Abstract
Background
Blood pressure variability (BPV) has emerged as a significant factor associated with clinical outcomes after intracerebral hemorrhage (ICH). Although hematoma expansion (HE) is associated with clinical outcomes, the relationship between BPV that encompasses prehospital data and HE is unknown. We hypothesized that BPV was positively associated with HE.
Methods
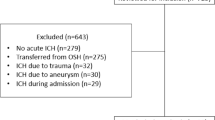
We analyzed 268 patients with primary ICH enrolled in the National Institutes of Health-funded Field Administration of Stroke Therapy-Magnesium (FAST-MAG) study who received head computed tomography or magnetic resonance imaging on arrival to the emergency department (ED) and repeat imaging within 6–48 h. BPV was calculated by standard deviation (SD) and coefficient of variation (CV) from prehospital data as well as systolic blood pressure (SBP) measurements taken on ED arrival, 15 min post antihypertensive infusion start, 1 h post maintenance infusion start, and 4 h after ED arrival. HE was defined by hematoma volume expansion increase > 6 mL or by 33%. Univariate logistic regression was used for presence of HE in quintiles of SD and CV of SBP for demographics and clinical characteristics.
Results
Of the 268 patients analyzed from the FAST-MAG study, 116 (43%) had HE. Proportions of patients with HE were not statistically significant in the higher quintiles of the SD and CV of SBP for either the hyperacute or the acute period. Presence of HE was significantly more common in patients on anticoagulation.
Conclusions
Higher BPV was not found to be associated with occurrence of HE in the hyperacute or the acute period of spontaneous ICH. Further study is needed to determine the relationship.






Similar content being viewed by others
References
Diedler J, Sykora M, Rupp A, Poli S, Karpel-Massler G, Sakowitz O, Steiner T. Impaired cerebral vasomotor activity in spontaneous intracerebral hemorrhage. Stroke. 2009;40:815–9. https://doi.org/10.1161/STROKEAHA.108.531020.
Rodriguez-Luna D, Piñeiro S, Rubiera M, Ribo M, Coscojuela P, Pagola J, Flores A, Muchada M, Ibarra B, Meler P, et al. Impact of blood pressure changes and course on hematoma growth in acute intracerebral hemorrhage. Eur J Neurol. 2013;20:1277–83. https://doi.org/10.1111/ene.12180.
Vaughan Sarrazin M, Limaye K, Samaniego EA, Al Kasab S, Sheharyar A, Dandapat S, Guerrero WR, Hasan DM, Ortega-Gutierrez S, Derdeyn CP, et al. Disparities in Inter-hospital helicopter transportation for hispanics by geographic region: a threat to fairness in the era of thrombectomy. J Stroke Cerebrovasc Dis. 2019;28:550–6. https://doi.org/10.1016/j.jstrokecerebrovasdis.2018.10.031.
Leira R, Dávalos A, Silva Y, Gil-Peralta A, Tejada J, Garcia M, Castillo J. Stroke Project. CrDGotSNS Early neurologic deterioration in intracerebral hemorrhage: predictors and associated factors. Neurology. 2004;63:461–7. https://doi.org/10.1212/01.wnl.0000133204.81153.ac.
Ohwaki K, Yano E, Nagashima H, Hirata M, Nakagomi T, Tamura A. Blood pressure management in acute intracerebral hemorrhage: relationship between elevated blood pressure and hematoma enlargement. Stroke. 2004;35:1364–7. https://doi.org/10.1161/01.STR.0000128795.38283.4b.
Anderson CS, Heeley E, Huang Y, Wang J, Stapf C, Delcourt C, Lindley R, Robinson T, Lavados P, Neal B, et al. Rapid blood-pressure lowering in patients with acute intracerebral hemorrhage. N Engl J Med. 2013;368:2355–65. https://doi.org/10.1056/NEJMoa1214609.
Kazui S, Minematsu K, Yamamoto H, Sawada T, Yamaguchi T. Predisposing factors to enlargement of spontaneous intracerebral hematoma. Stroke. 1997;28:2370–5. https://doi.org/10.1161/01.str.28.12.2370.
Qureshi AI, Palesch YY, Barsan WG, Hanley DF, Hsu CY, Martin RL, Moy CS, Silbergleit R, Steiner T, Suarez JI, et al. Intensive blood-pressure lowering in patients with acute cerebral hemorrhage. N Engl J Med. 2016;375:1033–43. https://doi.org/10.1056/NEJMoa1603460.
Moullaali TJ, Wang X, Martin RH, Shipes VB, Robinson TG, Chalmers J, Suarez JI, Qureshi AI, Palesch YY, Anderson CS. Blood pressure control and clinical outcomes in acute intracerebral haemorrhage: a preplanned pooled analysis of individual participant data. Lancet Neurol. 2019;18:857–64. https://doi.org/10.1016/S1474-4422(19)30196-6.
Carcel C, Wang X, Sato S, Stapf C, Sandset EC, Delcourt C, Arima H, Robinson T, Lavados P, Chalmers J, et al. Degree and timing of intensive blood pressure lowering on hematoma growth in intracerebral hemorrhage: intensive blood pressure reduction in acute cerebral hemorrhage trial-2 results. Stroke. 2016;47:1651–3. https://doi.org/10.1161/STROKEAHA.116.013326.
Chung PW, Kim JT, Sanossian N, Starkmann S, Hamilton S, Gornbein J, Conwit R, Eckstein M, Pratt F, Stratton S, et al. Association between hyperacute stage blood pressure variability and outcome in patients with spontaneous intracerebral hemorrhage. Stroke. 2018;49:348–54. https://doi.org/10.1161/strokeaha.117.017701.
Shkirkova K, Saver JL, Starkman S, Wong G, Weng J, Hamilton S, Liebeskind DS, Eckstein M, Stratton S, Pratt F, et al. Frequency, predictors, and outcomes of prehospital and early postarrival neurological deterioration in acute stroke: exploratory analysis of the FAST-MAG randomized clinical trial. JAMA Neurol. 2018;75:1364–74. https://doi.org/10.1001/jamaneurol.2018.1893.
Manning L, Hirakawa Y, Arima H, Wang X, Chalmers J, Wang J, Lindley R, Heeley E, Delcourt C, Neal B, et al. Blood pressure variability and outcome after acute intracerebral haemorrhage: a post-hoc analysis of INTERACT2, a randomised controlled trial. Lancet Neurol. 2014;13:364–73. https://doi.org/10.1016/S1474-4422(14)70018-3.
Meeks JR, Bambhroliya AB, Meyer EG, Slaughter KB, Fraher CJ, Sharrief AZ, Bowry R, Ahmed WO, Tyson JE, Miller CC, et al. High in-hospital blood pressure variability and severe disability or death in primary intracerebral hemorrhage patients. Int J Stroke. 2019;14:987–95. https://doi.org/10.1177/1747493019827763.
Lattanzi S, Cagnetti C, Provinciali L, Silvestrini M. Blood pressure variability and clinical outcome in patients with acute intracerebral hemorrhage. J Stroke Cerebrovasc Dis. 2015;24:1493–9. https://doi.org/10.1016/j.jstrokecerebrovasdis.2015.03.014.
Divani AA, Liu X, Di Napoli M, Lattanzi S, Ziai W, James ML, Jafarli A, Jafari M, Saver JL, Hemphill JC, et al. Blood pressure variability predicts poor in-hospital outcome in spontaneous intracerebral hemorrhage. Stroke. 2019;50:2023–9. https://doi.org/10.1161/STROKEAHA.119.025514.
de Havenon A, Majersik JJ, Stoddard G, Wong KH, McNally JS, Smith AG, Rost NS, Tirschwell DL. Increased blood pressure variability contributes to worse outcome after intracerebral hemorrhage. Stroke. 2018;49:1981–4. https://doi.org/10.1161/STROKEAHA.118.022133.
Tanaka E, Koga M, Kobayashi J, Kario K, Kamiyama K, Furui E, Shiokawa Y, Hasegawa Y, Okuda S, Todo K, et al. Blood pressure variability on antihypertensive therapy in acute intracerebral hemorrhage: the stroke acute management with urgent risk-factor assessment and improvement-intracerebral hemorrhage study. Stroke. 2014;45:2275–9. https://doi.org/10.1161/STROKEAHA.114.005420.
Jeon JP, Kim C, Kim SE. Blood pressure variability and outcome in patients with acute nonlobar intracerebral hemorrhage following intensive antihypertensive treatment. Chin Med J (Engl). 2018;131:657–64. https://doi.org/10.4103/0366-6999.226886.
Jauch EC, Lindsell CJ, Adeoye O, Khoury J, Barsan W, Broderick J, Pancioli A, Brott T. Lack of evidence for an association between hemodynamic variables and hematoma growth in spontaneous intracerebral hemorrhage. Stroke. 2006;37:2061–5. https://doi.org/10.1161/01.STR.0000229878.93759.a2.
Andalib S, Lattanzi S, Di Napoli M, Petersen A, Biller J, Kulik T, Macri E, Girotra T, Torbey MT, Divani AA. Blood pressure variability: a new predicting factor for clinical outcomes of intracerebral hemorrhage. J Stroke Cerebrovasc Dis. 2020;29: 105340. https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.105340.
Saver JL, Starkman S, Eckstein M, Stratton S, Pratt F, Hamilton S, Conwit R, Liebeskind DS, Sung G, Sanossian N, et al. Methodology of the field administration of stroke therapy—magnesium (FAST-MAG) phase 3 trial: part 1—rationale and general methods. Int J Stroke. 2014;9:215–9. https://doi.org/10.1111/ijs.12243.
Naidech AM, Shkirkova K, Villablanca JP, Sanossian N, Liebeskind DS, Sharma L, Eckstein M, Stratton S, Conwit R, Hamilton S, et al. Magnesium sulfate and hematoma expansion: an ancillary analysis of the FAST-MAG randomized trial. Stroke. 2022;53:1516–9. https://doi.org/10.1161/STROKEAHA.121.037999.
Funding
This work was supported by grants UL1TR001855 and UL1TR000130 from the National Center for Advancing Translational Science of the U.S. National Institutes of Health (to MW). This work was also supported by grant UL1TR001855 from the Southern California Clinical and Translational Science Institute (to RAP). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Southern California Clinical and Translational Science Institute.
Author information
Authors and Affiliations
Contributions
DMO writing manuscript draft, critical revision, interpretation of data. KS key statistical analysis, study design, statistical methodology, data analysis. RAP writing manuscript, review and editing, critical revision, interpretation of data. PWC conducted investigation for evidence analysis, provided analytic resources. JLS study design, methodology, and project administration in the original study. SS substantial contribution to conception, study design, and methodology in the original study. DSL substantial contribution to conception, study design, and methodology in the original study. SH substantial contribution to conception, statistical methodology, and analysis in the original study. MW performed statistical analysis and writing. NS principal investigator, study conceptualization and design, critical manuscript writing, project administration and supervision.
Corresponding author
Ethics declarations
Conflict of interest
No financial disclosures for DMO, KS, PWC, JLS, SS, SH, and NS. DSL: Consultant as Imaging Core Lab to Cerenovus, Genentech, Medtronic, Stryker, and Rapid Medical.
Ethical approval/informed consent
Informed consent and full institutional review board approval was not required. The secondary analysis falls under the exempt criteria of 45 CFR 46.101 (b) (4) because the study involved existing data, documents, and diagnostic records recorded in an anonymous manner such that the study participants cannot be identified neither directly nor through any identifiers.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Oh, D.M., Shkirkova, K., Poblete, R.A. et al. Association Between Hyperacute Blood Pressure Variability and Hematoma Expansion After Intracerebral Hemorrhage: Secondary Analysis of the FAST-MAG Database. Neurocrit Care 38, 356–364 (2023). https://doi.org/10.1007/s12028-022-01657-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-022-01657-2