Abstract
Purpose
Location of the primary tumor is prognostic and predictive of efficacy with VEGF-inhibitors (I) versus EGFR-I given first-line to metastatic colorectal cancer (mCRC) patients. However, little is known regarding the effect of location on prognosis and prediction in refractory mCRC. We assessed the efficacy of VEGF-I and EGFR-I in regards to location of the primary tumor in patients with refractory mCRC enrolled in early phase studies.
Methods
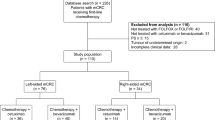
A historical cohort analysis of mCRC patients, including 44 phase I trials our institution, from March 2004 to September 2012. Median Progression free survival (mPFS) and overall survival (mOS) were estimated from Kaplan-Meier curves and groups were statistically compared with the log-rank test.
Results
One hundred thirty-nine patients with a median age 59 (33–81). 73.9% received 3+ lines of therapy. All KRAS wild-type patients had received prior EGFR-I. Location: right 20.9%, left 61.9%, and transverse 4.3%. For survival analysis, transverse CRC were included with right. Of the 112 patients, mOS was left (N = 80) 6.6 months versus right (N = 32) 5.9 months, P = 0.18. mPFS was left (n = 86) 2.0 months versus right (N = 35) 2.0 months, P = 0.76. In subgroup analysis, survival was significant for KRAS wild-type patients with left-sided mCRC had mOS of 6.2 months with other agents versus 9.4 months with EGFR-I (P = 0.03).
Conclusions
In phase 1 clinical trials, although location alone was not prognostic in heavily pretreated patients, left-sided mCRC had improved survival with EGFR-I. Despite progression on EGFR-I, left-sided KRAS wild mCRC patients should be considered for phase 1 studies of agents targeting growth factor pathways.
Similar content being viewed by others
References
Benson 3rd AB, Bekaii-Saab T, Chan E, Chen YJ, Choti MA, Cooper HS, Engstrom PF, Enzinger PC, Fakih MG, Fenton MJ, Fuchs CS, Grem JL, Hunt S, Kamel A, Leong LA, Lin E, May KS, Mulcahy MF, Murphy K, Rohren E, Ryan DP, Saltz L, Sharma S, Shibata D, Skibber JM, Small Jr W, Sofocleous CT, Venook AP, Willett CG, Gregory KM, Freedman-Cass DA. Metastatic colon cancer, version 3.2013: featured updates to the NCCN guidelines. Journal of the National Comprehensive Cancer Network : JNCCN. 2013;11(2):141–52. quiz 152
Gervaz P, Bucher P, Morel P. Two colons-two cancers: paradigm shift and clinical implications. J Surg Oncol. 2004;88(4):261–6. doi:10.1002/jso.20156.
Bufill JA. Colorectal cancer: evidence for distinct genetic categories based on proximal or distal tumor location. Ann Intern Med. 1990;113(10):779–88.
Warschkow R, Sulz MC, Marti L, Tarantino I, Schmied BM, Cerny T, Guller U. Better survival in right-sided versus left-sided stage I – III colon cancer patients. BMC Cancer. 2016;16:554. doi:10.1186/s12885-016-2412-0.
Tejpar S, Stintzing S, Ciardiello F, Tabernero J, Van Cutsem E, Beier F, Esser R, Lenz HJ, Heinemann V. Prognostic and predictive relevance of primary tumor location in patients with RAS wild-type metastatic colorectal cancer: retrospective analyses of the CRYSTAL and FIRE-3 trials. JAMA Oncol. 2016; doi:10.1001/jamaoncol.2016.3797.
Brule SY, Jonker DJ, Karapetis CS, O'Callaghan CJ, Moore MJ, Wong R, Tebbutt NC, Underhill C, Yip D, Zalcberg JR, Tu D, Goodwin RA. Location of colon cancer (right-sided versus left-sided) as a prognostic factor and a predictor of benefit from cetuximab in NCIC CO.17. Eur J Cancer. 2015;51(11):1405–14. doi:10.1016/j.ejca.2015.03.015.
Kim SE, Paik HY, Yoon H, Lee JE, Kim N, Sung MK. Sex- and gender-specific disparities in colorectal cancer risk. World journal of gastroenterology : WJG. 2015;21(17):5167–75. doi:10.3748/wjg.v21.i17.5167.
Nitsche U, Stogbauer F, Spath C, Haller B, Wilhelm D, Friess H, Bader FG. Right sided colon cancer as a distinct histopathological subtype with reduced prognosis. Dig Surg. 2016;33(2):157–63. doi:10.1159/000443644.
Guinney J, Dienstmann R, Wang X, de Reynies A, Schlicker A, Soneson C, Marisa L, Roepman P, Nyamundanda G, Angelino P, Bot BM, Morris JS, Simon IM, Gerster S, Fessler E, De Sousa EMF, Missiaglia E, Ramay H, Barras D, Homicsko K, Maru D, Manyam GC, Broom B, Boige V, Perez-Villamil B, Laderas T, Salazar R, Gray JW, Hanahan D, Tabernero J, Bernards R, Friend SH, Laurent-Puig P, Medema JP, Sadanandam A, Wessels L, Delorenzi M, Kopetz S, Vermeulen L, Tejpar S. The consensus molecular subtypes of colorectal cancer. Nat Med. 2015;21(11):1350–6. doi:10.1038/nm.3967.
Mao C, Wu XY, Yang ZY, Threapleton DE, Yuan JQ, Yu YY, Tang JL. Concordant analysis of KRAS, BRAF, PIK3CA mutations, and PTEN expression between primary colorectal cancer and matched metastases. Sci Rep. 2015;5:8065. doi:10.1038/srep08065.
Janku F. Tumor heterogeneity in the clinic: is it a real problem? Ther Adv Med Oncol. 2014;6(2):43–51. doi:10.1177/1758834013517414.
Acknowledgements
NCI P30CA054174 (All Authors), NIA P30AG044271 (Sukeshi Patel Arora).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Funding
P30 Cancer Center Support Grant No. CA054174 (all authors), NIA P30AG044271 (Sukeshi Patel Arora).
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Arora, S.P., Ketchum, N.S., Michalek, J. et al. Left Versus Right: Does Location Matter for Refractory Metastatic Colorectal Cancer Patients in Phase 1 Clinical Trials?. J Gastrointest Canc 49, 283–287 (2018). https://doi.org/10.1007/s12029-017-9948-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12029-017-9948-3