neurosci 27(6):651–668. https://doi.org/10.1515/revneuro-2016-0004
Sherer TB, Betarbet R, Kim J-H, Timothy Greenamyre J (2003) Selective microglial activation in the rat rotenone model of Parkinson’s disease. Neurosci Lett 341(2):87–90. https://doi.org/10.1016/S0304-3940(03)00172-1
Sherer TB, Betarbet R, Testa CM, Seo BB, Richardson JR, Kim JH, Miller GW, Yagi T, Matsuno-Yagi A, Timothy Greenamyre J (2003) Mechanism of toxicity in rotenone models of Parkinson’s disease. J Neurosci 23(34):10756–10764. https://doi.org/10.1523/JNEUROSCI.23-34-10756.2003
Sherer TB, Kim J-H, Betarbet R, Timothy Greenamyre J (2003) Subcutaneous rotenone exposure causes highly selective dopaminergic degeneration and α-synuclein aggregation. Exp Neurol 179(1):9–16. https://doi.org/10.1006/exnr.2002.8072
Simon DK, Tanner CM, Brundin P (2020) Parkinson disease epidemiology, pathology, genetics, and pathophysiology. Clin Geriatr Med 36(1):1–12. https://doi.org/10.1016/j.cger.2019.08.002
Thakur P, Nehru B (2015) Inhibition of neuroinflammation and mitochondrial dysfunctions by carbenoxolone in the rotenone model of Parkinson’s disease. Mol Neurobiol 51(1):209–219. https://doi.org/10.1007/s12035-014-8769-7
Tong Y, Bai L, Gong R, Chuan J, Duan X, Zhu Y (2018) Shikonin protects PC12 cells against β-amyloid peptide-induced cell injury through antioxidant and antiapoptotic activities. Sci Rep 8(1):26. https://doi.org/10.1038/s41598-017-18058-7
Tuo Hu, Li W, Zhao W, Zhao J, Li D, Jin L (2024) Shikonin alleviates doxorubicin-induced cardiotoxicity via Mst1/Nrf2 pathway in mice. Sci Rep 14(1):924. https://doi.org/10.1038/s41598-024-51675-7
Xiong N, Jia M, Chen C, Xiong J, Zhang Z, Huang J, Hou L et al (2011) Potential autophagy enhancers attenuate rotenone-induced toxicity in SH-SY5Y. Neuroscience 199(December):292–302. https://doi.org/10.1016/j.neuroscience.2011.10.031
Yang E, Zha J, Jockel J, Boise LH, Thompson CB, Korsmeyer SJ (1995) Bad, a heterodimeric partner for Bcl-XL and Bcl-2, displaces Bax and promotes cell death. Cell 80(2):285–291. https://doi.org/10.1016/0092-8674(95)90411-5
Yang H, Masters SC, Wang H, Fu H (2001) The proapoptotic protein bad binds the amphipathic groove of 14–3–3ζ. Biochimica et Biophysica Acta (BBA) - Protein Struct Mol Enzymol 1547(2):313–19. https://doi.org/10.1016/S0167-4838(01)00202-3
Zhang N, Yan Z, Xin H, Shao S, Xue S, Cespuglio R, Wang S (2023) Relationship among Α-synuclein, aging and inflammation in Parkinson’s disease (Review). Exp Ther Med 27(1):23. https://doi.org/10.3892/etm.2023.12311
Zhang Yu, Guo H, Guo X, Ge D, Shi Y, Xiyu Lu, Jinli Lu, Chen J, Ding F, Zhang Qi (2019) Involvement of Akt/MTOR in the neurotoxicity of rotenone-induced Parkinson’s disease models. Int J Environ Res Public Health 16(20):3811. https://doi.org/10.3390/ijerph16203811
Zhong J, Wang Z, Xie Q, Li T, Chen K, Zhu T, Tang Q, Shen C, Zhu J (2020) Shikonin ameliorates D-galactose-induced oxidative stress and cognitive impairment in mice via the MAPK and nuclear factor-ΚB signaling pathway. Int Immunopharmacol 83(June):106491. https://doi.org/10.1016/j.intimp.2020.106491
Zhong Yu, Qi Ao, Liu L, Huang Q, Zhang J, Cai K, Cai C (2021) Shikonin attenuates H 2 O 2 -induced oxidative injury in HT29 cells via antioxidant activities and the inhibition of mitochondrial pathway-mediated apoptosis. Exp Ther Med 22(4):1118. https://doi.org/10.3892/etm.2021.10552
Acknowledgements
Aparna Anandan sincerely acknowledges the Department of Science and Technology for providing financial support through INSPIRE programme (DST/INSPIRE Fellowship/2019/IF190185). Surovi Saika thank UGC-New Delhi for Dr. D S Kothari Fellowship (no. F-2/2006 [BSR]/BL/20-21/0396). Vijaya Padma Viswanadha acknowledges Tamil Nadu State Council for Higher Education-RGP (RGP/2019-20/BU/HECP-0005] no. C3/CRTD/ 995/ 2021) for equipment and travel support. The authors sincerely acknowledge DST-FIST and DST-SERB funding agencies for providing equipment.
Funding
This work is supported by Tamil Nadu State Council for Higher Education-RGP (RGP/2019–20/BU/HECP-0005] no. C3/CRTD/995/2021). Aparna Anandan and Surovi Saika received financial support fellowship from the Department of Science and Technology for providing financial support through INSPIRE programme (DST/INSPIRE Fellowship/2019/IF190185) and UGC-New Delhi for Dr. D S Kothari Fellowship (no. F-2/2006 [BSR]/BL/20–21/0396), respectively.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Primary Conceptualisation and guidance done by Dr. Vijaya Padma Viswanadha. Material preparation, data collection, execution and analysis were performed by Aparna Anandan. Mohammed Unais AK helped to execute the work. Dr. Surovi Saika executed the in-silico part in the work. The first draft of the manuscript was written by Aparna Anandan, revised by Dr. Marthandam Asokan Shibu and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Consent to Participate
No human subjects were involved in the study, and no consent is required.
Consent for Publication
No human subjects were involved in the study, and no consent is required.
Ethics Approval
No. As this is the in vitro work, no ethical approval is required. SH-SY5Y cells of P26 batch were procured from the National Centre for Cell Sciences, Pune cell repository.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Anandan, A., AK, M.U., Saika, S. et al. Shikonin Ameliorates Rotenone-Induced Neurotoxicity Through Inhibition of Apoptosis via IGF-1R/PI3K/AKT Pathway in a Parkinson’s Disease-Associated SH-SY5Y Cell Model. Mol Neurobiol (2025). https://doi.org/10.1007/s12035-025-04810-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12035-025-04810-y