Abstract
Purpose
Poor sleep accompanied by elevated TSH (thyroid stimulating hormone) levels is not uncommon since TSH secretion is controlled by the circadian rhythm. However, the relationship between poor sleep and TSH elevation is unclear; hence, we aimed to elucidate this relationship by conducting a cross-sectional and longitudinal study.
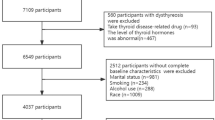
Methods
Participants with isolated elevated (N = 168) and normal (N = 119) TSH concentrations were recruited, and the Pittsburgh Sleep Quality Index (PSQI) was used to assess the sleep status. Subjects with an isolated TSH elevation were followed up longitudinally. The serum TSH concentration was remeasured after sleep status improved.
Results
The proportions of poor sleep and occasional poor sleep in subjects with isolated TSH elevation were significantly higher than those with normal TSH levels (70.24% vs. 49.58%, p = 0.001; 9.52% vs. 1.68%, p = 0.006). Subjects with isolated TSH elevation had significantly higher PSQI scores in the subjective sleep quality, sleep latency, sleep duration, and habitual sleep efficiency dimensions than those with normal TSH levels (all p < 0.05). Poor sleep was significantly associated with isolated TSH elevation in the multiple logistic regression analysis [odds ratio (OR) = 2.396, p = 0.001]. Among subjects with an isolated TSH elevation at baseline, the percentage of TSH normalization was significantly higher in those who slept better than in those who still slept poorly (85.42% vs. 6.45%, p < 0.001).
Conclusions
This study revealed that isolated elevated TSH concentrations normalize when the sleep status is improved; hence, we recommend that clinicians thoroughly assess the sleep status of patients and remeasure TSH concentrations after sleep status improves.


Similar content being viewed by others
References
J.G. Hollowell, N.W. Staehling, W.D. Flanders et al. Serum TSH, T4, and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab 87, 489–499 (2002)
S. Zou, F. Wu, C. Guo et al. Iodine nutrition and the prevalence of thyroid disease after salt iodization: a cross-sectional survey in Shanghai, a coastal area in China. PLoS ONE 7, e40718 (2012)
S.C. David, B. Bernadette, Subclinical thyroid disease. Lancet. 379, 1142–1154 (2012)
M.I. Surks, J.G. Hollowell, Age-specific distribution of serum thyrotropin and antithyroid antibodies in the US population: implications for the prevalence of subclinical hypothyroidism. J Clin Endocrinol Metab 92, 4575–4582 (2007)
A. Solanki, S. Bansal, S. Jindal et al. Relationship of serum thyroid stimulating hormone with body mass index in healthy adults. Indian J Endocrinol Metab 17, S167–S169 (2013)
E.M. Kaptein, J.S. LoPresti, M.J. Kaptein, Is an isolated TSH elevation in chronic nonthyroidal illness “subclinical hypothyroidism”? J Clin Endocrinol Metab 99, 4015–4026 (2014)
G. Brabant, K. Prank, U. Ranft et al. Physiological regulation of circadian and pulsatile thyrotropin secretion in normal man and woman. J Clin Endocrinol Metab 70, 403–409 (1990)
D.C. Parker, L.G. Rossman, A.E. Pekary et al. Effect of 64-h sleep deprivation on the circadian waveform of thyrotropin (TSH): further evidence of sleep-related inhibition of TSH release. J Clin Endocrinol Metab 64, 157–161 (1987)
E. Van Cauter, E. Tasali. Endocrine physiology in relation to sleep and sleep disturbances. Principles and practice of sleep medicine. M.H. Kryger, T. Roth, W.C. Dement editors. Elsevier Saunders, St Louis: MO), 1992)
M.C. Brum, F.F. Filho, C.C. Schnorr et al. Shift work and its association with metabolic Disorders. Diabetol Metab Syndr 7, 45 (2015)
L. Xia, G.H. Chen, Z.H. Li et al. Alterations in hypothalamus-pituitary-adrenal/thyroid axes and gonadotropin-releasing hormone in the patients with primary insomnia: a clinical research. PLoS ONE 8, e71065 (2013)
D J Buysse, C F Reynolds 3rd, T H Monk, et al. The Pittsburgh Sleep Quality Index: a new instrument forpsychiatric practice and research. Psychiatry Res 28, 193–213 (1989).
J. Tang, Y. Liao, B.C. Kelly et al. Gender and regional differences in sleep quality and insomnia: a general population-based study in Hunan Province of China. Sci Rep 7, 43690 (2017)
X. Liu, C. Liu, X. Tian et al. Associations of perceived stress, resilience and social support with sleep disturbance among community-dwelling adults. Stress Health 32, 578–586 (2016)
J. Li, X. Sun, Y. Yu, The prevalence of impaired glucose regulation in psychiatric patients with sleep disorders and its relationship with altered hypothalamopituitary-adrenal and hypothalamopituitary-thyroid axis activity. Sleep Med 14, 662–667 (2013)
Yue-Rong Yan, Jia-Qi Li, Ye-Rong Yu, Isolated thyrotropin elevation is associated with insufficient night-sleep in night-sleep restricted subjects. Chin Med J (Engl) 130, 3001–3002 (2017)
A. Aydin, Y. Selvi, L. Besiroglu et al. Mood and metabolic consequences of sleep deprivation as a potential endophenotype’ in bipolar disorder. J Affect Disord 150, 284–294 (2013)
D.J. Buysse, C.F. Reynolds, T.H. Monk et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28, 193–213 (1989)
W. Teng, Z. Shan, X. Teng et al. Effect of iodine intake on thyroid diseases in China. N Engl J Med 354, 2783–2793 (2006)
R.J. Adams, S.L. Appleton, A.W. Taylor et al. Sleep health of Australian adults in 2016: results of the 2016 Sleep Health Foundation national survey. Sleep Health 3, 35–42 (2017)
S.A. Bahammam, M.M. Sharif, A.A. Jammah et al. Prevalence of thyroid disease in patients with obstructive sleep apnea. Respir Med 105, 1755–1760 (2011)
J.S. Bajaj, L.R. Thacker, D. Leszczyszyn et al. Effects of obstructive sleep apnea on sleep quality, cognition, and driving performance in patients with cirrhosis. Clin Gastroenterol Hepatol 13, 390–397 (2015)
S. Takeuchi, T. Kitamura, T. Ohbuchi et al. Relationship between sleep apnea and thyroid function. Sleep Breath 19, 85–89 (2015)
O. Resta, P. Carratù, G.E. Carpagnano et al. Influence of subclinical hypothyroidism and T4 treatment on the prevalence and severity of obstructive sleep apnoea syndrome (OSAS). J Endocrinol Invest 28, 893–898 (2005)
J. Meyerovitch, P. Rotman-Pikielny, M. Sherf et al. Serum thyrotropin measurements in the community: five-year follow-up in a large network of primary care physicians. Arch Intern Med 167, 1533–1538 (2007)
R. Hoermann, J.E. Midgley, R. Larisch et al. Homeostatic control of the thyroid-pituitary axis: perspectives for diagnosis and treatment. Front Endocrinol (Lausanne) 6, 177 (2015)
A. Baumgartner, L. Hiedra, G. Pinna et al. Rat brain type II 5’-iodothyronine deiodinase activity is extremely sensitive to stress. J Neurochem 71, 817–826 (1998)
A.C. Bianco, B.W. Kim, Deiodinases: implications of the local control of thyroid hormone action. J Clin Invest 116, 2571–2579 (2006)
TaeHyuk Kim, KyungWon Kim, HwaYoung Ahn et al. Effect of seasonal changes on the transition between subclinical hypothyroid and euthyroid status. J Clin Endocrinol Metab 98, 3420–3429 (2013)
Jiaqi Li, Xueli Sun, Yerong Yu, The prevalence of impaired glucose regulation in psychiatric patients with sleep disorders and its relationship with altered hypothalamopituitary-adrenal and hypothalamopituitary-thyroid axis activity. Sleep Med 14, 662–667 (2013)
Author contributions
Y.Y. and J.L. contributed equally to this manuscript. Y.Y. performed the project, analyzed the data, and wrote the manuscript. J.L. helped to analyze the data and wrote the manuscript. W.Z., H.L., L.Z., and Z.X. helped to collect the data. H.T. and Y.W. helped to design the project. H.Y. helped to revise the manuscript. Y.Y. conceived and designed the project and revised the manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (81600603, 81902724), Chengdu Science and Technology Program (2019-YFYF-00143-SN) and China Postdoctoral Science Foundation Grant (2019M653230).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yan, Y., Li, J., Tang, H. et al. Elevated thyroid-stimulating hormone levels are associated with poor sleep: a cross-sectional and longitudinal study. Endocrine 75, 194–201 (2022). https://doi.org/10.1007/s12020-021-02849-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-021-02849-0