Abstract
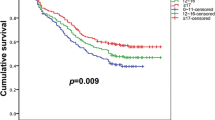
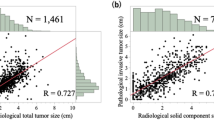
The detection and diagnosis of small-sized (2 cm or less) non-small cell lung cancer (NSCLC) has increased with the development of computed tomography (CT). Over 80% of 5-year survival rate has been reported in surgically treated peripheral lung cancer. There are systematic mediastinal and hilar lymph node involvement pleural invasion and intrapulmonary metastasis even with tumor diameter less than 2 cm. The appropriate surgical procedure for such kinds of lung cancer is lobectomy with mediastinal lymph node dissection. To evaluate the prognostic factors and establish the optimal surgical strategy, we analyzed the clinicopathologic features and survival benefit in different tumor size of peripheral small-sized NSCLC. Among the resected lung cancer cases between January 1999 and July 2001, 185 patients were retrospectively analyzed in surgical methods, lymph node involvement, CT scan findings and survival rates. Survival was analyzed by Kaplan–Meier method and log-rank test. Lymph node involvement was recognized in 26(14.05%) patients. There was no statistically significant difference in the incidence of lymph node involvement between tumors 1.6–2.0 cm (17.82%) in diameter than in those 1.0–1.5 cm (11.94%). There was no lymph node metastasis in tumors less than 1.0 cm in diameter. The 5-year survival rates with or without lymph node involvement were 89.98 and 46.15%, respectively, showing significant difference (P = 0.000). The overall 5-year survival rate was 83.78%. The 5-year survival rate in tumors 1.6–2.0 cm, 1.0–1.5 cm and less than 1.0 cm in diameter was 80.20, 85.07 and 100%, respectively, and showing significant difference(P = 0.035). The 5-year survival rate of 19 patients showing ground-glass opacity (GGO) on CT scan was 94.74% without any metastasis and recurrence after operation. There are systematic mediastinal and hilar lymph node involvement even with tumor diameter less than 2 cm. The results of the present study suggested that systematic lymph node dissection is necessary even for cases with tumor diameter less than 2 cm. However, if the tumor is within 1.0 cm in diameter with obvious GGO showing on chest CT scan, these are good candidates for partial resection without mediastinal lymph node dissection.




Similar content being viewed by others
References
Pirozynski M. 100 years of lung cancer. Respir Med. 2006;100:2073–84.
Arifa P, Pieter EP, Thomas GS. What is early lung cancer? A review of the literature. Lung cancer. 2004;45:267–77.
Ginsberg RJ (2002) Role of surgery in the treatment of stage I and II lung cancer. American Society of Clinical Oncology 2002. Educational book. Thirty-Eight Annual Meeting. May 18–21, 2002, Orlando FL, 460–464.
Park BJ, Altorki NK. Diagnosis and management of early lung cancer. Surg Clin North Am. 2002;82(3):457–76.
Birring SS, Peake MD. Symptoms and the early diagnosis of lung cancer. Thorax. 2005;60:268–9.
Henschke CI, Yankelevitz DF. CT screening for lung cancer: update 2007. Oncologist. 2008;13:65–78.
Cassidy A, Duffy SW, Myles JP, et al. Lung cancer risk prediction: a tool for early detection. Int J Cancer. 2007;120:1–6.
Watanabe T, Okada A, Imakiire T. Intentional limited resection for small peripheral lung cancer based on intraoperative pathologic exploration. Jpn J Thorac Cardiovasc Surg. 2005;53:29–35.
Konaka C, Ikeda N, Hiyoshi T, et al. Peripheral non-small cell lung cancers 2.0 cm or less in diameter: proposed criteria for limited pulmonary resection based upon clinicopathological presentation. Lung Cancer. 1998;21:185–91.
Watanabe S, Oda M, Go T, et al. Should mediastinal nodal dissection be routinely undertaken in patients with peripheral small-sized (2 cm or less) lung cancer? Retrospective analysis of 225 patients. Eur J Cardiothorac Surg. 2001;20:1007–11.
Swanson SJ, Batirel HF. Video-assisted thoracic surgery (VATS) resection for lung cancer. Surg Clin North Am. 2002;82(3):541–59.
Shennib H, Bogart J, Herndon JE, Kohman L, Keenan R, Green M, et al. Video-assisted wedge resection and local radiotherapy for peripheral lung cancer in high-risk patients: the cancer and leukemia group B (CALGB) 9335, a phase II, multi-institutional cooperative group study. J Thorac Cardiovasc Surg. 2005;129:813–8.
Rusch VW. High-resolution computed tomography in clinical T1 N0 M0 adenocarcinoma of the lung[J]. J Thorac Cardiovasc Surg. 2002;124:221–2.
Ohtsuka T, Watanabe K, Kaji M, et al. A clinicopathological study of resected pulmonary nodules with focal pure ground-glass opacity. Eur J Cardiothorac Surg. 2006;30:160–3.
Gomez M, Silvestri GA. Lung cancer screening. Am J Med Sci. 2008;335:46–50.
Sobue T, Moriyama N, Kaneko M, et al. Screening for lung cancer with low-dose helical computed tomography: anti-lung cancer association project. J Clin Oncol. 2002;20:911–20.
Koike T, Yamato Y, Yoshiya K, et al. Criteria for intentional limited pulmonary resection in cT1N0M0 peripheral lung cancer. Jpn J Thorac Cardiovasc Surg. 2003;51:515–9.
Nakamura H, Saji H, Ogata A, et al. Lung cancer patients showing pure ground-glass opacity on computed tomography are good candidates for wedge resection. Lung Cancer. 2004;44:61–8.
Matsuguma H, Yokoi K, Anraku M, et al. Proportion of ground-glass opacity on high-resolution computed tomography in clinical T1 N0 M0 adenocarcinoma of the lung a predictor of lymph node metastasis. J Thorac Cardiovasc Surg. 2002;124:278–84.
Nakata M, Sawada S, Saeki H, et al. Prospective study of thoracoscopic limited resection for ground-glass opacity selected by computed tomography. Ann Thorac Surg. 2003;75:1601–5.
Ginsberg RJ, Rubinstein LV, Lung Study Group. Randomized trial of lobectomy versus limited resection for T1N0 non-small cell lung cancer. Ann Thorac Surg. 1995;60:615–23.
Patz EF, Rossi S, Harpole DH, et al. Correlation of tumor size and survival in patients with stage IA non-small cell lung cancer. Chest. 2000;117:1568–71.
Pasic A, Postmus PE, Sutedja TG. What is early lung cancer? A review of the literature. Lung Cancer. 2004;45:267–77.
Detterbeck FC, Boffa DJ, Tanoue LT. The new lung cancer staging system. Chest. 2009;136:260–71.
Suzuki K, Nagai K, Yoshida J, et al. Predictors of lymph node and intrapulmonary metastasis in clinical stage IA non-small cell lung carcinoma. Ann Thorac Surg. 2001;72:352–6.
Fukui T, Mori S, Yokoi K, et al. T significance of the number of positive lymph nodes in resected non-small cell lung cancer. J Thorac Oncol. 2006;1:120–5.
Hung JJ, Wang CY, Huang MH, et al. Prognostic factors in resected stage I non-small cell lung cancer with a diameter of 3 cm or less: visceral pleural invasion did not influence overall and disease-free survival. J Thorac Cardiovasc Surg. 2007;134:638–43.
Miller DL, Rowland CR, Deschamps C, et al. Surgical treatment of non-small cell lung cancer 1 cm or less in diameter. Ann Thorac Surg. 2002;73:1545–51.
Takizawa T, Terashima M, Koike T, et al. Lymph node metastasis in small peripheral adenocarcinoma of the lung [J]. J Thorac Cardiovasc Surg. 1998;116:276–80.
Kim BT, Kim Y, Lee KS, et al. Localized form of bronchioloalveolar carcinoma. AJR. 1998;170:935–9.
Nakajima R, Yokose T, Kakinuma R, et al. Localized pure ground-glass opacity on high-resolution CT: histologic characteristics. J Comput Assist Tomogr. 2002;26:323–9.
Kodama K, Higashiyama M, Yokouchi H, et al. Natural history of pure ground-glass opacity after long-term follow-up of more than 2 years. Ann Thorac Surg. 2002;73:386–93.
Aoki T, Nakata H, Watanabe H, et al. Evolution of peripheral lung adenocarcinomas: CT findings correlated with histology and tumor doubling time. AJR. 2000;174:763–8.
Yamato Y, Tsuchida M, Watanabe T, et al. Early resection for brochioloalveolar adenocarcinoma of the lung. Ann Thorac Surg. 2001;71:971–4.
Yoshida J, Nagai K, Yokose T, et al. Limited resection trial of pulmonary ground-glass opacity nodules: fifty-case experience. J Thorac Cardiovasc Surg. 2005;129:991–6.
Yamato Y, Tsuchida M, Watanabe T, et al. Early results of a prospective study of limited resection for bronchioloalveolar adenocarcinoma of the lung. Ann Thorac Surg. 2001;71:971–4.
Nakata M, Sawada S, Yamashita M, et al. Objective radiologic analysis of ground-glass opacity aimed at curative limited resection for small peripheral non-small cell lung cancer. J Thorac Cardiovasc Surg. 2005;129:1226–31.
Lung Cancer Study Group. Randomized trial of lobectomy versus limited resection for T1N0 non-small cell lung cancer. Ann Thorac Surg. 1995;60:615–23.
Kondo D, Yamada K, Kitayama Y, et al. Peripheral lung adenocarcinomas: 10 mm or less in diameter. Ann Thorac Surg. 2003;76:350–5.
Ikeda N, Maeda J, Yashima K, et al. A clinicopathological study of resected adenocacinoma 2 cm of less in diameter. Ann Thorac Surg. 2004;78:1011–6.
Inoue M, Minami M, Shiono H, et al. Clinicopathologic study of resected, peripheral, small-sized, non-small cell lung cancer tumors of 2 cm or less in diameter: pleural invasion and increase of serum carcinoembryonic antigen level as predictors of nodal involvement. J Thorac Cardiovasc Surg. 2006;131:988–93.
Fukui T, Katayama T, Ito S, et al. Clinicopathological features of small-sized non-small cell lung cancer with mediastinal lymph node metastasis. Lung Cancer. 2009;66:309–13.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shi, CL., Zhang, XY., Han, BH. et al. A clinicopathological study of resected non-small cell lung cancers 2 cm or less in diameter: a prognostic assessment. Med Oncol 28, 1441–1446 (2011). https://doi.org/10.1007/s12032-010-9632-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12032-010-9632-y