Abstract
Background
The objective of this study was to analyze the impact of a structured educational intervention on the implementation of guideline-recommended pain, agitation, and delirium (PAD) assessment.
Methods
This was a prospective, multinational, interventional before-after trial conducted at 12 intensive care units from 10 centers in Germany, Austria, Switzerland, and the UK. Intensive care units underwent a 6-week structured educational program, comprising online lectures, instructional videos, educational handouts, and bedside teaching. Patient-level PAD assessment data were collected in three 1-day point-prevalence assessments before (T1), 6 weeks after (T2), and 1 year after (T3) the educational program.
Results
A total of 430 patients were included. The rate of patients who received all three PAD assessments changed from 55% (107/195) at T1 to 53% (68/129) at T2, but increased to 73% (77/106) at T3 (p = 0.003). The delirium screening rate increased from 64% (124/195) at T1 to 65% (84/129) at T2 and 77% (82/106) at T3 (p = 0.041). The pain assessment rate increased from 87% (170/195) at T1 to 92% (119/129) at T2 and 98% (104/106) at T3 (p = 0.005). The rate of sedation assessment showed no signficiant change. The proportion of patients who received nonpharmacological delirium prevention measures increased from 58% (114/195) at T1 to 80% (103/129) at T2 and 91% (96/106) at T3 (p < 0.001). Multivariable regression revealed that at T3, patients were more likely to receive a delirium assessment (odds ratio [OR] 2.138, 95% confidence interval [CI] 1.206–3.790; p = 0.009), sedation assessment (OR 4.131, 95% CI 1.372–12.438; p = 0.012), or all three PAD assessments (OR 2.295, 95% CI 1.349–3.903; p = 0.002) compared with T1.
Conclusions
In routine care, many patients were not assessed for PAD. Assessment rates increased significantly 1 year after the intervention.
Clinical trial registration ClinicalTrials.gov: NCT03553719.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Pain, agitation/sedation, and delirium (PAD) are common among critically ill patients. Previous studies have shown that pain is experienced by about half of medical and surgical intensive care unit (ICU) patients at rest [1, 2], severe or dangerous agitation is present in about half of ICU patients [3], 27% of ICU patients have been found to be deeply sedated [4], and up to 82% of ICU patients undergoing mechanical ventilation are affected by delirium [5, 6]. PAD are detrimental to patient outcomes. High-quality pain management reduces the duration of mechanical ventilation and the nosocomial infection rate [7], and early deep sedation is an independent predictor for delayed extubation and 6-month mortality [8]. Delirium is associated with a longer duration of mechanical ventilation [6], longer hospitalization [5, 6], increased mortality [9, 10], and higher rates of long-term cognitive impairment [11]. Hence, PAD management is an integral part of intensive care [12,13,14].
Guidelines recommend that PAD should be assessed every 8 h using validated screening tools [12,13,14]. Self-assessment is useful among patients able to report pain (e.g., the Numeric Rating Scale [NRS]) [15], alternatively observational tools such as the Behavioral Pain Scale (BPS) [16, 17] or the Critical-Care Pain Observation Tool for those unable to [12,13,14, 18]. Guidelines consider the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) [19] and the Intensive Care Delirium Screening Checklist (ICDSC) [20] as the most suitable delirium screening instruments and recommend the Richmond Agitation Sedation Scale (RASS) [21] or the Sedation Agitation Scale [22] for sedation assessment [12,13,14].
Despite the relevance of evidence-based PAD assessment, previous studies from routine care have indicated poor implementation rates in various settings. In a multinational survey in 2019/20 among a convenience sample of 1474 intensivists, 95.4% of respondents reported assessing delirium daily, but two thirds only assessed patients they considered to be at risk [23]. Although 85.4% of participants responded to assess sedation levels and 86.7% responded to assess pain in patients able to communicate, only two thirds assessed pain in those unable to communicate [23]. In a 2014 survey among 101 European ICUs, 49%, 30%, and 79% of centers reported the 8-hourly assessments of pain, agitation or delirium, respectively, but under half of patients in this study actually received PAD monitoring [24]. These results mirror surveys from Poland in 2016 [25], Belgium in 2011 [26], Australia/New Zealand in 2006/7 [27], Canada in 2002 [28], and Germany in 2002 [29].
Structured face-to-face training and e-learning have been employed as effective strategies to increase staff knowledge and improve the frequency and quality of routine PAD assessment in previous studies [30,31,32,33,34,35,36,37]. A prospective cohort study on three German ICUs of one university hospital showed an improvement in PAD screening rates more than 1 year following the implementation of formal and bedside teaching as well as the provision of educational resources and delirium support teams [38].
We are not aware of recent data on the real-world, guideline-adherent PAD assessment rates in European ICUs. In this prospective before-after trial among patients of 12 European ICUs, we first investigated whether PAD assessment rates change 6 weeks and 1 year following a structured educational program. Second, we explored which patient-specific characteristics might determine whether a patient was assessed for pain, sedation, or delirium.
Methods
Study Design
In this prospective, multinational, interventional before-after trial, data on the assessment of delirium, analgesia, and sedation for inpatients in participating adult ICUs were collected at three 1-day (i.e., 24-h) point-prevalence assessments. Immediately after the first 1-day assessment from December 2018 to January 2019, study sites underwent a structured 6-week educational program, aimed at improving the frequency and quality of PAD assessments. The educational program was based on a previously published extensive training algorithm [38]. Data for two additional 1-day point prevalences were collected 6 weeks (May–June 2019) and 1 year (March–May 2020) after the conclusion of the educational program (Fig. 1). The study adhered to the ethical standards of the Declaration of Helsinki and its later amendments and its protocol was registered at ClinicalTrials.gov on June 12, 2018 (Identifier: NCT03553719). Ethical approval at the coordinating study site was granted by the Institutional Review Board (IRB) of Charité–Universitätsmedizin Berlin (EA2/022/18) on March 23, 2018. Participating centers obtained their IRB approval before study commencement as required by local regulations. Written consent or a waiver was subject to the decision of the local IRBs.
Trial ICUs and Participants
The trial was hosted by Charité–Universitätsmedizin Berlin and conducted at 12 European adult ICUs from 10 centers, located in Germany, the UK, Austria, and Switzerland (Table S1). Centers were recruited from members of the Working Group Postoperative Delirium and Cognitive Dysfunction of the European Society of Intensive Care Medicine and its NEXT Committee.
Patients qualified for inclusion if they were treated in a participating ICU on a day of a point-prevalence assessment and were ≥ 18 years of age. Patients were excluded for blindness, deafness, or an insurmountable language barrier.
Structured Educational Program
We applied a structured educational algorithm pertaining to PAD based on a previously described training algorithm [38]. In short, the educational program consisted of three 2-week cycles and was based on the train-the-trainer concept. It combined theoretical lectures, handouts with key points, instructional videos, and bedside teaching. On the first 4 days of each cycle, trained PAD experts from Charité (MR and BW) provided participants of all study centers with 30–45-min webinars on the assessment of sedation and pain, the minimization of sedation, the pathophysiology, symptomatology, prevention, and detection of delirium, and provided a demonstration of the CAM-ICU. These webinars were recorded and provided to participants for later review and dissemination. All informational content was distributed to local study coordinators to adapt into their units’ practice, providing the core messages and structure remained unchanged. On the fifth day of each cycle, theoretical teaching was followed by 2–2.5-h face-to-face bedside teaching from PAD experts at each participating center, with immediate feedback and debriefing for participants. PAD experts were consultants with expertise in pain, sedation and delirium, and they were part of the study team. Bedside teaching also addressed a potential lack of documentation of assessments. At three centers where the local PAD expert was not available, bedside teaching was provided by a PAD expert from Charité (MR or BW). In the second week of each cycle, ICU staff were expected to apply the learning content in routine care. Our overarching goal was to train local “PAD leaders.” Local project leaders were tasked with recruting interested staff members. Participation was voluntary and open to all ICU staff members (doctors, nurses, and other health care professionals), but most participants were ICU nurses. Every center received its individual training to keep group sizes small and lower the barriers for questions during the training. Training of centers was performed sequentially and in close temporal proximity (Fig. 1).
Outcomes
The primary outcome was the percentage of patients screened for delirium at least once on the day of the point-prevalence assessment (delirium screening rate). Secondary outcomes comprised percentage of patients who received at least one pain or sedation assessment on the day of the point-prevalence assessment (pain and sedation assessment rates), delirium, pain, and sedation screening tools used, respective pain and sedation scores, delirium prevalence in routine delirium screening, and nonpharmacological measures to prevent or treat delirium (i.e., reorientation method, early mobilization, and sensory shielding) [39,40,41].
Data Collection
Patient characteristics, treatment data, and PAD management were recorded for each patient in an electronic case report form (LimeSurvey, Hamburg, Germany). Data on PAD assessment were taken from the patients’ health care records to obtain information on the current ICU practice. The assessors were therefore ICU physicians and nurses as per local standard. Data were stored on a secure server on the premises of the coordinating study site and handled according to European Union General Data Protection Regulations. Except for local study coordinators, ICU staff was unaware of the assessment days. Local study coordinators were also prompted to pick days that were not particularly busy or had usual staffing.
Data Analysis
In previously published work [24], 27% of patients received routine delirium screening prior to an educational program, and in a study implementing an educational program similar to our proposed intervention, the routine delirium screening rate increased by about 15% after a month of training [42]. According to our a priori sample size calculation, we could detect an increase in screening rate from 27% before the educational program to 42% following the educational program if each participating ICU enrolled 14 patients on average (170 patients total) per assessment point, with a power of at least 0.8 and a two-tailed significance level of 0.05 (Fisher’s exact test; nQuery Advisor 7.0, Statsols, Cork, Ireland). Although sample size planning was done conservatively on the basis of a simple two-group test, we planned to account for the clustered data structure in the analysis.
Descriptive statistics of the study population are either presented as medians with limits of the interquartile range (IQR) or absolute (n) with relative frequencies (%). Patient characteristics and PAD assessment points were compared using Pearson’s χ2 tests for categorical variables and Kruskal–Wallis test for continuous variables. Adjustments were not made for multiple testing. Multivariable mixed-effect logistic regression analyses were used to assess the association between the assessment points and the likelihood for a patient to receive a delirium, sedation, or pain assessment, all PAD assessments, or nonpharmacological measures to prevent or treat delirium, respectively. The regression models included sex, age, extracorporeal membrane oxygenation provision (yes/no), and mechanical ventilation (yes/no) as fixed effects. To account for the clustered nature of the data, a random effect for the treating country was added (Germany, Austria, Switzerland, or the UK). Statistical analyses were performed using Stata 17SE (StataCorp LP, College Station, TX).
Results
Study Population
A total of 430 patients from 12 ICUs from 10 centers were included, with 195 patients at the first (December 2018–January 2019), 129 patients from 8 centers at the second (May–June 2019), and 106 patients from 6 centers at the third (March–May 2020) 24-h assessment point. Recruitment by center and assessment point is shown in Table S1.
At the first, second, and third assessment points 76%, 66%, and 72% of patients, respectively, were mechanically ventilated. The median Simplified Acute Physiology Score II scores at admission were 37 (IQR 27–53), 41.5 (IQR 31.5–49), and 40 (IQR 28–51). There were no significant differences between patients of the three assessment points with respect to age, sex, height, weight, admitting diagnosis, current length of ICU stay, organ support received, mechanical ventilation, extracorporeal membrane oxygenation provision, and severity of illness (Table 1).
Delirium, Sedation, and Pain Assessments
Delirium screening was performed in 64% (124/195) of patients at least once daily at baseline. The CAM-ICU was used in 56% (109/195) of patients, the nursing delirium screening scale in 4% (7/195), and the ICDSC in 5% (10/195) of patients. Two patients received both CAM-ICU and ICDSC assessments. After completion of the educational program, the delirium screening rate increased to 65% (84/129) at 6 weeks, and 77% (82/106) at 1 year (p = 0.041). Among those screened, 26% (32/124), 23% (19/84), and 13% (11/82) screened positive for delirium at assessment points 1, 2, and 3, respectively. Screening for delirium at assessment points 2 and 3 was conducted solely using the CAM-ICU, as the two centers using the ICDSC and nursing delirium screening scale at assessment point 1 did not recruit patients at later assessment points (Table 2, Fig. 2a, Fig. S1a).
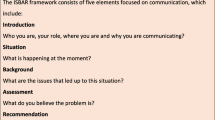
Percentage of patients who received a a delirium screening, b sedation assessment, c pain assessment, or d complete PAD assessment (delirium, sedation, and pain), by assessment point. In percentages. Assessment point 1 comprised n = 195 patients. Assessment point 2 comprised n = 129 patients. Assessment point 3 comprised n = 106 patients. Pearson’s χ2 test for differences between assessment points for delirium screening (p = 0.041), sedation assessment (p = 0.182), pain assessment (p = 0.005), and complete PAD assessment (p = 0.003). PAD pain, agitation, and delirium
At baseline, 58% (114/195) of patients received nonpharmacological measures to prevent or treat delirium. After the educational program, 80% (103/129) received nonpharmacological measures at assessment point 2, and 91% (96/106) at assessment point 3 (p < 0.001). The most common measure was reorientation (e.g., clock or whiteboard), which was used in 45% (87/195), 53% (68/129), and 67% (71/106) of patients at assessment points 1, 2, and 3, respectively (p = 0.001). The second most common nonpharmacological measure was early mobilization, which was provided to 43% (83/195), 46% (59/129), and 58% (61/106) of patients at assessment points 1, 2, and 3, respectively (p = 0.042).
Sedation depth was assessed in 88% (171/195) of patients at least once per day at baseline. After the educational program, 86% (111/129) received sedation depth assessment at assessment point 2, and 93% (99/106) at assessment point 3 (p = 0.182). RASS was used in 87% (169/195), 86% (111/129), and 74% (78/106) of patients (p = 0.009). The Sedation Agitation Scale was not used in any ICUs. Other sedation scales included the alert, verbal, pain, unresponsive scale, which was used in 20% (21/106) of patients, all of which were treated in one UK center at assessment point 3 (Table 2, Fig. 2b, Fig. S1c).
Pain was evaluated in 87% (170/195) of patients at least once per day at baseline. After completion of the educational program, the rate increased to 92% (119/129) and 98% (104/106) at assessment points 2 and 3, respectively (p = 0.005). The NRS was applied most frequently (46%, 39%, and 51% of patients at assessment points 1, 2, and 3, respectively), followed by the BPS (24%, 24%, and 40% of patients). The critical-care pain observation tool was only used by one UK center, which recruited patients at assessment points 1 and 2, but not 3 (Table 2, Fig. 2c, Fig. S1b).
At assessment point 1, 55% (107/195) of patients received all PAD assessments (pain, sedation, and delirium) at least once per day. Six weeks after completion of the educational program, 53% (68/129) of patients received all PAD assessments, which increased to 73% (77/106) at 1 year (p = 0.003; Table 2, Fig. 2d, Fig. S1d, Fig. S2). As shown in Fig. S1, centers started at different assessment rates for all PAD assessments, and while some centers improved, others stayed the same or worsened.
Determinants of Delirium, Pain, and Sedation Assessment
Multivariable mixed-effects logistic regression revealed that patients were more than twice as likely to receive delirium screening 1 year after the educational program (odds ratio [OR] 2.138, 95% confidence interval [CI] 1.206–3.790; p = 0.009) compared with before. Mechanical ventilation (OR 0.266, 95% CI 0.147–0.481; p < 0.001) or male sex (OR 0.635, 95% CI 0.404–0.997; p = 0.049) lowered the likelihood to receive delirium screening in our adjusted model. Compared with before, patients were more than twice as likely to receive nonpharmacological measures for delirium treatment or prevention 6 weeks after the educational program (OR 2.751, 95% CI 1.592–4.753; p < 0.001), and almost 10 times as likely 1 year after the educational program (OR 9.943, 95% CI 4.436–22.282; p < 0.001). The odds for sedation assessment were four times higher 1 year after the educational program (OR 4.131, 95% CI 1.372–12.438; p = 0.012) compared with before. Mechanical ventilation further increased the odds for sedation assessment (OR 5.684, 95% CI 2.765–11.683; p < 0.001). Almost all patients (98%) received pain assessment 1 year after the educational program. Finally, patients were more than two times more likely to receive all PAD assessments after 1 year (OR 2.295, 95% CI 1.349–3.903; p = 0.002) compared with before (Table 3).
In sensitivity analyses, we first excluded two centers that only recruited patients at assessment point 1 from the analysis. This reduced the screening rate of delirium, pain, sedation, and all PAD assessments for assessment period 1, and resulted in increased effects observed in the multivariable regression (Tables S2 and S3). Second, we excluded four centers that did not recruit at all assessment points from the analysis. This resulted in increased odds of a sedation and complete PAD assessment at assessment point 3, but the significant association of assessment point 3 with the odds of a delirium screening disappeared. Yet, assessment point 2 was newly associated with higher odds of a pain and complete PAD assessment (Tables S4 and S5).
Discussion
In this prospective before-after trial, we examined PAD assessment rates among patients of 12 European ICUs before and after the implementation of a structured educational intervention. About two thirds of patients were screened for delirium at baseline (64%) and 6 weeks after the educational program (65%), which increased to 77% after 1 year. Further, before the intervention, 55% of patients received a complete PAD assessment, which increased to almost three quarters (73%) 1 year after the intervention. Multivariable regression revealed that patients were more than twice as likely to receive a complete PAD assessment 1 year after the educational program.
PAD assessment rates in routine ICU care have been analyzed in previous studies. A study on ABCDEF (Awakening and Breathing Coordination, Delirium monitoring/management, Early exercise/mobility, Family engagement) bundle implementation among critically ill patients with Covid-19 found pain, sedation, and delirium assessment rates of 45%, 52%, and 35%, respectively [43]. These rates are much lower compared to the third assessment point in our study, which fell in the Covid-19 pandemic. However, contrary to our study, participating ICUs did not undergo a structured training, and they only included patients with Covid-19. Because of isolation and preventive measures, PAD assessment and mobilization may have been more difficult for patients with Covid-19 than for patients without Covid-19. In a recent international survey, 85.4% of the 1474 intensivists reported using sedation scales [23]. Just like in our study, the RASS was the commonest. Almost all intensivists (95.4%) reported assessing patients for delirium at least once per day [23], which is contrary to our measured findings and may be indicative of a discrepancy between surveys among ICU staff and real-world point-prevalence studies. In another point-prevalence estimation among a convenience sample of European ICU patients in 2011, more than half (57%) of the 868 patients were not assessed for pain or sedation depth on the study day [24], and almost three quarters (73.1%) were not screened for delirium with a validated instrument. Those rates are below the baseline assessment rates found in our study, where almost nine of ten patients received a pain and/or sedation assessment and 64% were screened for delirium. Another survey among 165 Polish ICUs from 2016 showed that only 10.9% of ICUs monitored delirium and 46.1% reported using sedation scales [25]. The sedation scale most used was the Ramsey scale, and delirium was most commonly identified using the International Classification of Diseases, 10th revision, whereas in our study, the RASS and CAM-ICU were most used [25]. In another survey among 214 ICUs in the UK in 2013/14, 57% of ICUs reported having a sedation protocol, 69.7% reported daily delirium screening, and 93.4% reported routine application of sedation scales [44], which appears consistent with our findings.
We found at 1 year after the educational program, PAD assessment rates significantly improved compared with baseline, with no effect seen at 6 weeks. These findings are consistent with a study conducted among three ICUs of one German hospital, which were subject to similar PAD training consisting of lectures, educational material, and tailored bedside teaching [38]. Similar to our study, their reported frequency of daily PAD monitoring significantly increased more than a year after the training [38]. In contrast to our study, they observed already improvements about 4 weeks after the training. However, their training was twice as long, they had a permanent on-site support team, and they trained all ICU staff instead of using a train-the-trainer concept. The observed delay in improvement in our study could possibly be explained by the train-the-trainer concept and the organizational nature of an ICU, as more than 6 weeks are likely required for the trainer to have sufficient face-to-face time with other staff members to disseminate and implement the content. This explanation is supported by reports on the challenges of changing routine actions and putting new evidence into practice [45]. Our results appear even more noteworthy considering that the third assessment point coincided with the Covid-19 pandemic, which put pressure on already constrained ICU resources. In the absence of the Covid-19 pandemic, we might have observed a stronger increase in PAD assessment rates. Alternatively, the Covid-19 pandemic may have prompted hospitals to focus more on intensive care practice.
PAD assessment is the important first step of adequate pain control, sedation management and delirium prevention, which is known to improve patient outcomes. Systematic pain and sedation assessments three times per day and after painful procedures have been shown to decrease the incidence of severe pain, the duration of mechanical ventilation, and nosocomial infections on a surgical ICU [7]. In a single-center study, an educational intervention using lectures and posters was used to implement an updated protocol mandating documented sedation assessment every 4 h, documented delirium assessment twice daily, and protocolized sedative dose reductions for patients with RASS − 2 or − 3 [46]. After implementation, patients had increased PAD assessment rates, reduced excess sedation, shorter mechanical ventilation, reduced ICU and hospital lengths of stay, and a lower risk of developing delirium [46]. High-quality PAD assessment and management should be part of a broader bundled quality improvement approach such as the ABCDE bundle. Rigorous application of the ABCDE bundle was shown to be associated with lower odds of delirium, more time breathing without mechanical assistance, and a greater likelihood of mobilization [47]. Interestingly, with increasing delirium screening rates, we observed a decline in positive delirium screenings from 26% at assessment point 1 to 13% at assessment point 3. This may indicate that 1 year after the training, a broad cohort of patients received a validated screening, and not only those patients appearing conspicuous of having delirium. Additionally, the higher rate of patients who received nonpharmacological measures to prevent or treat delirium 1 year after the intervention may have reduced the delirium incidence.
The strengths of this study include the international multicenter study design in a distinct geographical region. This enabled us to capture a range of PAD management practices in Europe. Patients were recruited prospectively, and patients treated on a particular day and ICU were enrolled. This should reduce the selection bias inherent to previous studies of routine PAD assessment that used cross-sectional surveys and convenience sampling [24, 27,28,29]. However, our findings come with limitations. Our before-after trial design does not allow for causal inferences on the effects of the educational program as external effects between time points one and three cannot be excluded. That is, we may have detected a general trend of improved PAD assessments or improved documentation over time, independent from our educational program. Further, we considered PAD assessments documented in the medical records. However, patients may have been assessed without documentation, although documentation is part of a complete formal assessment. Also, we did not collect longitudinal data on PAD management in patients throughout their ICU stay, but rather captured three cross-sectional time points. The train-the-trainer concept may have impeded penetration of the educational program, especially because we did not track how many training participants worked in the respective ICU at the 1-year follow-up. In addition, we observed a discrepancy between ICU bed capacity and patient enrollment in many centers, but it is uncertain if these ICUs were running below capacity on the assessment days or if some patients were not enrolled. Furthermore, we determined the rate of patients receiving PAD assessment, but an analysis of the quality or accuracy of these assessments and changes in PAD therapy, outcomes, or adverse events was beyond our study’s scope. Two centers ceased recruiting for the second assessment point and another two centers ceased recruiting at the third assessment point due to the onset of the Covid-19 pandemic in March 2020. In response, we conducted sensitivity analyses where we excluded the center dropouts to exclude the attrition bias. Finally, baseline delirium assessment rates were higher than we had anticipated based on previous literature. This may be due to improvements in delirium screening over time or may suggest that included centers already had above-average delirium screening rates.
Conclusions
In routine care, only about half of included ICU patients received a complete PAD assessment. Six weeks after a PAD educational program, we observed no significant improvement of PAD assessment rates, but a significant improvement 1 year after the educational program. The instruments most frequently used were the CAM-ICU for delirium, the RASS for sedation, and either the NRS or BPS for pain. Notably, at 6 weeks and at 1 year after the educational program, significantly more patients received nonpharmacological measures to prevent or treat delirium. Future randomized cohort studies should analyze the time lag of educational programs to cause behavioral changes and confirm that educational programs effectively improve PAD assessment rates.
References
Chanques G, Sebbane M, Barbotte E, et al. A prospective study of pain at rest: incidence and characteristics of an unrecognized symptom in surgical and trauma versus medical intensive care unit patients. Anesthesiology. 2007;107(5):858–60.
Desbiens NA, Wu AW, Broste SK, et al. Pain and satisfaction with pain control in seriously ill hospitalized adults: findings from the SUPPORT research investigations. Crit Care Med. 1996;24(12):1953–61.
Fraser GL, Prato BS, Riker RR, Berthiaume D, Wilkins ML. Frequency, severity, and treatment of agitation in young versus elderly patients in the ICU. Pharmacotherapy. 2000;20(1):75–82.
Balzer F, Weiß B, Kumpf O, et al. Early deep sedation is associated with decreased in-hospital and two-year follow-up survival. Crit Care. 2015;19(1):197.
Ely EW, Shintani A, Truman B, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004;291(14):1753–62.
Mehta S, Cook D, Devlin JW, et al. Prevalence, risk factors, and outcomes of delirium in mechanically ventilated adults*. Crit Care Med. 2015;43(3):557–66.
Chanques G, Jaber S, Barbotte E, et al. Impact of systematic evaluation of pain and agitation in an intensive care unit*. Crit Care Med. 2006;34(6):1691–9.
Shehabi Y, Bellomo R, Reade MC, et al. Early intensive care sedation predicts long-term mortality in ventilated critically ill patients. Am J Respir Crit Care Med. 2012;186(8):724–31.
Ely E, Gautam S, Margolin R, et al. The impact of delirium in the intensive care unit on hospital length of stay. Intensive Care Med. 2001;27(12):1892–900.
Luetz A, Weiss B, Boettcher S, et al. Routine delirium monitoring is independently associated with a reduction of hospital mortality in critically ill surgical patients: a prospective, observational cohort study. J Crit Care. 2016;35:168–73.
Goldberg TE, Chen C, Wang Y, et al. Association of delirium with long-term cognitive decline: a meta-analysis. JAMA Neurol. 2020;77(11):1373–81.
Devlin J, Skrobik Y, Gélinas C, et al. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med. 2018;46(9):e825–73.
Baron R, Binder A, Biniek R, et al. Evidence and consensus based guideline for the management of delirium, analgesia, and sedation in intensive care medicine. Revision 2015 (DAS-guideline 2015)—short version. GMS German Med Sci. 2015;13:Doc19.
Barr J, Fraser GL, Puntillo K, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013;41(1):263–306.
Chanques G, Viel E, Constantin J-M, et al. The measurement of pain in intensive care unit: comparison of 5 self-report intensity scales. Pain. 2010;151(3):711–21.
Payen J-F, Bru O, Bosson J-L, et al. Assessing pain in critically ill sedated patients by using a behavioral pain scale. Crit Care Med. 2001;29(12):2258–63.
Chanques G, Payen J-F, Mercier G, et al. Assessing pain in non-intubated critically ill patients unable to self report: an adaptation of the Behavioral Pain Scale. Intensive Care Med. 2009;35(12):2060.
Gélinas C, Fillion L, Puntillo KA, Viens C, Fortier M. Validation of the critical-care pain observation tool in adult patients. Am J Crit Care. 2006;15(4):420–7.
Ely EW, Margolin R, Francis J, et al. Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Crit Care Med. 2001;29(7):1370–9.
Bergeron N, Dubois MJ, Dumont M, Dial S, Skrobik Y. Intensive Care Delirium Screening Checklist: evaluation of a new screening tool. Intensive Care Med. 2001;27(5):859–64.
Sessler CN, Gosnell MS, Grap MJ, et al. The Richmond Agitation-Sedation Scale. Am J Respir Crit Care Med. 2002;166(10):1338–44.
Riker RR, Picard JT, Fraser GL. Prospective evaluation of the Sedation-Agitation Scale for adult critically ill patients. Crit Care Med. 1999;27(7):1325–9.
Luz M, Brandão Barreto B, de Castro REV, et al. Practices in sedation, analgesia, mobilization, delirium, and sleep deprivation in adult intensive care units (SAMDS-ICU): an international survey before and during the COVID-19 pandemic. Ann Intensive Care. 2022;12(1):9.
Luetz A, Balzer F, Radtke FM, et al. Delirium, sedation and analgesia in the intensive care unit: a multinational, two-part survey among intensivists. PLoS ONE. 2014;9(11):e110935.
Kotfis K, Zegan-Barańska M, Żukowski M, et al. Multicenter assessment of sedation and delirium practices in the intensive care units in Poland—Is this common practice in Eastern Europe? BMC Anesthesiol. 2017;17(1):120.
Sneyers B, Laterre P-F, Perreault MM, Wouters D, Spinewine A. Current practices and barriers impairing physicians’ and nurses’ adherence to analgo-sedation recommendations in the intensive care unit—a national survey. Crit Care. 2014;18(6):655.
O’Connor M, Bucknall T, Manias E. Sedation management in Australian and New Zealand intensive care units: doctors’ and nurses’ practices and opinions. Am J Crit Care. 2010;19(3):285–95.
Mehta S, Burry L, Fischer S, et al. Canadian survey of the use of sedatives, analgesics, and neuromuscular blocking agents in critically ill patients*. Crit Care Med. 2006;34(2):374–80.
Martin J, Parsch A, Franck M, et al. Practice of sedation and analgesia in German intensive care units: results of a national survey. Crit Care. 2005;9(2):R117.
Lee SY, Fisher J, Wand APF, et al. Developing delirium best practice: a systematic review of education interventions for healthcare professionals working in inpatient settings. Eur Geriatr Med. 2020;11(1):1–32.
Balas MC, Burke WJ, Gannon D, et al. Implementing the ABCDE bundle into everyday care: opportunities, challenges, and lessons learned for implementing the ICU Pain, Agitation, and Delirium guidelines. Crit Care Med. 2013;41(9):S116–27.
Gesin G, Russell BB, Lin AP, et al. Impact of a delirium screening tool and multifaceted education on nurses’ knowledge of delirium and ability to evaluate it correctly. Am J Crit Care. 2012;21(1):e1–11.
Devlin JW, Fong JJ, Schumaker G, et al. Use of a validated delirium assessment tool improves the ability of physicians to identify delirium in medical intensive care unit patients. Crit Care Med. 2007;35(12):2721–4.
Hickin SL, White S, Knopp-Sihota J. Nurses’ knowledge and perception of delirium screening and assessment in the intensive care unit: long-term effectiveness of an education-based knowledge translation intervention. Intensive Crit Care Nurs. 2017;41:43–9.
Mistraletti G, Umbrello M, Anania S, et al. Neurological assessment with validated tools in general ICU: multicenter, randomized, before and after, pragmatic study to evaluate the effectiveness of an e-learning platform for continuous medical education. Minerva Anestesiol. 2017;83(2):145–54.
Swan JT. Decreasing inappropriate unable-to-assess ratings for the Confusion Assessment Method for the Intensive Care Unit. Am J Crit Care. 2014;23(1):60–9.
Sinvani L, Delle Site C, Laumenede T, et al. Improving delirium detection in intensive care units: multicomponent education and training program. J Am Geriatr Soc. 2021;69(11):3249–57.
Radtke FM, Heymann A, Franck M, et al. How to implement monitoring tools for sedation, pain and delirium in the intensive care unit: an experimental cohort study. Intensive Care Med. 2012;38(12):1974–81.
Rosenthal M, Paul N, Grunow JJ, et al. Comparing routine with expert delirium screening in critically ill patients: a secondary analysis of data from the prospective, multicenter EuMAS study (abstract at ESICM LIVES, 22–26 October 2022, Paris, France). Intensive Care Med Exp. 2022;10(supplement 2):39.
Paul N, Grunow JJ, Rosenthal M, et al. Perceived vs. observed adherence to delirium screening: a secondary analysis of data from the prospective, multicenter EuMAS study (abstract at ESICM LIVES, 22–26 October 2022, Paris, France). Intensive Care Med Exp. 2022;10(supplement 2):39.
Grunow JJ, Paul N, Rosenthal M, et al. Mobilization practice in European ICUs and the impact of a structured sedation, analgesia and delirium training: a secondary analysis of data from the prospective, multicenter EuMAS study (abstract at ESICM LIVES, 22–26 October 2022, Paris, France). Intensive Care Med Exp. 2022;10(supplement 2):39.
Carrothers KM, Barr J, Spurlock B, et al. Contextual issues influencing implementation and outcomes associated with an integrated approach to managing pain, agitation, and delirium in adult ICUs. Crit Care Med. 2013;41(9):S128–35.
Liu K, Nakamura K, Katsukawa H, et al. ABCDEF bundle and supportive ICU practices for patients with coronavirus disease 2019 infection: an international point prevalence study. Crit Care Explor. 2021;3(3):1–16.
Richards-Belle A, Canter RR, Power GS, et al. National survey and point prevalence study of sedation practice in UK critical care. Critical Care. 2016;20(1):355.
Green LW. Making research relevant: If it is an evidence-based practice, where’s the practice-based evidence? Fam Pract. 2008;25(suppl_1):i20–4.
Dale CR, Kannas DA, Fan VS, et al. Improved analgesia, sedation, and delirium protocol associated with decreased duration of delirium and mechanical ventilation. Ann Am Thorac Soc. 2014;11(3):367–74.
Balas MC, Vasilevskis EE, Olsen KM, et al. Effectiveness and safety of the awakening and breathing coordination, delirium monitoring/management, and early exercise/mobility bundle. Crit Care Med. 2014;42(5):1024–36.
Acknowledgments
The authors thank the staff of the intensive care units for their valuable time and dedication. JJG is participant of the Berlin Institute of Health Charité Junior Clinician Scientist Program funded by the Charité – Universitätsmedizin Berlin and the Berlin Institute of Health.
Funding
Open Access funding enabled and organized by Projekt DEAL. The study was funded by the European Society of Intensive Care Medicine with one of their NEXT Start-up Grant Awards. The study received support from the National Institute for Health and Care Research (NIHR) Clinical Research Network as a study adopted onto the NIHR Research Portfolio. This means that National Health Service research nurse time was funded via NIHR and it received infrastructure support from the NIHR. Neither did the funding bodies have a role in the design of the study nor in the collection, analysis, and interpretation of data or in writing of the article.
Author information
Authors and Affiliations
Contributions
Conceptualization, BW, MR, and JJG; methodology, BW, MR, NP, and JJG; validation, MR, JJG, and NP; formal analysis, NP; investigation, MR, JJG, VJP, JH, BP, AR, RvH, UP, CS, CW, PS, EL, MS, DC, AT, and BW; resources, CDS, BW; data curation, MR, JJG, and NP; writing—original draft preparation, NP; writing—review and editing, JJG, MR, CDS, VJP, JH, BP, AR, RvH, UP, CS, CW, PS, EL, MS, SKP, DC, AT, and BW; visualization, NP; supervision, CDS; project administration, BW; funding acquisition, BW. All authors have read and agreed to the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
NP, JJG, MR, JH, BP, AR, UP, CS, PS, EL, and DC report no conflicts of interest. Outside the submitted work, CDS reports grants from Deutsche Forschungsgemeinschaft/German Research Society, grants from Deutsches Zentrum für Luft- und Raumfahrt e. V. (DLR)/German Aerospace Center, grants from Einstein Stiftung Berlin/Einstein Foundation Berlin, grants from Gemeinsamer Bundesausschuss/Federal Joint Committee (G-BA), grants from Inneruniversitäre Forschungsförderung/Inner University Grants, grants from Projektträger im DLR/Project Management Agency, grants from Stifterverband/Nonprofit Society Promoting Science and Education, grants from European Society of Anaesthesiology and Intensive Care, grants from BMWI (Federal Ministry for Economic Affairs and Climate Action), grants from Baxter Deutschland GmbH, grants from Cytosorbents Europe GmbH, grants from Edwards Lifesciences Germany GmbH, grants from Fresenius Medical Care, grants from Grünenthal GmbH, grants from Masimo Europe Ltd., grants from Pfizer Pharma PFE GmbH, personal fees from Georg Thieme Verlag, grants from Dr. F. Köhler Chemie GmbH, grants from Sintetica GmbH, grants from Stifterverband für die deutsche Wissenschaft e.V./Philips, grants from Stiftung Charité, grants from AGUETTANT Deutschland GmbH, grants from AbbVie Deutschland GmbH & Co. KG, grants from Amomed Pharma GmbH, grants from InTouch Health, grants from Copra System GmbH, grants from Correvio GmbH, grants from Drägerwerk AG & Co. KGaA, grants from Gemeinsamer Bundesausschuss/Federal Joint Committee (G-BA) – Innovationsfonds, grants from Max-Planck-Gesellschaft zur Förderung der Wissenschaften e.V., grants from Deutsche Gesellschaft für Anästhesiologie & Intensivmedizin (DGAI), grants from Stifterverband für die deutsche Wissenschaft e.V./Metronic, grants from Philips ElectronicsNederland BV, grants from BMBF – Federal Ministry of Education and Research, grants from BMBF/RKI, grants from Deutsche Forschungsgemeinschaft/German Research Society; in addition, CDS has a patent 15753 627.7 issued (Europe), a patent PCT/EP 2015/067731 issued (US), a patent 3 174 588 issued (Europe), a patent 10 2014 215 211.9 licensed, a patent 10 2018 114 364.8 licensed, a patent 10 2018 110 275.5 licensed, a patent 50 2015 010 534.8 licensed, a patent 50 2015 010 347.7 licensed, and a patent 10 2014 215 212.7 licensed; in addition, CDS reports a leadership role at AWMF (Association of the Scientific Medical Societies in Germany), a leadership role at Deutsche Forschungsgemeinschaft (German Research Foundation) review boards, and a leadership role at Deutsche Akademie der Naturforscher Leopoldina e.V. (German National Academy of Sciences – Leopoldina). Outside the submitted work, VJP reports a project grant from Alzheimers Society UK. Outside the submitted work, RvH reports speaker fees from OrionPharma. Outside the submitted work, CW reports fees for patient recruitment as investigator of the Sedaconda study SED001, honoraria for a presentation on a symposium for Sedana medical AB, honoraria as board member of Digimed GmbH (quality insurance software), a leadership role as editor of the journal “Notfall + Rettungsmedizin,” and a leadership role as a member of the board of directors of the DIVI (German Association of Intensive Care Medicine). Outside the submitted work, MS reports grants from Edwards Lifescience, grants from Medtronic, personal fees from Georg Thieme Verlag, honoraria from Edwards Lifescience, honoraria from BTG, honoraria from OrionPharma, a leadership role as president of MJC Intensivmedizin UEMS, a leadership role as German representative of the European Board of Anesthesiology/Section Anesthesiology of the UEMS, a member role of the ICU Subcom of ESAIC, a leadership role as corresponding author of S3-Leitlinie für die Intensivmedizin bei herzchirurgischen Patienten: Hämodynamisches Monitoring und kardiopulmonales System, and a leadership role as Schriftführer Arbeitskreis Kardioanästhesie der DGAI. Outside the submitted work, SKP reports participation on a data safety monitoring board for study German Clinical Trial Register DRKS 00021256, prospectively registered on 24.04.2020. Outside the submitted work, AT received consultation honoraria from Argenx and is a member of the medical advisory board of the German Myasthenia Society. BW reports a NEXT Start-up Grant from the European Society of Intensive Care Medicine (ESICM) related to the study; outside the submitted work, BW reports grants from Gemeinsamer Bundesausschuss / Federal Joint Committee (G-BA)—Innovationsfonds, consulting fees from OrionPharma, honoraria from Dr. F. Köhler Chemie, support for attending meetings and travel from Teladoc Health, a leadership role as ESICM NEXT Chair, a member role in the ESICM ARDS Guideline group, and a member role in the Covriin-Group of the Robert Koch Institute.
Ethical Approval/Informed Consent
The study adhered to the ethical standards of the Declaration of Helsinki and its later amendments. Ethical approval at the coordinating study site was granted by the Institutional Review Board (IRB) of Charité–Universitätsmedizin Berlin (EA2/022/18) on March 23, 2018. Participating centers obtained IRB approval before study commencement as required by local regulations. Written consent or a waiver was subject to the decision of the local IRBs.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Paul, N., Grunow, J.J., Rosenthal, M. et al. Enhancing European Management of Analgesia, Sedation, and Delirium: A Multinational, Prospective, Interventional Before-After Trial. Neurocrit Care (2023). https://doi.org/10.1007/s12028-023-01837-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12028-023-01837-8