Abstract
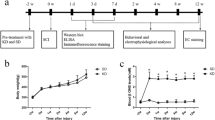
Sodium butyrate (SB) is a dietary microbial fermentation product and serves as an important neuromodulator in the central nervous system. Recent experimental evidence has suggested potential therapeutic applications for butyrate, including its utility in treating metabolic and inflammatory diseases. The aim of the present study was to evaluate the potential beneficial effects of SB in a mouse model of spinal cord injury (SCI) and its possible mechanism of action. SCI was induced by extradural compression for 1 min of the spinal cord at the T6–7 level using an aneurysm clip, and SB (10–30-100 mg/kg) was administered by oral gavage 1 and 6 h after SCI. For locomotor activity, study mice were treated with SB once daily for 10 days. Morphological examination was performed by light microscopy through hematoxylin-eosin (H&E) staining. In addition, NF-κB, IκB-α, COX-2, and iNOS expressions were assayed by western blot analysis and IL-1β and TNF-α levels by immunohistochemistry analysis. The results showed that SB treatment significantly ameliorated histopathology changes and improved recovery of motor function changes in spinal cord injury in a dose-dependent manner. Moreover, we demonstrated that SB modulated the NF-κB pathway showing a significant reduction in cytokine expression. Thus, this study showed that SB exerts neuroprotective effects anti-inflammatory properties following spinal cord injury suggesting that SB may serve as a potential candidate for future treatment of spinal cord injury.






Similar content being viewed by others
References
Zhang N, Fang M, Chen H, Gou F, Ding M (2014) Evaluation of spinal cord injury animal models. Neural Regen Res 9(22):2008–2012. https://doi.org/10.4103/1673-5374.143436
Chuang DM, Leng Y, Marinova Z, Kim HJ, Chiu CT (2009) Multiple roles of HDAC inhibition in neurodegenerative conditions. Trends Neurosci 32(11):591–601. https://doi.org/10.1016/j.tins.2009.06.002
Scheppach W (1994) Effects of short chain fatty acids on gut morphology and function. Gut 35(1 Suppl):S35–S38
Machado RA, Constantino Lde S, Tomasi CD, Rojas HA, Vuolo FS, Vitto MF, Cesconetto PA, de Souza CT et al Sodium butyrate decreases the activation of NF-kappaB reducing inflammation and oxidative damage in the kidney of rats subjected to contrast-induced nephropathy. Nephrol Dial Transplant 27(8):3136–3140. https://doi.org/10.1093/ndt/gfr807
Arpaia N, Campbell C, Fan X, Dikiy S, van der Veeken J, de Roos P, Liu H, Cross JR et al Metabolites produced by commensal bacteria promote peripheral regulatory T-cell generation. Nature 504(7480):451–455. https://doi.org/10.1038/nature12726
Smith PM, Howitt MR, Panikov N, Michaud M, Gallini CA, Bohlooly YM, Glickman JN, Garrett WS The microbial metabolites, short-chain fatty acids, regulate colonic Treg cell homeostasis. Science 341(6145):569–573. https://doi.org/10.1126/science.1241165
Sun J, Chang EB Exploring gut microbes in human health and disease: pushing the envelope. Genes Dis 1(2):132–139. https://doi.org/10.1016/j.gendis.2014.08.001
Canani RB, Costanzo MD, Leone L, Pedata M, Meli R, Calignano A Potential beneficial effects of butyrate in intestinal and extraintestinal diseases. World J Gastroenterol 17(12):1519–1528. https://doi.org/10.3748/wjg.v17.i12
Guilloteau P, Martin L, Eeckhaut V, Ducatelle R, Zabielski R, Van Immerseel F From the gut to the peripheral tissues: the multiple effects of butyrate. Nutr Res Rev 23(2):366–384. https://doi.org/10.1017/S0954422410000247
Yaku K, Enami Y, Kurajyo C, Matsui-Yuasa I, Konishi Y, Kojima-Yuasa A (2012) The enhancement of phase 2 enzyme activities by sodium butyrate in normal intestinal epithelial cells is associated with Nrf2 and p53. Mol Cell Biochem 370(1–2):7–14. https://doi.org/10.1007/s11010-012-1392-x
Vernia P, Marcheggiano A, Caprilli R, Frieri G, Corrao G, Valpiani D, Di Paolo MC, Paoluzi P et al (1995) Short-chain fatty acid topical treatment in distal ulcerative colitis. Aliment Pharmacol Ther 9(3):309–313
Steinhart AH, Brzezinski A, Baker JP (1994) Treatment of refractory ulcerative proctosigmoiditis with butyrate enemas. Am J Gastroenterol 89(2):179–183
Patz J, Jacobsohn WZ, Gottschalk-Sabag S, Zeides S, Braverman DZ (1996) Treatment of refractory distal ulcerative colitis with short chain fatty acid enemas. Am J Gastroenterol 91(4):731–734
Pinto A, Fidalgo P, Cravo M, Midoes J, Chaves P, Rosa J, dos Anjos Brito M, Leitao CN (1999) Short chain fatty acids are effective in short-term treatment of chronic radiation proctitis: randomized, double-blind, controlled trial. Dis Colon Rectum 42(6):788–795 discussion 795-786
Kukkar A, Singh N, Jaggi AS Attenuation of neuropathic pain by sodium butyrate in an experimental model of chronic constriction injury in rats. J Formos Med Assoc 113(12):921–928. https://doi.org/10.1016/j.jfma.2013.05.013
Russo R, De Caro C, Avagliano C, Cristiano C, La Rana G, Mattace Raso G, Berni Canani R, Meli R et al Sodium butyrate and its synthetic amide derivative modulate nociceptive behaviors in mice. Pharmacol Res 103:279–291. https://doi.org/10.1016/j.phrs.2015.11.026
Basso DM, Fisher LC, Anderson AJ, Jakeman LB, McTigue DM, Popovich PG (2006) Basso mouse scale for locomotion detects differences in recovery after spinal cord injury in five common mouse strains. J Neurotrauma 23(5):635–659. https://doi.org/10.1089/neu.2006.23.635
Lang-Lazdunski L, Blondeau N, Jarretou G, Lazdunski M, Heurteaux C (2003) Linolenic acid prevents neuronal cell death and paraplegia after transient spinal cord ischemia in rats. J Vasc Surg 38(3):564–575
Ferre N, Marsillach J, Camps J, Mackness B, Mackness M, Riu F, Coll B, Tous M et al (2006) Paraoxonase-1 is associated with oxidative stress, fibrosis and FAS expression in chronic liver diseases. J Hepatol 45(1):51–59. https://doi.org/10.1016/j.jhep.2005.12.018
Hernandez-Aguilera A, Sepulveda J, Rodriguez-Gallego E, Guirro M, Garcia-Heredia A, Cabre N, Luciano-Mateo F, Fort-Gallifa I et al (2015) Immunohistochemical analysis of paraoxonases and chemokines in arteries of patients with peripheral artery disease. Int J Mol Sci 16(5):11323–11338. https://doi.org/10.3390/ijms160511323
Rodriguez-Sanabria F, Rull A, Beltran-Debon R, Aragones G, Camps J, Mackness B, Mackness M, Joven J (2010) Tissue distribution and expression of paraoxonases and chemokines in mouse: the ubiquitous and joint localisation suggest a systemic and coordinated role. J Mol Histol 41(6):379–386. https://doi.org/10.1007/s10735-010-9299-x
Visavadiya NP, Patel SP, VanRooyen JL, Sullivan PG, Rabchevsky AG (2016) Cellular and subcellular oxidative stress parameters following severe spinal cord injury. Redox Biol 8:59–67. https://doi.org/10.1016/j.redox.2015.12.011
Cogswell JP, Godlevski MM, Wisely GB, Clay WC, Leesnitzer LM, Ways JP, Gray JG (1994) NF-kappa B regulates IL-1 beta transcription through a consensus NF-kappa B binding site and a nonconsensus CRE-like site. J Immunol 153(2):712–723
Herman PE, Papatheodorou A, Bryant SA, Waterbury CKM, Herdy JR, Arcese AA, Buxbaum JD, Smith JJ et al Highly conserved molecular pathways, including Wnt signaling, promote functional recovery from spinal cord injury in lampreys. Sci Rep 8(1):742. https://doi.org/10.1038/s41598-017-18757-1
Carlson SL, Parrish ME, Springer JE, Doty K, Dossett L (1998) Acute inflammatory response in spinal cord following impact injury. Exp Neurol 151(1):77–88. https://doi.org/10.1006/exnr.1998.6785
Mautes AE, Weinzierl MR, Donovan F, Noble LJ (2000) Vascular events after spinal cord injury: contribution to secondary pathogenesis. Phys Ther 80(7):673–687
Popovich PG, Wei P, Stokes BT (1997) Cellular inflammatory response after spinal cord injury in Sprague-Dawley and Lewis rats. J Comp Neurol 377(3):443–464. https://doi.org/10.1002/(SICI)1096-9861(19970120)377:3<443::AID-CNE10>3.0.CO;2-S
Resnick DK, Nguyen P, Cechvala CF (2001) Regional and temporal changes in prostaglandin E2 and thromboxane B2 concentrations after spinal cord injury. Spine J 1(6):432–436
Streit WJ, Semple-Rowland SL, Hurley SD, Miller RC, Popovich PG, Stokes BT (1998) Cytokine mRNA profiles in contused spinal cord and axotomized facial nucleus suggest a beneficial role for inflammation and gliosis. Exp Neurol 152(1):74–87. https://doi.org/10.1006/exnr.1998.6835
Tonai T, Taketani Y, Ueda N, Nishisho T, Ohmoto Y, Sakata Y, Muraguchi M, Wada K et al (1999) Possible involvement of interleukin-1 in cyclooxygenase-2 induction after spinal cord injury in rats. J Neurochem 72(1):302–309
Wang CX, Olschowka JA, Wrathall JR (1997) Increase of interleukin-1beta mRNA and protein in the spinal cord following experimental traumatic injury in the rat. Brain Res 759(2):190–196
Xu J, Fan G, Chen S, Wu Y, Xu XM, Hsu CY (1998) Methylprednisolone inhibition of TNF-alpha expression and NF-kB activation after spinal cord injury in rats. Brain Res Mol Brain Res 59(2):135–142
Dusart I, Schwab ME (1994) Secondary cell death and the inflammatory reaction after dorsal hemisection of the rat spinal cord. Eur J Neurosci 6(5):712–724
Pineau I, Sun L, Bastien D, Lacroix S Astrocytes initiate inflammation in the injured mouse spinal cord by promoting the entry of neutrophils and inflammatory monocytes in an IL-1 receptor/MyD88-dependent fashion. Brain Behav Immun 24(4):540–553. https://doi.org/10.1016/j.bbi.2009.11.007
Beck KD, Nguyen HX, Galvan MD, Salazar DL, Woodruff TM, Anderson AJ Quantitative analysis of cellular inflammation after traumatic spinal cord injury: evidence for a multiphasic inflammatory response in the acute to chronic environment. Brain 133(Pt 2):433–447. https://doi.org/10.1093/brain/awp322
Brennan FH, Popovich PG Emerging targets for reprograming the immune response to promote repair and recovery of function after spinal cord injury. Curr Opin Neurol 31(3):334–344. https://doi.org/10.1097/WCO.0000000000000550
Barnes PJ, Karin M (1997) Nuclear factor-kappaB: a pivotal transcription factor in chronic inflammatory diseases. N Engl J Med 336(15):1066–1071. https://doi.org/10.1056/NEJM199704103361506
Liu T, Zhang L, Joo D, Sun SC. NF-kappaB signaling in inflammation. Signal Transduct Target Ther 2. https://doi.org/10.1038/sigtrans.2017.23
Wang L, Yu WB, Tao LY, Xu Q Myeloid-derived suppressor cells mediate immune suppression in spinal cord injury. J Neuroimmunol 290:96–102. https://doi.org/10.1016/j.jneuroim.2015.11.023
Lago N, Pannunzio B, Amo-Aparicio J, Lopez-Vales R, Peluffo H (2018) CD200 modulates spinal cord injury neuroinflammation and outcome through CD200R1. Brain Behav Immun. https://doi.org/10.1016/j.bbi.2018.06.002
Park JS, Woo MS, Kim SY, Kim WK, Kim HS (2005) Repression of interferon-gamma-induced inducible nitric oxide synthase (iNOS) gene expression in microglia by sodium butyrate is mediated through specific inhibition of ERK signaling pathways. J Neuroimmunol 168(1–2):56–64. https://doi.org/10.1016/j.jneuroim.2005.07.003
Appleton I, Tomlinson A, Willoughby DA (1996) Induction of cyclo-oxygenase and nitric oxide synthase in inflammation. Adv Pharmacol 35:27–78
Resnick DK, Graham SH, Dixon CE, Marion DW (1998) Role of cyclooxygenase 2 in acute spinal cord injury. J Neurotrauma 15(12):1005–1013. https://doi.org/10.1089/neu.1998.15.1005
Narita M, Shimamura M, Imai S, Kubota C, Yajima Y, Takagi T, Shiokawa M, Inoue T et al (2008) Role of interleukin-1beta and tumor necrosis factor-alpha-dependent expression of cyclooxygenase-2 mRNA in thermal hyperalgesia induced by chronic inflammation in mice. Neuroscience 152(2):477–486. https://doi.org/10.1016/j.neuroscience.2007.10.039
Pool-Zobel B, Veeriah S, Bohmer FD (2005) Modulation of xenobiotic metabolising enzymes by anticarcinogens -- focus on glutathione S-transferases and their role as targets of dietary chemoprevention in colorectal carcinogenesis. Mutat Res 591(1–2):74–92. https://doi.org/10.1016/j.mrfmmm.2005.04.020
Acknowledgments
The authors would like to thank Antonietta Medici for the excellent technical assistance during this study and Miss Valentina Malvagni for the editorial assistance with the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
The authors declare that they do not have any conflicts of interest.
Rights and permissions
About this article
Cite this article
Lanza, M., Campolo, M., Casili, G. et al. Sodium Butyrate Exerts Neuroprotective Effects in Spinal Cord Injury. Mol Neurobiol 56, 3937–3947 (2019). https://doi.org/10.1007/s12035-018-1347-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-018-1347-7