Abstract
Background
It is generally believed that hypercapnia and hypocapnia will cause secondary injury to patients with craniocerebral diseases, but a small number of studies have shown that they may have potential benefits. We assessed the impact of partial pressure of arterial carbon dioxide (PaCO2) on in-hospital mortality of patients with craniocerebral diseases. The hypothesis of this research was that there is a nonlinear correlation between PaCO2 and in-hospital mortality in patients with craniocerebral diseases and that mortality rate is the lowest when PaCO2 is in a normal range.
Methods
We identified patients with craniocerebral diseases from Medical Information Mart for Intensive Care third and fourth edition databases. Cox regression analysis and restricted cubic splines were used to examine the association between PaCO2 and in-hospital mortality.
Results
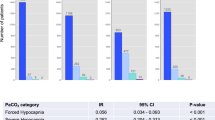
Nine thousand six hundred and sixty patients were identified. A U-shaped association was found between the first 24-h PaCO2 and in-hospital mortality in all participants. The nadir for in-hospital mortality risk was estimated to be at 39.5 mm Hg (p for nonlinearity < 0.001). In the subsequent subgroup analysis, similar results were found in patients with traumatic brain injury, metabolic or toxic encephalopathy, subarachnoid hemorrhage, cerebral infarction, and other encephalopathies. Besides, the mortality risk reached a nadir at PaCO2 in the range of 35–45 mm Hg. The restricted cubic splines showed a U-shaped association between the first 24-h PaCO2 and in-hospital mortality in patients with other intracerebral hemorrhage and cerebral tumor. Nonetheless, nonlinearity tests were not statistically significant. In addition, Cox regression analysis showed that PaCO2 ranging 35–45 mm Hg had the lowest death risk in most patients. For patients with hypoxic-ischemic encephalopathy and intracranial infections, the first 24-h PaCO2 and in-hospital mortality did not seem to be correlated.
Conclusions
Both hypercapnia and hypocapnia are harmful to most patients with craniocerebral diseases. Keeping the first 24-h PaCO2 in the normal range (35–45 mm Hg) is associated with lower death risk.



Similar content being viewed by others
Data Availability
The datasets generated and/or analyzed during the current study are available in the MIMIC-III (https://mimic.physionet.org) & MIMIC-IV (https://mimic-iv.mit.edu) databases.
References
Feigin VL, Vos T, Nichols E, et al. The global burden of neurological disorders: translating evidence into policy. Lancet Neurol. 2020;19(3):255–65.
Feigin VL, Nichols E, Alam T, et al. Global, regional, and national burden of neurological disorders, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18(5):459–80.
Hoiland RL, Fisher JA, Ainslie PN. Regulation of the cerebral circulation by arterial carbon dioxide. Compr Physiol. 2019;9(3):1101–54.
Harper AM, Glass HI. Effect of alterations in the arterial carbon dioxide tension on the blood flow through the cerebral cortex at normal and low arterial blood pressures. J Neurol Neurosurg Psychiatry. 1965;28(5):449–52.
Godoy DA, Rovegno M, Lazaridis C, Badenes R. The effects of arterial CO2 on the injured brain: two faces of the same coin. J Crit Care. 2021;61:207–15.
Kofke WA, Rajagopalan S, Ayubcha D, et al. Defining a taxonomy of intracranial hypertension: is ICP more than just a number? J Neurosurg Anesthesiol. 2020;32(2):120–31.
Schneider AG, Eastwood GM, Bellomo R, et al. Arterial carbon dioxide tension and outcome in patients admitted to the intensive care unit after cardiac arrest. Resuscitation. 2013;84(7):927–34.
Roberts BW, Kilgannon JH, Chansky ME, et al. Association between postresuscitation partial pressure of arterial carbon dioxide and neurological outcome in patients with post-cardiac arrest syndrome. Circulation. 2013;127(21):2107–13.
Davis DP, Idris AH, Sise MJ, et al. Early ventilation and outcome in patients with moderate to severe traumatic brain injury. Crit Care Med. 2006;34(4):1202–8.
Roberts BW, Karagiannis P, Coletta M, et al. Effects of PaCO2 derangements on clinical outcomes after cerebral injury: a systematic review. Resuscitation. 2015;91:32–41.
Reiff T, Barthel O, Schonenberger S, et al. High-normal PaCO2 values might be associated with worse outcome in patients with subarachnoid haemorrhage—a retrospective cohort study. BMC Neurol. 2020;20(1):31.
Johnson AE, Pollard TJ, Shen L, et al. MIMIC-III, a freely accessible critical care database. Sci Data. 2016;3:160035.
Hextrum S, Minhas JS, Liotta EM, et al. Hypocapnia, ischemic lesions, and outcomes after intracerebral hemorrhage. J Neurol Sci. 2020;418:117139.
Godoy DA, Badenes R, Robba C, et al. Hyperventilation in severe traumatic brain injury has something changed in the last decade or uncertainty continues? A brief review. Front Neurol. 2021;12:573237.
Lundberg N. Continuous recording and control of ventricular fluid pressure in neurosurgical practice. Acta Psychiatr Scand Suppl. 1960;36(149):1–193.
Godoy DA, Seifi A, Garza D, et al. Hyperventilation therapy for control of posttraumatic intracranial hypertension. Front Neurol. 2017;8:250.
Neumann JO, Chambers IR, Citerio G, et al. The use of hyperventilation therapy after traumatic brain injury in Europe: an analysis of the BrainIT database. Intensive Care Med. 2008;34(9):1676–82.
Esnault P, Roubin J, Cardinale M, et al. Spontaneous hyperventilation in severe traumatic brain injury: incidence and association with poor neurological outcome. Neurocrit Care. 2018;30(2):405–13.
Marhong J, Fan E. Carbon dioxide in the critically ill: too much or too little of a good thing? Respir Care. 2014;59(10):1597–605.
Forbes ML, Clark RS, Dixon CE, et al. Augmented neuronal death in CA3 hippocampus following hyperventilation early after controlled cortical impact. J Neurosurg. 1998;88(3):549–56.
Marion DW, Puccio A, Wisniewski SR, et al. Effect of hyperventilation on extracellular concentrations of glutamate, lactate, pyruvate, and local cerebral blood flow in patients with severe traumatic brain injury. Crit Care Med. 2002;30(12):2619–25.
Solaiman O, Singh JM. Hypocapnia in aneurysmal subarachnoid hemorrhage: incidence and association with poor clinical outcomes. J Neurosurg Anesthesiol. 2013;25(3):254–61.
Muizelaar J, Marmarou A, Ward J, et al. Adverse effects of prolonged hyperventilation in patients with severe head injury: a randomized clinical trial. J Neurosurgery. 1991;75(5):731–9.
Gelb A, Craen R, Rao G, et al. Does hyperventilation improve operating condition during supratentorial craniotomy? A multicenter randomized crossover trial. Anesthesia Analgesia. 2008;106(2):585–94.
Dodds C. Carbon dioxide and the cerebral circulation. Br J Anaesth. 1999;82(5):813.
van Hulst RA, Hasan D, Lachmann B. Intracranial pressure, brain PCO2, PO2, and pH during hypo- and hyperventilation at constant mean airway pressure in pigs. Intensive Care Med. 2002;28(1):68–73.
Westermaier T, Stetter C, Kunze E, et al. Controlled hypercapnia enhances cerebral blood flow and brain tissue oxygenation after aneurysmal subarachnoid hemorrhage: results of a phase 1 study. Neurocrit Care. 2016;25(2):205–14.
Eastwood GM, Schneider AG, Suzuki S, et al. Targeted therapeutic mild hypercapnia after cardiac arrest: a phase II multi-centre randomised controlled trial (the CCC trial). Resuscitation. 2016;104:83–90.
Hope Kilgannon J, Hunter BR, Puskarich MA, et al. Partial pressure of arterial carbon dioxide after resuscitation from cardiac arrest and neurological outcome: a prospective multi-center protocol-directed cohort study. Resuscitation. 2019;135:212–20.
Vannucci RC, Brucklacher RM, Vannucci SJ. Effect of carbon dioxide on cerebral metabolism during hypoxia-ischemia in the immature rat. Pediatr Res. 1997;42(1):24–9.
Katsura K, Kristian T, Smith ML, et al. Acidosis induced by hypercapnia exaggerates ischemic brain damage. J Cereb Blood Flow Metab. 1994;14(2):243–50.
Paljarvi L, Soderfeldt B, Kalimo H, et al. The brain in extreme respiratory acidosis: a light- and electron-microscopic study in the rat. Acta Neuropathol. 1982;58(2):87–94.
Warner KJ, Cuschieri J, Copass MK, et al. The impact of prehospital ventilation on outcome after severe traumatic brain injury. J Trauma. 2007;62(6):1330–6.
Tiruvoipati R, Pilcher D, Botha J, et al. Association of hypercapnia and hypercapnic acidosis with clinical outcomes in mechanically ventilated patients with cerebral injury. JAMA Neurol. 2018;75(7):818.
Funding
This work was supported by GDPH Scientific Research Funds for Leading Medical Talents and Distinguished Young Scholars in Guangdong Province (KJ012019452) and the Science and Technology Project of Guangzhou (201804010379).
Author information
Authors and Affiliations
Contributions
WJ and MW came up with the study concept. All authors contributed to the study design. GC, XZ, QO, YZ, LH, SC, and HZ collected and analyzed the data. GC, XZ, and QO wrote the first draft of the article and all authors commented on previous versions of the article. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethical Approval/Informed Consent
The study was an analysis of anonymized publicly available databases with preexisting institutional review board approval.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cai, G., Zhang, X., Ou, Q. et al. Optimal Targets of the First 24-h Partial Pressure of Carbon Dioxide in Patients with Cerebral Injury: Data from the MIMIC-III and IV Database. Neurocrit Care 36, 412–420 (2022). https://doi.org/10.1007/s12028-021-01312-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-021-01312-2