Abstract
Background
Delayed cerebral ischemia (DCI) contributes to morbidity following aneurysmal subarachnoid hemorrhage; however, its etiology remains poorly understood. DCI is not only a consequence of angiographic vasospasm, but also involves microthrombosis and neuroinflammation, two events with unexplained phenomenology. The vascular endothelial glycocalyx mediates platelet aggregation and endothelial cell-leukocyte interactions and may play an important role in DCI pathogenesis.
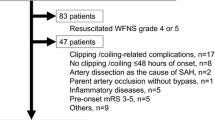
Methods
We present a case series in which we conducted multiplex and singlet enzyme-linked immunosorbent assays of endothelial, glycocalyx, inflammatory, and neuroinjury proteins in both CSF and plasma in three patients during active DCI following SAH. Samples were obtained at baseline following surgical repair of SAH, and again at DCI onset. CSF was sampled at the same time points from in situ external ventricular drains.
Results
DCI was associated with significant elevations of soluble markers of endotheliopathy, including vascular adhesion protein-1, soluble fractions of endothelial cell adhesion molecules (CAMs), procoagulant tissue factor, and specific markers of glycocalyx injury, including syndecan-1, and CD44. These phenomena were also associated with an elevation of both circulating and CSF matrix metalloproteinases, which are known to cleave components of the glycocalyx. Elevation of vascular CAM-1 in the CSF with DCI indicated these events were possibly associated with the breakdown of brain microvasculature integrity.
Conclusions
These preliminary data support the hypothesis that glycocalyx injury occurs in SAH, and might contribute to DCI by regulating cerebral microthrombosis and delayed neuroinflammation.




Similar content being viewed by others
References
Macdonald RL. Delayed neurological deterioration after subarachnoid haemorrhage. Nat Rev Neurol. 2014;10(1):44–58.
Vergouwen MD, Vermeulen M, Coert BA, Stroes ES, Roos YB. Microthrombosis after aneurysmal subarachnoid hemorrhage: an additional explanation for delayed cerebral ischemia. J Cereb Blood Flow Metab. 2008;28(11):1761–70.
Przybycien-Szymanska MM, Yang Y, Ashley WW. Microparticle derived proteins as potential biomarkers for cerebral vasospasm post subarachnoid hemorrhage. A preliminary study. Clin Neurol Neurosurg. 2016;141:48–55.
Provencio JJ. Inflammation in subarachnoid hemorrhage and delayed deterioration associated with vasospasm: a review. Acta neurochir Suppl. 2013;115:233–8.
Miller BA, Turan N, Chau M, Pradilla G. Inflammation, vasospasm, and brain injury after subarachnoid hemorrhage. Biomed Res Int. 2014;2014:384342.
Reitsma S, Slaaf DW, Vink H, van Zandvoort MA, oude Egbrink MG. The endothelial glycocalyx: composition, functions, and visualization. Pflugers Arch. 2007;454(3):345–59.
Becker BF, Jacob M, Leipert S, Salmon AH, Chappell D. Degradation of the endothelial glycocalyx in clinical settings: searching for the sheddases. Br J Clin Pharmacol. 2015;80(3):389–402.
Di Battista AP, Rizoli SB, Lejnieks B, et al. Sympathoadrenal activation is associated with acute traumatic coagulopathy and endotheliopathy in isolated brain injury. Shock. 2016;46(3 Suppl 1):96–103.
Di Battista AP, Rhind SG, Hutchison MG, et al. Inflammatory cytokine and chemokine profiles are associated with patient outcome and the hyperadrenergic state following acute brain injury. J Neuroinflamm. 2016;13:40.
Su G, Blaine SA, Qiao D, Friedl A. Membrane type 1 matrix metalloproteinase-mediated stromal syndecan-1 shedding stimulates breast carcinoma cell proliferation. Cancer Res. 2008;68(22):9558–65.
Manon-Jensen T, Multhaupt HA, Couchman JR. Mapping of matrix metalloproteinase cleavage sites on syndecan-1 and syndecan-4 ectodomains. FEBS J. 2013;280(10):2320–31.
McGirt MJ, Lynch JR, Blessing R, Warner DS, Friedman AH, Laskowitz DT. Serum von Willebrand factor, matrix metalloproteinase-9, and vascular endothelial growth factor levels predict the onset of cerebral vasospasm after aneurysmal subarachnoid hemorrhage. Neurosurgery. 2002;51(5):1128–34 (discussion 1134–5).
Johansson PI, Bergstrom A, Aachmann-Andersen NJ, et al. Effect of acute hypobaric hypoxia on the endothelial glycocalyx and digital reactive hyperemia in humans. Front Physiol. 2014;5:459.
Zeng Y, Tarbell JM. The adaptive remodeling of endothelial glycocalyx in response to fluid shear stress. PLoS ONE. 2014;9(1):e86249.
Xu H, Testai FD, Valyi-Nagy T, et al. VAP-1 blockade prevents subarachnoid hemorrhage-associated cerebrovascular dilating dysfunction via repression of a neutrophil recruitment-related mechanism. Brain Res. 2015;1603:141–9.
Sokol B, Wozniak A, Jankowski R, et al. HMGB1 level in cerebrospinal fluid as a marker of treatment outcome in patients with acute hydrocephalus following aneurysmal subarachnoid hemorrhage. J Stroke Cerebrovasc Dis. 2015;24(8):1897–904.
Zhao XD, Mao HY, Lv J, Lu XJ. Expression of high-mobility group box-1 (HMGB1) in the basilar artery after experimental subarachnoid hemorrhage. J Clin Neurosci. 2016;27:161–5.
Sun Q, Wu W, Hu YC, et al. Early release of high-mobility group box 1 (HMGB1) from neurons in experimental subarachnoid hemorrhage in vivo and in vitro. J Neuroinflamm. 2014;11:106.
Acknowledgements
We thank Dr. Marlene Santos for her excellent coordination of sample collection and ongoing study enrollment and Ms. Witty Tse for technical assistance. In accordance with the Department of National Defence policy, the paper was reviewed and approved for submission without modification by the DRDC Publications Office.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests. Dr. Bell and Dr. Baker report receiving funds from the Physician Services Incorporated Foundation and the Canadian Anesthesiologists Society in collaboration with Ontario’s Anesthesiologists and the Canadian Anesthesia Research Foundation.
Additional information
Disclaimer: Opinions expressed or implied in this publication are those of the authors and do not represent the views or policy of the Department of National Defence or the Canadian Armed Forces.
Electronic supplementary material
Below is the link to the electronic supplementary material.
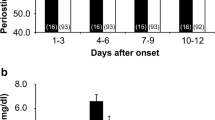
Supplementary Figure 1
Further evidence of evolving endotheliopathy and glycocalyx damage. A + B) CSF data for MMP-3 and MMP-9 demonstrate these metalloproteinases do not increase with the onset of DCI and that the increase in MMP-1 was specific to that isoform. C) Subarachnoid hemorrhage is associated with a large increase of soluble vascular adhesion protein-1, suggesting breakdown of the endothelium and release of surface receptors, detectable as soluble fragments in plasma. D) SAH is similarly associated with upregulation of soluble CD44, the hyaluronic acid receptor and a critical component of the endothelial glycocalyx. E) Raw data for vascular adhesion protein-1, showing compelling upregulation in all patients studied. F) SAH is associated with increased plasma IL-6 and HMGB1, but the onset of DCI does not change these levels, suggesting the increase in CSF IL-6 likely originates within the brain parenchyma via native or transmigrated immune cells. * = p < 0.05 vs control, ** = p < 0.05 vs. SAH, SAH = subarachnoid hemorrhage, DCI = delayed cerebral ischemia, CSF = cerebrospinal fluid, VAP-1 = vascular adhesion protein-1, MMP = matrix metalloproteinase, IL-6 = interleukin 6, HMGB1 = high-mobility group box 1 (JPEG 713 kb)
Rights and permissions
About this article
Cite this article
Bell, J.D., Rhind, S.G., Di Battista, A.P. et al. Biomarkers of Glycocalyx Injury are Associated with Delayed Cerebral Ischemia Following Aneurysmal Subarachnoid Hemorrhage: A Case Series Supporting a New Hypothesis. Neurocrit Care 26, 339–347 (2017). https://doi.org/10.1007/s12028-016-0357-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-016-0357-4