Abstract
Purpose
Patients with adrenal insufficiency (AI) are at risk of life-threatening illness. Medical jewellery is recommended for emergencies, but its uptake is unknown. This study assessed the use of medical jewellery among Australian AI patients aged 25 years and under.
Methods
Data on the age, sex, region, and diagnosis of subscribers to the largest medical jewellery provider in Australia were analysed. Subscription rates were calculated using 2017 Australian population data.
Results
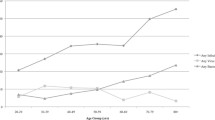
There were 666 patients aged 25 years and under in the database but only 358 (53.8%) had an active (up to date) subscription, corresponding to a subscription rate of 43.67/million or approximately 14.6% of the estimated patient population. The majority (n = 238, 66.5%) had primary AI; followed by secondary AI (n = 82, 22.9%); and the remaining patients (n = 38, 10.6%) could not be classified. Congenital adrenal hyperplasia (CAH) was the most frequent diagnosis (n = 153, 42.7%), corresponding to a subscription rate of 18.67/ million or 28.9% of the estimated number of patients with CAH. The mean age of subscribers was 15.9 (SD = 5.8) years. Only 18 (5%) patients were aged under 5 years. More females (n = 199, 55.9%) than males were active subscribers and subscription rates differed significantly by geographic area. Inactive (lapsed) subscriptions increased with age and were highest in the 20–25 year age group.
Conclusion
Subscription rates were lower than recommended; increased with age; and were more common in females. Older age was associated with higher levels of lapsed subscriptions. Factors leading to low use and discontinuation in young adults should be addressed.




Similar content being viewed by others
Data availability
Data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restriction.
References
P. Osuwannaratana, S. Nimkarn, J. Santiprabhob, S. Likitmaskul, P. Sawathiparnich, The etiologies of adrenal insufficiency in 73 Thai children: 20 years experience. J. Med. Assoc. Thail. 91(10), 1544–1550 (2008)
S.A. Bowden, R. Henry, Pediatric adrenal insufficiency: diagnosis, management, and new therapies. Int. J. Pediatrics 2018, 1739831 (2018). https://doi.org/10.1155/2018/1739831
J. Park, M. Didi, J. Blair, The diagnosis and treatment of adrenal insufficiency during childhood and adolescence. Arch. Dis. Child. 101(9), 860–865 (2016). https://doi.org/10.1136/archdischild-2015-308799
H.K. Gleeson, V. Wiley, B. Wilcken, E. Elliott, C. Cowell, M. Thonsett, G. Byrne, G. Ambler, Two-year pilot study of newborn screening for congenital adrenal hyperplasia in New South Wales compared with nationwide case surveillance in Australia. J. Paediatr. Child Health 44(10), 554–559 (2008)
S. Gidlöf, H. Falhammar, A. Thilén, U. von Döbeln, M. Ritzén, A. Wedell, A. Nordenström, One hundred years of congenital adrenal hyperplasia in Sweden: a retrospective, population-based cohort study. Lancet Diabetes Endocrinol. 1(1), 35–42 (2013)
R.L. Rushworth, D.J. Torpy, H. Falhammar, Adrenal crises: perspectives and research directions. Endocrine 55(2), 336–345 (2017)
E.B. Goldbloom, A. Mokashi, E.A. Cummings, S. Abish, S.M. Benseler, H.Q. Huynh, W. Watson, A. Ahmet, Symptomatic adrenal suppression among children in Canada. Arch. Dis. Child 102(4), 338–339 (2017)
A. Ahmet, V. Brienza, A. Tran, J. Lemieux, M. Aglipay, N. Barrowman, C. Duffy, J. Roth, R. Jurencak, Frequency and duration of adrenal suppression following glucocorticoid therapy in children with rheumatic diseases. Arthritis Car Res (Hoboken) 69(8), 1224–1230 (2017)
E. Bayman, A.J. Drake, Adrenal suppression with glucocorticoid therapy: still a problem after all these years? Arch. Dis. Child 102(4), 338–339 (2017)
R.L. Rushworth, D.J. Torpy, H. Falhammar, Adrenal crisis. N. Engl. J. Med. 381, 852–861 (2019)
R.L. Rushworth, H. Falhammar, C.F. Munns, A.M. Maguire, D.J. Torpy, Hospitalisation in children with congenital adrenal hyperplasia: the importance of younger age, viral infections and acute hypoadrenalism. Int. J. Endocrinol. 2016(ID 5738264), 1–7 (2016)
G.L. Chrisp, A.M. Maguire, M. Quartararo, H. Falhammar, B.R. King, C.F. Munns, D.J. Torpy, S. Hameed, R.L. Rushworth, Variations in the management of acute illness in children with congenital adrenal hyperplasia: an audit of three paediatric hospitals. Clin. Endocrinol. 89(5), 577–585 (2018)
R.L. Rushworth, D.J. Torpy, C. Stratakis, H. Falhammar, Adrenal crises in childhood: perspectives and research directions. Horm. Res. Paediatr. 89(5), 341–351 (2018)
S. Bornstein, B. Allolio, W. Arlt, A. Barthel, A. Don-Wauchope, G.D. Hammer, E.S. Husebye, D.P. Merke, M.H. Murad, C.A. Stratakis, D.J. Torpy, Diagnosis and treatment of primary adrenal insufficiency: an endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 101(2), 364–389 (2016)
R.L. Rushworth, G.L. Chrisp, D.J. Torpy, The use of medical identification jewellery in adults with adrenal insufficiency in Australia. Clin. Endocrinol. 91(1), 41–47 (2019)
Australian Bureau of Statistics, Australian demographic statistics, Jun 2017, estimated resident population b age and sex – at 30 June 2017, Datacube: Excel Spreadsheet, Cat no: 3101.0, 2017
J.H.Choi, H.W.Yoo, Management issues of congenital adrenal hyperplasia during the transition from pediatric to adult care. Korean J. Pediatr. 60(2), 31–37 (2017).
L.F. Zhang, J.S.W. Ho, S.E. Kennedy, A systematic review of the psychometric properties of transition readiness assessment tools in adolescents with chronic disease. BMC Pediatr. 14(4), 1–10 (2014)
S. Jenkins-Jones, L. Parviainen, J. Porter, M. Withe, M.J. Whitaker, S.E. Holden, C.L. Morgan, C.J. Currie, R.J.M. Ross, Poor compliance and increased mortality, depression and healthcare costs in patients with congenital adrenal hyperplasia. Eur. J. Endocrinol. 178(4), 309–320 (2018)
R.L. Rushworth, G.L. Chrisp, B. Dean, H. Falhammar, D.J. Torpy, Hospitalisation in children with adrenal insufficiency and hypopituitarism: is there a differential burden between boys and girls and between age groups? Horm. Res. Paediatr. 88(5), 339–346 (2017)
T. Goubar, D.J. Torpy, S. McGrath, R.L. Rushworth, Prehospital management of acute addisons disease: audit of patients attending a referral hospital in a regional area. J. Endocr. Soc. 3(12), 2194–2203 (2019)
A.P. Vidmar, J.F. Weber, R. Monzavi, C.M. Koppin, M.S. Kim, Improved medical-alert ID ownership and utilization in youth with congenital adrenal hyperplasia following a parent educational intervention. J. Pediatr. Endocrinol. Metab. 31(2), 213–219 (2018)
G. Meyer, A. Hackemann, J. Reusch, K. Badenhoop, Nocturnal hypoglycemia identified by a continuous glucose monitoring system in patients with primary adrenal insufficiency (Addison’s Disease). Diabetes Technol. Ther. 14(5), 386–388 (2012)
B. Mortimer, V.D. Naganur, P. Sartouris, J.R. Greenfield, D.J. Torpy, R.L. Rushworth, Acute illness in patients with concomitant Addison’s disease and type 1 diabetes mellitus: increased incidence of hypoglycaemia and adrenal crises. Clin Endocrinol. (2020). https://doi.org/10.1111/cen.14219
Acknowledgements
We thank MedicAlert Australia for provision of the data and for their support of the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
Permission to conduct this study was given by the Board of the subscription service and by the Human Research Ethics Committee of the University of Notre Dame, Australia (HREC Reference Number: 018070S).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chrisp, G.L., Quartararo, M., Torpy, D.J. et al. Use of medical identification jewellery in children and young adults with adrenal insufficiency in Australia. Endocrine 72, 539–545 (2021). https://doi.org/10.1007/s12020-020-02595-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-020-02595-9