Abstract
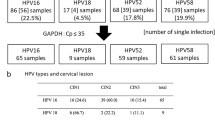
Integration of the HPV genome into a host cell DNA leads to the deregulated overexpression of the viral E6 and E7 oncoproteins, and this is a key factor for progression from low-grade cervical lesions to high-grade lesions and invasive cervical cancer. The aim of our study was to analyze the expression levels of HPV E6*I/E6*II and E7 genes in cervical neoplasia of different grades. The analysis involved 10 low-grade squamous intraepithelial lesions (CIN1), 15 high-grade lesions (CIN2 and CIN3), as well as normal cytology samples (n = 10). HPV genotyping was done using RealLine HPV 16/18 kit. The expression analysis was performed in real-time PCR assay using gene-specific primers and SYBR Green. HPV16 DNA was found in 65.71 % patients, including also normal cytology samples. The increased expression level of E6*I was observed in 12 (34.3 %) patients. The expression of E6*II was increased in 10 (28.6 %) samples, and E7 overexpression was found in 14 (40 %) patients. Significant positive correlation was observed between the amount of HPV16 DNA and the levels of E6*I and E6*II expression. There were no statistically significant differences in expression levels of the studied genes between the groups (CIN1 vs. CIN2/CIN3 vs. normal cytology). Statistically significant differences were found in CIN2/CIN3 group, with the higher expression of E6*II as compared with E6*I. We suggest that the expression level of E6*II gene might be used as an indicator of cervical cancer severity, in patients with high-grade cervical neoplasia, but these observations need to be confirmed in a larger patient cohort.
Similar content being viewed by others
References
Castellsagué X, Bruni L, Brotons M, Barrionuevo L, Serrano B, Muñoz J, Bosch FX, de Sanjosé S. ICO information centre on HPV and cervical cancer (HPV information centre). Human papillomavirus and related diseases in Poland. PREHDICT edition. Summary Report 2013. http://www.hpvcentre.net/statistics/reports/POL.pdf.
Bosch FX, Lorincz A, Muñoz N, Meijer CJ, Shah KV. The causal relation between human papillomavirus and cervical cancer. J Clin Pathol. 2002;55:244–65.
Muñoz N, Bosch FX, de Sanjosé S, Herrero R, Castellsagué X, Shah KV, Snijders PJ, Meijer CJ. International Agency for Research on Cancer Multicenter Cervical Cancer Study Group. Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med. 2003;348:518–27.
Clifford G, Franceschi S, Diaz M, Muñoz N, Villa LL. Chapter 3: HPV type-distribution in women with and without cervical neoplastic diseases. Vaccine. 2006;24:26–34.
zur Hausen H. Papillomaviruses causing cancer: evasion from host-cell control in early events in carcinogenesis. J Natl Cancer Inst. 2000;92:690–8.
Syrjänen KJ. Epidemiology of human papillomavirus (HPV) infections and their associations with genital squamous cell cancer: review article. APMIS. 1989;97:957–70.
Khan MJ, Castle PE, Lorincz AT, Wacholder S, Sherman M, Scott DR, Rush BB, Glass AG, Schiffman M. The elevated 10-year risk of cervical precancer and cancer in women with human papillomavirus (HPV) type 16 or 18 and the possible utility of type-specific HPV testing in clinical practice. J Natl Cancer Inst. 2005;97:1072–9.
Trottier H, Mahmud SM, Lindsay L, Jenkins D, Quint W, Wieting SL, Schuind A, Franco EL, GSK HPV-001 Vaccine Study Group. Persistence of an incident human papillomavirus infection and timing of cervical lesions in previously unexposed young women. Cancer Epidemiol Biomarkers Prev. 2009. doi: 10.1158/1055-9965.EPI-08-1012.
Winer RL, Kiviat NB, Hughes JP, Adam DE, Lee SK, Kuypers JM, Koutsky LA. Development and duration of human papillomavirus lesions, after initial infection. J Infect Dis. 2005;191:731–8.
Kjær SK, Frederiksen K, Munk C, Iftner T. Long-term absolute risk of cervical intraepithelial neoplasia grade 3 or worse following human papillomavirus infection: role of persistence. J Natl Cancer Inst. 2010. doi: 10.1093/jnci/djq356.
Cattani P, Zannoni GF, Ricci C, D’Onghia S, Trivellizzi IN, Di Franco A, Vellone VG, Durante M, Fadda G, Scambia G, Capelli G, De Vincenzo R. Clinical performance of human papillomavirus E6 and E7 mRNA testing for high-grade lesions of the cervix. J Clin Microbiol. 2009. doi: 10.1128/JCM.01275-09.
Lukic A, Sbenaglia G, Carico E, DI Properzio M, Giarnieri E, Frega A, Nobili F, Moscarini M, Giovagnoli MR. Prediction of clinical outcome using p16INK4a immunocytochemical expression in low-grade squamous intraepithelial lesions and high-risk HPV-positive atypical squamous cells of undetermined significance in patients with and without colposcopic evident cervical disease. Exp Ther Med. 2011;2:853–8.
DiPaolo JA, Popescu NC, Alvarez L, Woodworth CD. Cellular and molecular alterations in human epithelial cells transformed by recombinant human papillomavirus DNA. Crit Rev Oncog. 1993;4:337–60.
Hu G, Liu W, Hanania EG, Fu S, Wang T, Deisseroth AB. Suppression of tumorigenesis by transcription units expressing the antisense E6 and E7 messenger RNA (mRNA) for the transforming proteins of the human papilloma virus and the sense mRNA for the retinoblastoma gene in cervical carcinoma cells. Cancer Gene Ther. 1995;2:19–32.
Jeon S, Lambert PF. Integration of human papillomavirus type 16 DNA into the human genome leads to increased stability of E6 and E7 mRNAs: implications for cervical carcinogenesis. Proc Natl Acad Sci USA. 1995;92:1654–8.
Howley PM, Münger K, Romanczuk H, Scheffner M, Huibregtse JM. Cellular targets of the oncoproteins encoded by the cancer associated human papillomaviruses. Princess Takamatsu Symp. 1991;22:239–48.
Münger K, Phelps WC, Bubb V, Howley PM, Schlegel R. The E6 and E7 genes of the human papillomavirus type 16 together are necessary and sufficient for transformation of primary human keratinocytes. J Virol. 1989;63:4417–21.
Mammas IN, Sourvinos G, Giannoudis A, Spandidos DA. Human papilloma virus (HPV) and host cellular interactions. Pathol Oncol Res. 2008. doi: 10.1007/s12253-008-9056-6.
Fehrmann F, Laimins LA. Human papillomaviruses: targeting differentiating epithelial cells for malignant transformation. Oncogene. 2003;22:5201–7.
Ganguly N, Parihar SP. Human papillomavirus E6 and E7 oncoproteins as risk factors for tumorigenesis. J Biosci. 2009;34:113–23.
Sotlar K, Stubner A, Diemer D, Menton S, Menton M, Dietz K, Wallwiener D, Kandolf R, Bültmann B. Detection of high-risk human papillomavirus E6 and E7 oncogene transcripts in cervical scrapes by nested RT-polymerase chain reaction. J Med Virol. 2004;74:107–16.
Kösel S, Burggraf S, Engelhardt W, Olgemöller B. Increased levels of HPV16 E6*I transcripts in high-grade cervical cytology and histology (CIN II+) detected by rapid real-time RT-PCR amplification. Cytopathology. 2007;18:290–9.
McNicol P, Guijon F, Wayne S, Hidajat R, Paraskevas M. Expression of human papillomavirus type 16 E6–E7 open reading frame varies quantitatively in biopsy tissue from different grades of cervical intraepithelial neoplasia. J Clin Microbiol. 1995;33:1169–73.
Kraus I, Molden T, Holm R, Lie AK, Karlsen F, Kristensen GB, Skomedal H. Presence of E6 and E7 mRNA from human papillomavirus types 16, 18, 31, 33, and 45 in the majority of cervical carcinomas. J Clin Microbiol. 2006;44:1310–7.
Cornelissen MT, Smits HL, Briët MA, van den Tweel JG, Struyk AP, van der Noordaa J, ter Schegget J. Uniformity of the splicing pattern of the E6/E7 transcripts in human papillomavirus type 16-transformed human fibroblasts, human cervical premalignant lesions and carcinomas. J Gen Virol. 1990;71:1243–6.
Cricca M, Venturoli S, Leo E, Costa S, Musiani M, Zerbini M. Molecular analysis of HPV 16 E6*I/E6*II spliced mRNAs and correlation with the viral physical state and the grade of the cervical lesion. J Med Virol. 2009. doi: 10.1002/jmv.21496.
Huang LW, Chao SL, Lee BH. Integration of human papillomavirus type-16 and type-18 is a very early event in cervical carcinogenesis. J Clin Pathol. 2008;61:627–31.
Kulmala SM, Syrjänen SM, Gyllensten UB, Shabalova IP, Petrovichev N, Tosi P, Syrjänen KJ, Johansson BC. Early integration of high copy HPV16 detectable in women with normal and low grade cervical cytology and histology. J Clin Pathol. 2006;59:513–7.
Peitsaro P, Johansson B, Syrjänen S. Integrated human papillomavirus type 16 is frequently found in cervical cancer precursors as demonstrated by a novel quantitative real-time PCR technique. J Clin Microbiol. 2002;40:886–91.
Li W, Wang W, Si M, Han L, Gao Q, Luo A, Li Y, Lu Y, Wang S, Ma D. The physical state of HPV16 infection and its clinical significance in cancer precursor lesion and cervical carcinoma. J Cancer Res Clin Oncol. 2008;. doi:10.1007/s00432-008-0413-3.
Sotlar K, Selinka HC, Menton M, Kandolf R, Bültmann B. Detection of human papillomavirus type 16 E6/E7 oncogene transcripts in dysplastic and nondysplastic cervical scrapes by nested RT-PCR. Gynecol Oncol. 1998;69:114–21.
Johnson MA, Blomfield PI, Bevan IS, Woodman CB, Young LS. Analysis of human papillomavirus type 16 E6-E7 transcription in cervical carcinomas and normal cervical epithelium using the polymerase chain reaction. J Gen Virol. 1990;71:1473–9.
Nindl I, Rindfleisch K, Lotz B, Schneider A, Dürst M. Uniform distribution of HPV 16 E6 and E7 variants in patients with normal histology, cervical intra-epithelial neoplasia and cervical cancer. Int J Cancer. 1999;82:203–7.
Castle PE, Cox JT, Jeronimo J, Solomon D, Wheeler CM, Gravitt PE, Schiffman M. An analysis of high-risk human papillomavirus DNA-negative cervical precancers in the ASCUS-LSIL Triage Study (ALTS). Obstet Gynecol. 2008;. doi:10.1097/AOG.0b013e318168460b.
Liverani CA, Ciavattini A, Monti E, Puglia D, Mangano S, DI Giuseppe J, Zizzi A, Goteri G, Bolis G. High risk HPV DNA subtypes and E6/E7 mRNA expression in a cohort of colposcopy patients from Northern Italy with high-grade histologically verified cervical lesions. Am J Transl Res. 2012;4:452–7.
Broccolo F, Fusetti L, Rosini S, Caraceni D, Zappacosta R, Ciccocioppo L, Matteoli B, Halfon P, Malnati MS, Ceccherini-Nelli L. Comparison of oncogenic HPV type-specific viral DNA load and E6/E7 mRNA detection in cervical samples: results from a multicenter study. J Med Virol. 2013;. doi:10.1002/jmv.23487.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pastuszak-Lewandoska, D., Bartosińska-Dyc, A., Migdalska-Sęk, M. et al. HPV16 E6*II gene expression in intraepithelial cervical lesions as an indicator of neoplastic grade: a pilot study. Med Oncol 31, 842 (2014). https://doi.org/10.1007/s12032-014-0842-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-014-0842-6