Abstract
Coronavirus disease 2019 (COVID-19) is a viral infection caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). A single-stranded RNA virus from a β-Coronaviridae family causes acute clinical manifestations. Its high death rate and severe clinical symptoms have turned it into the most significant challenge worldwide. Up until now, several effective COVID-19 vaccines have been designed and marketed, but our data on specialized therapeutic drugs for the treatment of COVID-19 is still limited. In order to synthesis virus particles, SARS-CoV-2 uses host metabolic pathways such as phosphoinositide3-kinase (PI3K)/protein kinase B (PKB, also known as AKT)/mammalian target of rapamycin (mTOR). mTOR is involved in multiple biological processes. Over-activation of the mTOR pathway improves viral replication, which makes it a possible target in COVID-19 therapy. Clinical data shows the hyperactivation of the mTOR pathway in lung tissues during respiratory viral infections. However, the exact impact of mTOR pathway inhibitors on the COVID-19 severity and death rate is yet to be thoroughly investigated. There are several mTOR pathway inhibitors. Rapamycin is the most famous inhibitor of mTORC1 among all. Studies on other respiratory viruses suggest that the therapeutic inhibitors of the mTOR pathway, especially rapamycin, can be a potential approach to anti-SARS-CoV-2 therapy. Using therapeutic methods that inhibit harmful immune responses can open a new chapter in treating severe COVID-19 disease. We highlighted the potential contribution of PI3K/Akt/mTOR inhibitors in the treatment of COVID-19.
Similar content being viewed by others
Introduction
SARS-CoV-2 has emerged since December 2019, a single-stranded RNA virus from a β-Coronaviridae family that causes acute clinical manifestations. An extremely contagious viral infection that soon turned into a global nightmare [1]. COVID-19, with high mortality rates and severe clinical manifestations, has become the world’s greatest challenge since 2019. There is an urgent need for efficient therapeutic agents to prevent and cure COVID-19 infection [2]. SARS-CoV-2 needs the host cell cycles for its replication. It modifies the host metabolism pathways to synthesize the virus particles such as proteins and nucleotides [3]. SARS-CoV-2 can improve its survival and replication by dysregulating the PI3K/Akt/mTOR signaling pathway [4]. The onset of SARS-CoV-2 infection generally induces immune-related mechanisms such as oxidative stress and triggers a cytokine storm, leading to severe clinical manifestations in the infected host [5]. The host signaling pathways such as the PI3K/Akt/mTOR pathway can modify the production of pro-inflammatory cytokines (e.g., IL-8) [6]. Therefore, therapeutic methods that inhibit harmful immune responses can open a new chapter in treating severe COVID-19 disease [5].
Cellular signaling pathways play critical roles during viral infections. PI3K/Akt/mTOR pathway is the most outstanding pathway and is considered as a possible target for anti-COVID-19 treatment [6]. mTOR (also known as the mechanistic target of rapamycin) is a serine-threonine protein kinase involved in various biological processes, including metabolism pathways, protein synthesis, cell proliferation, autophagy, and cell growth [7]. Since mTOR is involved in initiating the inflammatory response, the inhibitory compounds of this pathway (such as rapamycin) can reduce the severity of the disease [8].
Like other viruses, SARS-CoV-2 exploits the host’s metabolic pathways to synthesize the proteins needed for its replication, leading to abnormal activation of signaling cascades [9]. Over-activation of the PI3K/Akt/mTOR pathway can be closely correlated with COVID-19 severity. Thus, using PI3K/Akt/mTOR pathway therapeutic inhibitors with other drugs may help researchers effectively treat COVID-19 [10]. Here in this article, we aim to review the role of the PI3K/Akt/mTOR pathway in SARS-CoV-2 infection and to comment on the efficiency and effect of their inhibitors in COVID-19 treatment.
The mTOR pathway in the immune system
A letter by Omarjee L. et al.suggests that targeting mTORC1 with rapamycin could be a potential therapeutic in COVID-19 patients [11]. The inflammation caused by the host immune system during COVID-19 can lead to pathological injuries, including acute respiratory distress syndrome (ARDS) and eventual death. High percentages of Th17 and low percentages of Treg have been reported in COVID-19 patients [1]. Previous studies have shown that mTORC1 plays a role in inducing Th17 and Th1 differentiation during viral infections, and mTORC2 can enhance Th2 differentiation, while both complexes reduce Treg differentiation [11]. mTOR over-activation during SARS-CoV-2 infection increased Th17 differentiation and decreased Treg differentiation, which ultimately led to increased immunopathology. Therefore, inhibitors of the mTOR pathway can significantly prevent the pathological damage caused by COVID-19 infection [12]. Duarte de Souza et al. reported that RSV interferes with TCD8+ lymphocytes proliferation through mTOR phosphorylation. Therefore, rapamycin administration can increase the antiviral TCD8+ lymphocytes population [13]. These studies introduce the mTOR signaling pathway as the potential Achilles heel of viral infection.
The role of the PI3K/Akt/mTOR axis in the development of regulatory immune responses and its involvement in cell differentiation has made this pathway an ideal target for a variety of viruses [14], although more investigations are needed to evaluate the precise and extensive effects of targeting the mTOR pathway during viral infections, especially SARS-CoV-2.
SARS-CoV-2 and mTOR pathway
SARS-CoV-2 interacts with angiotensin I-converting enzyme 2 (ACE2) via its spike glycoprotein, and receptor-binding domain (RBD) of the virus binds to the external domain of ACE2, which therefore boosts the viral entry into the host cells [6]. ACE2 was proven to be related to susceptibility to COVID-19 infection. Hence, pharmaceutical agents that can target the expression of ACE2 may lead to effective therapeutic approaches [15]. SARS-CoV-2 infection can lead to hyperactivation of mTOR in vitro. The unregulated activation of the mTOR pathway is assumed to be related to the pathogenesis of SARS-CoV-2 [1]. The use of nanomolar concentrations of inhibitors of mTOR showed that PI3K/AKT/mTOR is an important signaling pathway during SARS-CoV-2 infection [16]. As mTOR activity increases during MERS-CoV infection, due to many similarities between SARS-CoV-2 and MERS-CoV, it is speculated that SARS-CoV-2 infection also leads to hyperactivation of mTOR pathway [2]. P.j. Mullen. et al. reported an increase in mTORC1 activity in Lung ALI cultures and cell lines in SARS-CoV-2 infection. Due to the activation of mTORC1 in the lung cells of SARS-CoV-2 patients, inhibitors of mTORC1 declined the virus replication in lung ALI cultures and kidney epithelial cells, suggesting mTORC1 inhibitors as potential treatments for COVID-19 [17].
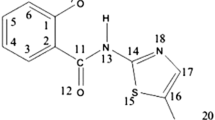
As shown in Fig. 1, the entry of the virus into the host cell causes the over-activation of PI3K, which activates mTOR by phosphorylating Akt. mTOR eventually increases the protein synthesis (including viral proteins), the production of inflammatory cytokines, and infected cell survival, which can be inhibited by therapeutic inhibitors of PI3K/Akt/mTOR cascade.
Activation of the mTOR pathway by SARS-CoV-2. PI3K activates mTORC1 by phosphorylating Akt. PI3K/Akt/mTOR inhibitors may enhance the SARS-CoV-2 infected cells autophagy and impede the viral replication and the subsequent hyper-inflammation. SARS‐CoV‐2, severe acute respiratory syndrome coronavirus 2; mTOR, mammalian target of rapamycin; PI3K, phosphoinositide3-kinase; PKB (or Akt), protein kinase B; PDK1, Phosphoinositide-Dependent Kinase-1; mTORC1, mTOR Complex 1; ACE2, angiotensin-converting enzyme 2
Several factors regulate PI3K/AKT/mTOR pathway, including growth factors and their receptors, amino acids, Toll-like receptor ligands, cellular stress, energy status, and some negative regulators such as phosphatase and tensin homolog (PTEN) [18, 19]. The activation of regulators such as growth factors receptor recruits PI3K to the cell membrane and phosphorylates AKT which later induces mTOR activation leading to the activation of its downstream effectors (4EBP1 and P70S6) and eventually induces RNA translation, protein synthesis, cell survival, and so on [18]. mTORC1 also inhibits unc-51-like kinase 1 (ULK1) and autophagy-related gene 13 (ATG13) via phosphorylation which results in autophagy inhibition [20].
Once the virus enters, the activation of eukaryotic translation initiation factor 4E-binding protein1 (4-E-BP1) and ribosomal protein S6 kinase beta 1 (S6K1) (downstream mTOR compounds) leads to increased synthesis of ribosomes and proteins (including viral proteins) [9]. SARS-CoV-2 infection can lead to hyperactivation of mTOR in vitro, and since the unregulated activation of the mTOR pathway plays a decisive role in COVID-19-induced pathogenesis, inhibiting this pathway can prevent the progression of infection [1]. Thus, drug inhibitors of the mTOR or microRNAs that interact with 3-UTR of mTOR could be a proper candidate for treating COVID-19 patients [9]. Data from gene-trapping of five genes associated with the PI3K/AKT/mTOR pathway including, AKT2 and mTOR (HSV-2), RAPTOR and FK506 binding protein 8 (FKBP8; reovirus), and insulin receptor substrate 1 (IRS1, influenza A/WS/33) and siRNA screening of the indicated genes in influenza A/WS/33 or respiratory syncytial virus (RSV), herpes simplex virus-2 (HSV-2), human rhinovirus 16 (HRV16), dengue fever virus type 2 (DFV-2), and cowpox, showed that they play an important role in viral replication. For example mTOR knockdown leads to a reduction in HRV16 and cowpox replication and AKT1, IRS1, and FKBP8 siRNA could inhibit influenza A infection [21]. Since the PI3K/AKT-mTOR pathway is a key signaling pathway in the replication of most viruses, precise molecular screening of this pathway can help elucidate the exact mechanism of these cellular signaling cascades.
SARS-CoV-2 also enhances the expression of pyruvate carboxylase and decreases the metabolism of oxidative glutamin, suggesting SARS-CoV-2 had remodeled the host carbon-metabolism pathways to produce its particles [3]. However, still more studies are required to fully reveal the precise mechanisms of SARS-CoV-2 using the host cell pathways for its replication.
Since mTORC1 can control autophagy, some viruses inhibit mTORC1 activity and increase their replication rate via autophagy, for example, the hepatitis C virus (HCV)-induced autophagy by mTORC1 blockade under endoplasmic reticulum stress (ER stress) [22]. Highly pathogenic avian influenza A (H5N1) virus activates autophagy by blocking mTOR pathway; hence, inhibitors of autophagy may be potential treatments in H5N1 infection [23]. M2 and NP proteins of influenza A virus (IAV) activate autophagy via mTOR axis leading to the virus replication [24]. Considering the proviral role of autophagy in ZIKA infection, NS4A and NS4B (nonstructural protein 4A and AB) block AKT and mTOR which results in autophagy induction [23]. Based on recent findings the dengue virus (DENV), a flavivirus, also induces autophagy to improve its replication [25].
Rapamycin: a proper mTORC1 inhibitor
mTOR interacts with several proteins, which later form two complexes: mTORC1 (sensitive to rapamycin) and mTORC2 (non-sensitive to rapamycin) [7]. Various mTOR pathway inhibitors (such as rapamycin) have been presented up until now [8]. AMPK is considered a significant regulator of mTORC1. Metformin can inhibit mTOR signaling pathway by activating AMPK via phosphorylating raptor and TSC2/1 [26]. Rapamycin specifically inhibits mTORC1. After binding to FKBP12, it forms the rapamycin-FKBP12 compound, which then integrates with the FKBP12-rapamycin (FRB) domain of mTORC1, impedes the interaction between mTOR, and raptor, and eventually leads to inhibition of mTORC1 [19]. Rapamycin inhibits PI3K/AKT/ mTORC1 by blocking mTORC1 during MERS-CoV which has a positive effect on preventing the virus replication [9].
As shown in Fig. 1, mTORC1 and mTORC2 have different components and can have different effects on signaling pathways. Raptor subunit in mTORC1 is found to be sensitive to rapamycin and is thus inhibited by it, while Rictor subunit of mTORC2 is rapamycin-insensitive and therefore not inhibited by rapamycin. The rapamycin-sensitive mTORC1 has a key role in protein synthesis, cell growth, and so on and the rapamycin-insensitive mTORC2 is mostly involved in cell survival and cytoskeletal organization [27].
Rapamycin blocks mTORC1 during MERS-CoV infection. Rapamycin also significantly prevents MERS-CoV infection by blocking LARP1 (the translational receptor of mTOR)[9]. Rapamycin binds to the FRB (FKBP12-rapamycin-binding) and FK506-binding protein12 (FKBP12) domain of mTOR and blocks the protein synthesis pathway of mTOR, thereby decreases the differentiation of lymphocytes [8, 28]. Rapamycin inactivates mTORC1 by binding to the immunophilin FK506-binding protein12A (FKBP12A) and preventing the effective interaction between mTOR and regulatory-associated protein of mTOR, also known as raptor [9].
Although the exact mechanism is not yet precise, it has been reported that rapamycin can prevent the onset of cytokine storms and related pathological damage by impeding the production of inflammatory cytokines inhibitors of mTOR may prevent the development of severe pathological symptoms in COVID-19 patients by selectively reducing the population of B lymphocytes and consequently blocking cross‐reactive antibodies expression [2]. By affecting the cell cycle of T lymphocytes (G1-S), rapamycin disrupts the signaling pathway of cytokine production to prevent severe inflammation during disease [8].
Rapamycin attenuates the replication rate of MERS-CoV in vitro by blocking the signaling of mTOR pathway. Moreover, corticosteroids and mTOR inhibitors in patients with severe HIN1 influenza accelerate the healing process [2]. It seems that the high rate of mutation in the SARS-CoV-2 will not reduce the effectiveness of this drug [8]. In patients with H1N1 pneumonia, inhibition of mTOR pathway by rapamycin in combination with corticosteroids significantly reduced clinical manifestations and the duration of ventilator use [29].
The current clinical trials that inhibit mTOR include phase I (SirCo-1, NCT04371640) which was withdrawn in 2021, phase II (The SCOPE trials, NCT04341675) which has had no update for over 1.5 years, and also phase III (NCT04409327) trial which was closed in Feb 2021 due to insufficient accrual rate [4].
Metformin, tacrolimus, sapanisertib, and PP-242: mTOR inhibitors
Experimental studies on other inhibitory drugs have revealed that metformin blocks mTOR signaling by inducing AMPK (through LKB1) and inhibits Akt via phosphorylated IRS [9]. Therefore, it can be helpful in the treatment of COVID-19. Recent retrospective studies suggest metformin as an effective pharmacological treatment in COVID-19 patients based on data on SARS-CoV-2 patients with diabetes mellitus [27]. Metformin inhibits mTORC1 by AMPK phosphorylation and activation via activating liver kinase B1 (LKB1). Also indirectly, by phosphorylating insulin receptor substrate 1 (IRS1), it attenuates AKT and inhibits mTORC1, which can ultimately lead to a reduction in disease severity and death rate. Metformin induces ACE2 phosphorylation via activation of AMPK and reduces the entry rate of SARS-Cov-2 into host cells [30]. More detailed studies reveal that metformin also inhibits mTORC1 through activating transcription factor 4 (ATF4)/regulated in DNA damage and development 1 (REDD1), or via p53/REDD1, or by induction of ataxia telangiectasia mutated (ATM) and also through a GTPase-dependent pathway [31]. Since metformin has a significant impact on MERS-CoV by inhibiting PI3K/AKT/mTOR and considering the similarities between MERS-CoV and SARS-CoV-2, its role in COVID-19 should be examined [30].
Using everolimus or rapamycin in H5N1-and H1N1-infected mice significantly reduced pathological lung tissue damage and decreased viral titers in the respiratory system, indicating the importance of mTOR pathway inhibitors in respiratory viral infections [21]. tacrolimus has shown a more significant inhibitory effect on cellular immune responses than everolimus, but both inhibit humoral immune responses equally. as a result, tacrolimus can be effective in COVID-19 treatment due to its ability to attenuate the production of T-related cytokines [5]. Oral administration of sapanisertib (INK0128; INK128) blocks mTORC1 and mTORC2 [9]. PP-242 also significantly prevents PRRSV (porcine reproductive, respiratory syndrome virus) infection by inhibiting mTORC1 and mTORC2 [32]. Of course, more detailed and specialized studies on these inhibitors can pave the way for more effective treatments for viral infections, especially SARS-CoV-2. The mTOR pathway inhibitors (such as rapamycin or everolimus, temsirolimus, MK-2206, and wortmannin) can reduce the pathological damage caused by the immune response to SARS-CoV-2, but do not decrease the ability of the immune system to respond to subsequent viral infections [4]. Further in vitro experiments and clinical trials are recommended to fully elucidate the efficacy of using PI3K/Akt/mTOR (and particularly mTOR) inhibitors as a therapeutic approach for treating SARS-CoV-2 severe disease. Some of the most important and well-known inhibitors of this pathway (which have been clinically studied in recent years) are listed in Table 1.
Inhibition of PI3K/Akt/ mTOR pathway
The PI3K/Akt/mTOR compounds (such as mTOR, AKT1, RPS6KB1, PIK3R1, and PIK3R2) increases during MERS-CoV infection. It has been reported that high concentrations of wortmannin (PI3K inhibitor) reduce MERS-CoV titers by blocking the PI3K/Akt pathway [8]. Rapamycin also inhibits MERS-CoV replication by blocking mTOR [14]. The influential role of PI3K/Akt/mTOR in MERS-CoV infection identifies pharmacological inhibitors of this pathway as possible candidates in the treatment of viral infections such as MERS-CoV and SARS-CoV.
Experimental data from the Borchers C. et al. study made it clear that PI3K activation during COVID-19 infection did not directly stimulate the spike protein-induced IL-8 production [6]. Wang L. et al. found that activation of the PI3K/Akt signaling pathway in cancers induces the production of some pro-inflammatory cytokines, including IL-8 [33]. So, blocking the PI3K/Akt and its downstream molecules like mTOR may improve the treatment of cancer and even viral infections such as SARS-CoV-2 by preventing the expression of cytokines and thus inhibiting the inflammation.
Knockout of the PI3K gene leads to attenuation of T lymphocytes responses. PI3K inhibition also increases CD4+ T lymphocytes. On the other hand, inhibition of PI3K reduces the activity of mast cells and neutrophils in lung diseases [10]. A study on Vero E6 cells revealed that PI3K/Akt axis plays an essential role in SARS-CoV persistence [34]. Administration of idelalisib, a PI3K inhibitor, reduces the expression of inflammatory cytokines, reducing the pathological damage caused by inflammation in COVID-19 patients and accelerating the healing process [10].
Inhibition of Akt by MK-2206 in Huh-7 cell line and Vero FM cell line was able to reduce the replication of the SARS-CoV-2 effectively. Vorinostat or SAHA also inhibited the replication of SARS-CoV-2 in the Huh-7 cell line via the mTOR1 blockage [4], while rapamycin, wortmannin, and BI-D1870 did not significantly inhibit the SARS-CoV-2 proliferation in the Huh-7 cell line [4]. In order to prevent the systematic effects of PI3K/Akt/mTOR inhibition in the body, the use of the inhalation drug is recommended [10].
Further investigations are required to clarify the precise role of PI3K/Akt during COVID-19 infection.
Inhibitory drugs: foes or allies?!
Although inhibitory drugs that interfere with host signaling pathways or immune responses can effectively prevent pathological damages, some of these drugs may cause adverse effects, usually through immunosuppression properties [35]. For instance, rapamycin, despite its inhibitory role in virus replication during severe H1N1 infection, can cause pathological damage to lung tissue by breaking down the immune barriers [4]. Rapamycin decreases CD19+ CD27+ memory B lymphocytes and induces their differentiation to plasma cells. It is also shown that rapamycin (by inducing HLA-DR expression) was more effective in reducing the population of B lymphocytes than tacrolimus [5]. In the light of such investigations, it can be concluded that rapamycin can play a role in intervening in the production of antibodies in COVID-19 by reducing the population of B lymphocytes.
Since mTOR inhibitors can reduce the titer of cross-reactive antibodies, they may impair disease recovery by reducing the beneficial antibodies [8]. Although rapamycin acts like a double-edged sword in viral infections, it is still more effective than other drugs [35]. Previous studies also reported the contradictory impacts of rapamycin on the differentiation of T subtypes, especially regulatory T lymphocytes [4, 36]. However, blocking the mTOR pathway may present a more efficient and less detrimental immunosuppressive effect in comparison with other inhibitory drugs such as calcineurin [35]. Of course, since there is still scarce data about the potentially harmful effects of such compounds, they should probably be prescribed in doses similar to anti-cancer studies.
Conclusion
Here in this review, we highlighted the importance of the PI3K/Akt/mTOR pathway in viral infections and its potential involvement during COVID-19. Viruses such as SARS-CoV-2 use the host signaling pathways and biological mechanisms for their survival and replication. Hence, using inhibitors of these cellular pathways and antiviral and anti-inflammatory drugs may improve the therapeutic approaches in this catastrophic pandemic. Although confirmed data on the role of the mTOR pathway in COVID-19 is still limited, experimental and clinical evidence on similar respiratory viruses such as MERS-CoV, RSV, and influenza suggest that using therapeutic inhibitors of the mTOR pathway may be a distinctive approach to anti-SARS-CoV-2 therapy. To date, several effective COVID-19 vaccines have been developed and marketed, but our knowledge of specialized therapeutic drugs for the treatment of COVID-19 is insufficient. Therefore, finding an effective drug (with the most negligible side effects) that prevents pathological damage (caused by the viral infection) and improves the survival rate in patients is a vital necessity.
Data availability
The dataset of the current study are available from the corresponding author on reasonable request.
References
Yang F, Chen R, Li WY, Zhu HY, Chen XX, Hou ZF, et al. D-Limonene is a potential monoterpene to inhibit PI3K/Akt/IKK-α/NF-κB p65 signaling pathway in coronavirus disease 2019 pulmonary fibrosis. Front Med. 2021;8:591830. https://doi.org/10.3389/fmed.2021.591830.
Zheng Y, Li R, Liu S. Immunoregulation with mTOR inhibitors to prevent COVID-19 severity: a novel intervention strategy beyond vaccines and specific antiviral medicines. J Med Virol. 2020;92(9):1495–500. https://doi.org/10.1002/jmv.26009.
Mullen PJ, Garcia G Jr, Purkayastha A, Matulionis N, Schmid EW, Momcilovic M, et al. SARS-CoV-2 infection rewires host cell metabolism and is potentially susceptible to mTORC1 inhibition. Nat Commun. 2021;12(1):1876. https://doi.org/10.1038/s41467-021-22166-4.
Appelberg S, Gupta S, Svensson Akusjärvi S, Ambikan AT, Mikaeloff F, Saccon E, et al. Dysregulation in Akt/mTOR/HIF-1 signaling identified by proteo-transcriptomics of SARS-CoV-2 infected cells. Emerging microbes & infections. 2020;9(1):1748–60. https://doi.org/10.1080/22221751.2020.1799723.
Hasbal NB, Turgut D, Gok Oguz E, Ulu S, Gungor O. Effect of calcineurin inhibitors and mammalian target of rapamycin inhibitors on the course of COVID-19 in kidney transplant recipients. Ann Transplant. 2021;26:e929279. https://doi.org/10.12659/aot.929279.
Borchers C, Thyagarajan A, Rapp CM, Travers JB, Sahu RP. Evaluation of SARS-CoV-2 spike S1 protein response on PI3K-mediated IL-8 release. Med Sci. 2021;9(2):30. https://doi.org/10.3390/medsci9020030.
Laplante M, Sabatini DM. mTOR signaling in growth control and disease. Cell. 2012;149(2):274–93. https://doi.org/10.1016/j.cell.2012.03.017.
Patocka J, Kuca K, Oleksak P, Nepovimova E, Valis M, Novotny M, et al. Rapamycin: drug repurposing in SARS-CoV-2 infection. Pharmaceuticals (Basel). 2021;14(3):217. https://doi.org/10.3390/ph14030217.
Ramaiah MJ. mTOR inhibition and p53 activation, microRNAs: the possible therapy against pandemic COVID-19. Gene reports. 2020;20:100765. https://doi.org/10.1016/j.genrep.2020.100765.
Palma G, Pasqua T, Silvestri G, Rocca C, Gualtieri P, Barbieri A, et al. PI3Kδ Inhibition as a potential therapeutic target in COVID-19. Front Immunol. 2020;11:2094. https://doi.org/10.3389/fimmu.2020.02094.
Omarjee L, Janin A, Perrot F, Laviolle B, Meilhac O, Mahe G. Targeting T-cell senescence and cytokine storm with rapamycin to prevent severe progression in COVID-19. Clinical immunology (Orlando, Fla). 2020;216:108464. https://doi.org/10.1016/j.clim.2020.108464.
Kurebayashi Y, Nagai S, Ikejiri A, Ohtani M, Ichiyama K, Baba Y, et al. PI3K-Akt-mTORC1-S6K1/2 axis controls Th17 differentiation by regulating Gfi1 expression and nuclear translocation of RORγ. Cell Rep. 2012;1(4):360–73. https://doi.org/10.1016/j.celrep.2012.02.007.
de Souza AP, de Freitas DN, Antuntes Fernandes KE, D’Avila da Cunha M, Antunes Fernandes JL, Benetti Gassen R et al. Respiratory syncytial virus induces phosphorylation of mTOR at ser2448 in CD8 T cells from nasal washes of infected infants. Clinical and experimental immunology. 2016;183(2):248–57. https://doi.org/10.1111/cei.12720.
Kindrachuk J, Ork B, Hart BJ, Mazur S, Holbrook MR, Frieman MB, et al. Antiviral potential of ERK/MAPK and PI3K/AKT/mTOR signaling modulation for Middle East respiratory syndrome coronavirus infection as identified by temporal kinome analysis. Antimicrob Agents Chemother. 2015;59(2):1088–99. https://doi.org/10.1128/aac.03659-14.
Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181(2):271-80.e8. https://doi.org/10.1016/j.cell.2020.02.052.
Garcia Jr G, Sharma A, Ramaiah A, Sen C, Kohn DB, Gomperts BN, et al. Antiviral drug screen of kinase inhibitors identifies cellular signaling pathways critical for SARS-CoV-2 replication. 2020. Available at SSRN: https://ssrn.com/abstract=3682004 or https://doi.org/10.2139/ssrn.3682004.
Mullen PJ, Garcia G, Purkayastha A, Matulionis N, Schmid EW, Momcilovic M, et al. SARS-CoV-2 infection rewires host cell metabolism and is potentially susceptible to mTORC1 inhibition. Nat Commun. 2021;12(1):1–10.
Porta C, Paglino C, Mosca A. Targeting PI3K/Akt/mTOR signaling in cancer. Front Oncol. 2014;4:64.
Rostamzadeh D, Yousefi M, Haghshenas MR, Ahmadi M, Dolati S, Babaloo Z. mTOR Signaling pathway as a master regulator of memory CD8+ T-cells, Th17, and NK cells development and their functional properties. J Cell Physiol. 2019;234(8):12353–68.
Laplante M, Sabatini DM. mTOR signaling at a glance. J Cell Sci. 2009;122(20):3589–94.
Murray JL, McDonald NJ, Sheng J, Shaw MW, Hodge TW, Rubin DH, et al. Inhibition of influenza A virus replication by antagonism of a PI3K-AKT-mTOR pathway member identified by gene-trap insertional mutagenesis. Antiviral Chem Chemother. 2012;22(5):205–15. https://doi.org/10.3851/imp2080.
Huang H, Kang R, Wang J, Luo G, Yang W, Zhao Z. Hepatitis C virus inhibits AKT-tuberous sclerosis complex (TSC), the mechanistic target of rapamycin (MTOR) pathway, through endoplasmic reticulum stress to induce autophagy. Autophagy. 2013;9(2):175–95.
Ma J, Sun Q, Mi R, Zhang H. Avian influenza A virus H5N1 causes autophagy-mediated cell death through suppression of mTOR signaling. J Genet Genomics. 2011;38(11):533–7.
Wang R, Zhu Y, Zhao J, Ren C, Li P, Chen H, et al. Autophagy promotes replication of influenza A virus in vitro. J Virol. 2019;93(4):e01984-e2018.
Liang Q, Luo Z, Zeng J, Chen W, Foo S-S, Lee S-A, et al. Zika virus NS4A and NS4B proteins deregulate Akt-mTOR signaling in human fetal neural stem cells to inhibit neurogenesis and induce autophagy. Cell Stem Cell. 2016;19(5):663–71.
Zakikhani M, Blouin M-J, Piura E, Pollak MN. Metformin and rapamycin have distinct effects on the AKT pathway and proliferation in breast cancer cells. Breast Cancer Res Treat. 2010;123(1):271–9.
Kamyshnyi O, Matskevych V, Lenchuk T, Strilbytska O, Storey K, Lushchak O. Metformin to decrease COVID-19 severity and mortality: molecular mechanisms and therapeutic potential. Biomed Pharmacother. 2021;144:112230. https://doi.org/10.1016/j.biopha.2021.112230.
Yang H, Rudge DG, Koos JD, Vaidialingam B, Yang HJ, Pavletich NP. mTOR kinase structure, mechanism and regulation. Nature. 2013;497(7448):217–23. https://doi.org/10.1038/nature12122.
Jia X, Liu B, Bao L, Lv Q, Li F, Li H, et al. Delayed oseltamivir plus sirolimus treatment attenuates H1N1 virus-induced severe lung injury correlated with repressed NLRP3 inflammasome activation and inflammatory cell infiltration. PLoS Pathog. 2018;14(11):e1007428. https://doi.org/10.1371/journal.ppat.1007428.
Sharma S, Ray A, Sadasivam B. Metformin in COVID-19: a possible role beyond diabetes. Diabetes Res Clin Pract. 2020;164:108183. https://doi.org/10.1016/j.diabres.2020.108183.
Melnik BC, Schmitz G. Metformin: an inhibitor of mTORC1 signaling. J Endocrinol Diabetes Obes. 2014;2(2):1029.
Liu Q, Miller LC, Blecha F, Sang Y. Reduction of infection by inhibiting mTOR pathway is associated with reversed repression of type I interferon by porcine reproductive and respiratory syndrome virus. J Gen Virol. 2017;98(6):1316–28. https://doi.org/10.1099/jgv.0.000802.
Wang L, Tang C, Cao H, Li K, Pang X, Zhong L, et al. Activation of IL-8 via PI3K/Akt-dependent pathway is involved in leptin-mediated epithelial-mesenchymal transition in human breast cancer cells. Cancer Biol Ther. 2015;16(8):1220–30. https://doi.org/10.1080/15384047.2015.1056409.
Mizutani T, Fukushi S, Saijo M, Kurane I, Morikawa S. JNK and PI3k/Akt signaling pathways are required for establishing persistent SARS-CoV infection in Vero E6 cells. Biochem Biophys Acta. 2005;1741(1–2):4–10. https://doi.org/10.1016/j.bbadis.2005.04.004.
Terrazzano G, Rubino V, Palatucci AT, Giovazzino A, Carriero F, Ruggiero G. An open question: is it rational to inhibit the mTor-dependent pathway as COVID-19 therapy? Front Pharmacol. 2020;11:856. https://doi.org/10.3389/fphar.2020.00856.
Traitanon O, Mathew JM, La Monica G, Xu L, Mas V, Gallon L. Differential Effects of tacrolimus versus sirolimus on the proliferation, activation and differentiation of human B cells. PLoS ONE. 2015;10(6):e0129658. https://doi.org/10.1371/journal.pone.0129658.
Hirai H, Sootome H, Nakatsuru Y, Miyama K, Taguchi S, Tsujioka K, et al. MK-2206, an allosteric Akt inhibitor, enhances antitumor efficacy by standard chemotherapeutic agents or molecular targeted drugs in vitro and in vivo. Mol Cancer Ther. 2010;9(7):1956–67. https://doi.org/10.1158/1535-7163.mct-09-1012.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
All authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fattahi, S., Khalifehzadeh-Esfahani, Z., Mohammad-Rezaei, M. et al. PI3K/Akt/mTOR pathway: a potential target for anti-SARS-CoV-2 therapy. Immunol Res 70, 269–275 (2022). https://doi.org/10.1007/s12026-022-09268-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12026-022-09268-x