Abstract
Purpose
Hepatocellular carcinoma (HCC) is most often a sequela of chronic liver disease or chronic hepatitis B infection. Among high-risk patients, surveillance for HCC every 6 months is recommended by international guidelines. However, rates of HCC surveillance are suboptimal (11–64%). Barriers at the patient, provider, and healthcare delivery system levels have been identified.
Methods
We performed a systemic scoping review to identify and characterize interventions to improve HCC surveillance that has previously been evaluated. Searches using key terms in PubMed and Embase were performed to identify studies examining interventions designed to improve the surveillance rate for HCC in patients with cirrhosis or chronic liver disease that were published in English between January 1990 and September 2021.
Results
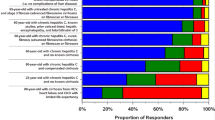
Included studies (14) had the following study designs: (1) randomized clinical trials (3, 21.4%), (2) quasi-experimental (2, 14.3%), (3) prospective cohort (6, 42.8%), and (4) retrospective cohort (3, 21.4%). Interventions included mailed outreach invitations, nursing outreach, patient education with or without printed materials, provider education, patient navigation, chronic disease management programs, nursing-led protocols for image ordering, automated reminders to physicians and nurses, web-based clinical management tools, HCC surveillance databases, provider compliance reports, radiology-led surveillance programs, subsidized HCC surveillance, and the use of oral medications. It was found that HCC surveillance rates increased after intervention implementation in all studies.
Conclusion
Despite improvements in HCC surveillance rates with intervention, compliance remained suboptimal. Further analysis of which interventions yield the greatest increases in HCC surveillance, design of multi-pronged strategies, and improved implementation are needed.

Similar content being viewed by others
Abbreviations
- HCC:
-
Hepatocellular carcinoma
- HBV:
-
Hepatitis B virus
- HCV:
-
Hepatitis C virus
- AASLD:
-
American Association for the Study of Liver Diseases
- EASL-EORTC:
-
European Association for the Study of the Liver and European Organization for Research and Treatment of Cancer
- APASL:
-
Asian Pacific Association for the Study of the Liver
- NCCN:
-
National Comprehensive Cancer Network (NCCN)
- US:
-
Ultrasound
- AFP:
-
Alpha-fetoprotein
- UK:
-
United Kingdom
- NCSP:
-
National Cancer Screening Program
- USPSTF:
-
United States Preventive Services Task Force
References
El-Serag HB. Epidemiology of viral hepatitis and hepatocellular carcinoma. Gastroenterology; 142. Epub ahead of print 2012. https://doi.org/10.1053/j.gastro.2011.12.061.
Sangiovanni A, Prati GM, Fasani P, et al. The natural history of compensated cirrhosis due to hepatitis C virus: a 17-year cohort study of 214 patients. Hepatology. 2006;43:1303–10.
Singal AG, Lampertico P, Nahon P. Epidemiology and surveillance for hepatocellular carcinoma: new trends. J Hepatol. 2020 Feb;72(2):250–61. https://doi.org/10.1016/j.jhep.2019.08.025. http://gco.iarc.fr/today.
El-Serag HB. Hepatocellular carcinoma: recent trends in the United States. In: Gastroenterology. W.B. Saunders, 2004. Epub ahead of print 2004. https://doi.org/10.1053/j.gastro.2004.09.013.
Singal AG, Marrero JA. Recent advances in the treatment of hepatocellular carcinoma. Curr Opin Gastroenterol. 2010;26:189–95.
Kansagara D, Papak J, Pasha AS, et al. Screening for hepatocellular carcinoma in chronic liver disease: a systematic review. Ann Intern Med. 2014;161:261–9.
Kanwal F, Singal AG. Surveillance for hepatocellular carcinoma: current best practice and future direction. Gastroenterology. 2019;157:54–64.
Heimbach JK, Kulik LM, Finn RS, et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology. 2018;67:358–80.
EASL. EASL Clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2018;69:182–236.
Benson AB, D’Angelica MI, Abbott DE, et al. Hepatobiliary cancers, Version 2.2021. JNCCN J Natl Compr Canc Netw. 2021;19:541–565.
Marrero JA, Kulik LM, Sirlin CB, et al. Diagnosis, Staging, and Management of Hepatocellular Carcinoma: 2018 Practice guidance by the American Association for the Study of Liver Diseases. Hepatology. 2018;68:723–50.
Bruix J, Sherman M. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53:1020–2.
Eslam M, Sarin SK, Wong VWS, et al. The Asian Pacific Association for the Study of the Liver clinical practice guidelines for the diagnosis and management of metabolic associated fatty liver disease. Hep Intl. 2020;14:889–919.
Singal AG, Yopp A, Skinner CS, et al. Utilization of hepatocellular carcinoma surveillance among American patients : a systematic review. J Gen Intern Med. 2012;27:861–7.
Farvardin S, Patel J, Khambaty M, et al. Patient-reported barriers are associated with lower hepatocellular carcinoma surveillance rates in patients with cirrhosis. Hepatology. 2017;65:875–84.
Dalton-Fitzgerald E, Tiro J, Kandunoori P, et al. Practice patterns and attitudes of primary care providers and barriers to surveillance of hepatocellular carcinoma in patients with cirrhosis. Clin Gastroenterol Hepatol. 2016;13:791–8.
Singal AG, Tiro JA, Murphy CC, et al. Patient-reported barriers are associated with receipt of hepatocellular carcinoma surveillance in a multicenter cohort of patients with cirrhosis. Clin Gastroenterol Hepatol. 2021;19:987-995.e1.
Mahfouz M, Nguyen H, Tu J, et al. Knowledge and perceptions of hepatitis B and hepatocellular carcinoma screening guidelines among trainees: a tale of three centers. Dig Dis Sci. 2020;65:2551–61.
Goldberg DS, Taddei TH, Serper M, et al. Identifying barriers to hepatocellular sample of patients with cirrhosis. 2017;65:864–74.
El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology. 2007;132:2557–76.
Artinyan A, Mailey B, Sanchez-Luege N, et al. Race, ethnicity, and socioeconomic status influence the survival of patients with hepatocellular carcinoma in the United States. Cancer. 2010;116:1367–77.
Arksey H, Malley LO. Scoping studies : towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32.
Levac D, Colquhoun H, Brien KKO. Scoping studies : advancing the methodology. Implement Sci. 2010;5:1–9.
Singal AG, Tiro JA, Marrero JA, et al. Mailed outreach program increases ultrasound screening of patients with cirrhosis for hepatocellular carcinoma. Gastroenterology. 2017;152:608-615.e4.
Singal AG, Tiro JA, Murphy CC, et al. Mailed outreach invitations significantly improve HCC surveillance rates in patients with cirrhosis: a randomized clinical trial. Hepatology; 69. Epub ahead of print 2019. https://doi.org/10.1002/hep.30129/suppinfo.
Wigg AJ, McCormick R, Wundke R, et al. Efficacy of a chronic disease management model for patients with chronic liver failure. Clin Gastroenterol Hepatol. 2013;11:850-858.e4.
Shaw J, Patidar KR, Reuter B, et al. Focused education increases hepatocellular cancer screening in patients with cirrhosis regardless of functional health literacy. Dig Dis Sci. 2021;66:2603–9.
Cahill JA, Rizvi S, Saeian K. Assessment of adherence to baseline quality measures for cirrhosis and the impact of performance feedback in a Regional VA Medical Center. Am J Med Qual. 2018;33:262–8.
O’Leary DA, Cropp E, Isaac D, et al. “B in IT” - a community-based model for the management of hepatitis B patients in primary care clinics using a novel web-based clinical tool. Hepatol Med Policy. 2018;3:1–10.
Kim HY, Kim CW, Choi JY, et al. A decade-old change in the screening rate for hepatocellular carcinoma among a hepatitis b virus-infected population in Korea. Chin Med J (Engl). 2016;129:15–21.
Aberra FB, Essenmacher M, Fisher N, et al. Quality improvement measures lead to higher surveillance rates for hepatocellular carcinoma in patients with cirrhosis. Dig Dis Sci. 2013;58:1157–60.
Kennedy NA, Rodgers A, Altus R, et al. Optimisation of hepatocellular carcinoma surveillance in patients with viral hepatitis: a quality improvement study. Intern Med J. 2013;43:772–7.
Rogal SS, Yakovchenko V, Gonzalez R, et al. The hepatic innovation team collaborative: a successful population-based approach to hepatocellular carcinoma surveillance. Cancers (Basel). 2021;13:1–10.
Beste LA, Ioannou GN, Yang Y, et al. Improved surveillance for hepatocellular carcinoma with a primary care-oriented clinical reminder. Clin Gastroenterol Hepatol. 2015;13:172–9.
Allard N, Cabrie T, Wheeler E, et al. The challenge of liver cancer surveillance in general practice: do recall and reminder systems hold the answer? Aust Fam Physician. 2017;46:859–64.
Nam JY, Lee JH, Kim HY, et al. Oral medications enhance adherence to surveillance for hepatocellular carcinoma and survival in chronic hepatitis B patients. PLoS ONE. 2017;12:1–14.
Farrell C, Halpen A, Cross TJS, et al. Ultrasound surveillance for hepatocellular carcinoma: service evaluation of a radiology-led recall system in a tertiary-referral centre for liver diseases in the UK. Clin Radiol. 2017;72(338):e11-338.e17.
Sabatino SA. Updated recommendations for client- and provider-oriented interventions to increase breast, cervical, and colorectal cancer screening. Am J Prev Med. 2012;43:92–6.
Holden DJ, Jonas DE, Porterfield DS, et al. Systematic review: enhancing the use and quality of colorectal cancer screening. 2010. www.annals.org.
Bonfill Cosp X, Marzo Castillejo M, Pladevall Vila M, et al. Strategies for increasing the participation of women in community breast cancer screening. Cochrane Database Syst Rev. 2016. Epub ahead of print 22 January 2001. https://doi.org/10.1002/14651858.CD002943.
Duffy SW, Myles JP, Maroni R, et al. Rapid review of evaluation of interventions to improve participation in cancer screening services. J Med Screen. 2017;24:127–45.
Dougherty MK, Brenner AT, Crockett SD, et al. Evaluation of interventions intended to increase colorectal cancer screening rates in the United States: a systematic review and meta-analysis. JAMA Intern Med. 2018;178:1645–58.
Acharya A, Markar SR, Sodergren MH, et al. Meta-analysis of adjuvant therapy following curative surgery for periampullary adenocarcinoma. Br J Surg. Epub ahead of print 2017. https://doi.org/10.1002/bjs.10563.
Shojania KG, Jennings A, Mayhew A, et al. Effect of point-of-care computer reminders on physician behaviour: a systematic review. CMAJ Can Med Assoc J. 182. Epub ahead of print 23 March 2010. https://doi.org/10.1503/cmaj.090578.
Pedersen ER, Rubenstein L, Kandrack R, et al. Elusive search for effective provider interventions: a systematic review of provider interventions to increase adherence to evidence-based treatment for depression. Implement Sci. 13. Epub ahead of print 20 July 2018. https://doi.org/10.1186/s13012-018-0788-8.
Thomson MJ, Lok AS, Tapper EB. Optimizing medication management for patients with cirrhosis: evidence-based strategies and their outcomes. Liver Int. 2018;38:1882–90.
Episoft. https://episofthealth.com/our-story/. Accessed 25 April 2023.
AviTracks. https://www.avicenna-medical.com/specialty-disease-management-software-hepatology. Accessed 25 April 2023.
Lok ASF, Mcmahon BJ, Brown RS, et al. Antiviral therapy for chronic hepatitis B viral infection in adults: a systematic review and meta-analysis. Epub ahead of print 2015. https://doi.org/10.1002/hep.28280/suppinfo.
Russo MW. Antiviral therapy for hepatitis C is associated with improved clinical outcomes in patients with advanced fibrosis. Expert Rev Gastroenterol Hepatol. 2010;4:535–9.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Literature review, data collection, and analysis were performed by Molly McNamara and Eliza Beal. The first draft of the manuscript was written by Molly McNamara, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Beal, E.W., McNamara, M., Owen, M. et al. Interventions to Improve Surveillance for Hepatocellular Carcinoma in High-Risk Patients: A Scoping Review. J Gastrointest Canc 55, 1–14 (2024). https://doi.org/10.1007/s12029-023-00944-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12029-023-00944-1