Abstract
Background and Purpose
Acute physiologic derangements and multiple organ dysfunction are common after subarachnoid hemorrhage. We aimed to evaluate the simplified acute physiology score 3 (SAPS-3) and the sequential organ failure assessment (SOFA) scores for the prediction of in-hospital mortality in a large multicenter cohort of SAH patients.
Methods
This was a retrospective analysis of prospectively collected data from 45 ICUs in Brazil, during 2014 and 2015. Patients admitted with non-traumatic subarachnoid hemorrhage (SAH) were included. Clinical and outcome data were retrieved from an electronic ICU quality registry. SAPS-3 and SOFA scores, without the neurological components (i.e., nSAPS-3 and nSOFA, respectively) were recorded, as well as the World Federation of Neurological Surgeons (WFNS) scale. We used multilevel logistic regression analysis to identify factors associated with in-hospital mortality. We evaluated performance using the area under the receiver operating characteristic curve (AUROC), as well as calibration belts and precision–recall plots.
Results
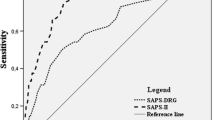
The study included 997 patients, from which 426 (43%) had poor clinical grade (WFNS 4 or 5) and in-hospital mortality was 34%. Median nSAPS-3 and nSOFA score at admission were 46 (IQR: 38–55) and 2 (0–5), respectively. Non-survivors were older, had higher nSAPS-3 and nSOFA, and more often poor grade. After adjustment for age, poor grade and withdrawal of life sustaining therapies, multivariable analysis identified nSAPS-3 and nSOFA score as independent clinical predictors of in-hospital mortality. The AUROC curve that included nSAPS-3 and nSOFA scores significantly improved the already good discrimination and calibration of age and WFNS to predict in-hospital mortality (AUROC: 0.89 for the full final model vs. 0.85 for age and WFNS; P < 0.0001).
Conclusions
nSAPS-3 and nSOFA scores were independently associated with in-hospital mortality after SAH. The addition of these scores improved early prediction of hospital mortality in our cohort and should be integrated to other specific prognostic indices in the early assessment of SAH.


Similar content being viewed by others
References
Rass V, Gaasch M, Kofler M, et al. Systemic inflammatory response syndrome as predictor of poor outcome in nontraumatic subarachnoid hemorrhage patients. Crit Care Med. 2018;46:e1152–9.
Goncalves B, Kurtz P, Turon R, et al. Incidence and impact of sepsis on long-term outcomes after subarachnoid hemorrhage: a prospective observational study. Ann Intensive Care. 2019;9:94.
Claassen J, Bernardini GL, Kreiter K, et al. Effect of cisternal and ventricular blood on risk of delayed cerebral ischemia after subarachnoid hemorrhage: the Fisher scale revisited. Stroke. 2001;32:2012–20.
Claassen J, Vu A, Kreiter KT, et al. Effect of acute physiologic derangements on outcome after subarachnoid hemorrhage. Crit Care Med. 2004;32:832–8.
Kerro A, Woods T, Chang JJ. Neurogenic stunned myocardium in subarachnoid hemorrhage. J Crit Care. 2017;38:27–34.
Basile-Filho A, Lago AF, Menegueti MG, et al. The use of SAPS 3, SOFA, and glasgow coma scale to predict mortality in patients with subarachnoid hemorrhage: A retrospective cohort study. Medicine (Baltimore). 2018;97:e12769.
Soares M, Bozza FA, Angus DC, et al. Organizational characteristics, outcomes, and resource use in 78 Brazilian intensive care units: the ORCHESTRA study. Intensive Care Med. 2015;41:2149–60.
Zampieri FG, Soares M, Borges LP, Salluh JIF, Ranzani OT. The Epimed Monitor ICU Database(R): a cloud-based national registry for adult intensive care unit patients in Brazil. Rev Bras Ter Intensiva. 2017;29:418–26.
Zampieri FG, Iwashyna TJ, Viglianti EM, et al. Association of frailty with short-term outcomes, organ support and resource use in critically ill patients. Intensive Care Med. 2018;44:1512–20.
Saito T, Rehmsmeier M. The precision-recall plot is more informative than the ROC plot when evaluating binary classifiers on imbalanced datasets. PLoS ONE. 2015;10:e0118432.
Finazzi S, Poole D, Luciani D, Cogo PE, Bertolini G. Calibration belt for quality-of-care assessment based on dichotomous outcomes. PLoS ONE. 2011;6:e16110.
Etminan N, Chang HS, Hackenberg K, et al. Worldwide incidence of aneurysmal subarachnoid hemorrhage according to region, time period, blood pressure, and smoking prevalence in the population: a systematic review and meta-analysis. JAMA Neurol. 2019;76:588–97.
Witsch J, Frey HP, Patel S, et al. Prognostication of long-term outcomes after subarachnoid hemorrhage: The FRESH score. Ann Neurol. 2016;80:46–58.
Jaja BNR, Saposnik G, Lingsma HF, et al. Development and validation of outcome prediction models for aneurysmal subarachnoid haemorrhage: the SAHIT multinational cohort study. BMJ. 2018;360:j5745.
Damani R, Mayer S, Dhar R, et al. Common data element for unruptured intracranial aneurysm and subarachnoid hemorrhage: recommendations from assessments and clinical examination workgroup/subcommittee. Neurocrit Care. 2019;30:28–35.
Funding
The present study was funded by institutional departmental funds (IDOR).
Author information
Authors and Affiliations
Contributions
PK conceptualization, data curation, formal analysis, supervision, validation, visualization, roles/writing – original draft, writing – review & editing. FST conceptualization, roles/writing – original draft, writing – review & editing. FAB conceptualization, data curation investigation, methodology, project administration, resources supervision, validation, roles/writing – original draft, writing – review & editing. LSLB data curation, formal analysis methodology, software. CR, BG, RT, MMM, MM, MAF, CN data curation, investigation, writing – review & editing. MS, JIFS conceptualization, data curation, funding acquisition, investigation, methodology, project administration, resources, software, supervision, validation, roles/writing – original draft, writing – review & editing.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Taccone reports other from BD, other from Zoll, other from Nihon Khoden, other from Neuroptics, all outside the submitted work. JIFS and MS are shareholders of Epimed Solutions®, outside of the submitted work. JIFS and MS are partially supported by research grants from National and State funding agencies (CNPq and FAPERJ).
Ethical Approval
The local ethics committee at the D’Or Institute for Research and Education (Approval Number 334.835) and Brazilian National Ethics Committee (CAAE 19687113.8.1001.5249) approved the study and waived need for informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kurtz, P., Taccone, F.S., Bozza, F.A. et al. Systemic Severity and Organ Dysfunction in Subarachnoid Hemorrhage: A Large Retrospective Multicenter Cohort Study. Neurocrit Care 35, 56–61 (2021). https://doi.org/10.1007/s12028-020-01139-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-020-01139-3