Abstract
Purpose
End stage renal disease (ESRD) in male patients is associated with a high prevalence of hypogonadism. After renal transplantation (RTx) an improvement in gonadal function is often observed. However, the time course of changes in pituitary-gonadal axis after RTx and the influence of renal function, age and anthropometric parameters are not well characterized. We prospectively evaluated pituitary-gonadal axis in male patients with ESRD before and after RTx for up to 1 year.
Methods
Ninety-seven male patients with ESRD were consecutively investigated on day of surgery and 1, 3, 6, and 12 months after RTx. Time course of changes in sex hormones (total testosterone ((TT)), calculated free testosterone ((cfT)), estradiol (E2), LH, FSH and prolactin), and interdependence with renal function, age, anthropometric factors, cause of ERDS, time on dialysis, and transplant associated factors were analyzed.
Results
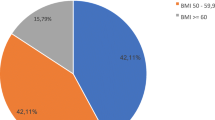
Hypogonadism (TT < 8 nmol/l) was present in 40% of pts prior to RTX and in only 18% at 1 year after RTX. Recovery from hypogonadism was significantly higher in pts < 50 years and occurred within 3 months. RTx resulted in a decrease in E2/T ratio starting at 1 month and suggesting a shift from estrogen to testosterone production. BMI and waist circumference had the similar impact on T levels after successful RTx compared to patients without renal disease. No specific impact on recovery of hypogonadism was found for time on dialysis prior to RTx and living or cadaver transplantation.
Conclusions
Successful RTx is associated with a rapid recovery from hypogonadism within 3 months preceeded by improvement in renal function particularly in patients younger than 50 years.




Similar content being viewed by others
References
J.J. Carrero, P. Stenvinkel, The vulnerable man: impact of testosterone deficiency on the uraemic phenotype. Nephrol. Dial. Transplant. 27, 4030–4041 (2012). https://doi.org/10.1093/ndt/gfs383
D.J. Handelsman, Hypothalamic–pituitary gonadal dysfunction in renal failure, dialysis and renal transplantation. Endocr. Rev. 6, 151–182 (1985)
A.K. Bello, P. Stenvinkel, M. Lin, B. Hemmelgarn, R. Thadhani, S. Klarenbach, C. Chan, D. Zimmerman, G. Cembrowski, G. Strippoli, J.J. Carrero, M. Tonelli, Serum testosterone levels and clinical outcomes in male hemodialysis patients. Am. J. Kidn Dis. 63, 268–275 (2014). https://doi.org/10.1053/j.ajkd.2013.06.010
J.J. Carrero, A.R. Qureshi, P. Parini, S. Arver, B. Lindholm, P. Bárány, O. Heimbürger, P. Stenvinkel, Low serum testosterone increases mortality risk among male dialysis patients. J. Am. Soc. Nephrol. 20, 613–620 (2009)
J. Kyriazis, I. Tzanakis, K. Stylianou, I. Katsipi, D. Moisiadis, A. Papadaki, V. Mavroeidi, S. Kagia, N. Karkavitsas, E. Daphnis, Low serum testosterone, arterial stiffness and mortality in male haemodialysis patients. Nephrol. Dial. Transplant. 26, 2971–2977 (2011). https://doi.org/10.1093/ndt/gfq847
D.A. Shoskes, H. Kerr, M. Askar, D.A. Goldfarb, J. Schold, Low testosterone at time of transplantation is independently associated with poor patient and graft survival in male renal transplant recipients. J. Urol. 192, 1168–1171 (2014). https://doi.org/10.1016/j.juro.2014.03.102
M. Grossmann, R. Hoermann, M. Ng Tang Fui, J.D. Zajac, F.L. Ierino, M.A. Roberts, Sex steroids levels in chronic kidney disease and kidney transplant recipients: associations with disease severity and prediction of mortality. Clin. Endocrinol. 82, 767–775 (2015). https://doi.org/10.1111/cen
J. Bao, Q. Yu, H. Yu, J. Hao, J. Liu, J. Yao, W. Yuan, Erectile dysfunction in male hemodialysis patients in China--one center experience. Clin. Nephrol. 75, 135–140 (2011)
D. Eckersten, A. Giwercman, A. Christensson, Male patients with terminal renal failure exhibit low serum levels of antimullerian hormone. J. Androl. 17, 149–153 (2015). https://doi.org/10.4103/1008-682X.135124
M.T. Saha, H.H. Saha, L.K. Niskanen, K.T. Salmela, A.I. Pasternack, Time course of serum prolactin and sex hormones following successful renal transplantation. Nephron 92, 735–737 (2002)
E. Samojlik, M.A. Kirschner, S. Ribot, E. Szmal, Changes in the hypothalamic-pituitary-gonadal axis in men after cadaver kidney transplantation and cyclosporine therapy. J. Androl. 13, 332–336 (1992)
J.D. Veldhuis, A. Iranmanesh, M.J. Wilkowski, E. Samojlik, Neuroendocrine alterations in the somatotropic and lactotropic axes in uremic men. Eur. J. Endocrinol. 131, 489–498 (1994)
S. Yi, E. Selvin, S. Rohrmann, S. Basaria, A. Menke, N. Rifai, E. Guallar, E.A. Platz, B. Astor, Endogenous sex steroid hormones and measures of chronic kidney disease (CKD) in a nationally representative sample of men. Clin. Endocrinol. 71, 246–252 (2009). https://doi.org/10.1111/j.1365-2265.2008.03455
F. Albaaj, M. Sivalingham, P. Haynes, G. McKinnon, R.N. Foley, S. Waldek, D.J. O’Donoghue, P.A. Kalra, Prevalence of hypogonadism in male patients with renal failure. Postgrad. Med. J. 82, 693–696 (2006)
M.G. Park, H.S. Koo, B. Lee, Characteristics of testosterone deficiency syndrome in men with chronic kidney disease and male renal transplant recipients: a cross-sectional study. Transplant. Proc. 45, 2970–2974 (2013). https://doi.org/10.1016/j.transproceeding
R. Peces, M. de la Torre, J.M. Urra, Pituitary-testicular function in cyclosporin-treated renal transplant patients. Nephrol. Dial. Transplant. 9, 1453–1455 (1994)
A.R. Prem, S.V. Punekar, M. Kalpana, A.R. Kelkar, V.N. Acharya, Male reproductive function in uraemia: efficacy of haemodialysis and renal transplantation. Brit J. Urol. 78, 635–638 (1996)
V. Tondolo, F. Citterio, N. Panocchia, G. Nanni, E. Favi, A. Brescia, M. Castagneto, Gonadal function and immunosuppressive therapy after renal transplantation. Transpl. Proc. 37, 1915–1917 (2005). https://doi.org/10.1016/j.transproceed.2005.04.004
R. Yadav, S.N. Mehta, A. Kumar, S. Guleria, V. Seenu, S.C. Tiwari, A prospective analysis of testicular androgenic function in recipients of a renal allograft. Int. J. Urolol. Nephrol. 40, 397–403 (2008). https://doi.org/10.1007/s11255-007-9277-8
H. Colak, I. Sert, Y. Kurtulmus, C. Karaca, H. Toz, S. Kursat, The relation between serum testosterone levels and cardiovascular risk factors in patients with kidney transplantation and chronic kidney disease. Saudi J. Kid Dis. Transplant. 25, 951–959 (2014)
L. Tauchmanovà, R. Carrano, M. Sabbatini, M. De Rosa, F. Orio, S. Palomba, T. Cascella, G. Lombardi, S. Federico, A. Colao, Hypothalamic-pituitary-gonadal axis function after successful kidney transplantation in men and women. Hum. Reprod. 19, 867–873 (2004). https://doi.org/10.1093/humrep/deh192
W. Reinhardt, D. Patschan, F. Pietruck, T. Philipp, O.E. Janssen, K.I. Mann, F. Jockenhoevel, O. Witzke, Free androgen index is superior to total testosterone for short-term assessment of the gonadal axis after renal transplantation. Horm. Res. 64, 248–252 (2005). https://doi.org/10.1159/000089292
A. Vermeulen, L. Verdonck, J.M. Kaufman, A critical evaluation of simple methods for the estimation of free testosterone in serum. J. Clin. Endocrinol. Metab. 84, 3666–3672 (1999)
A.S. Levey, L. Inker, J. Coresh, GFR estimation from physiology to public health. Am. J. Kidn. Dis. 63, 820–834 (2014)
C. Wang, E. Nieschlag, R. Swerdloff, H.M. Behre, W.J. Hellstrom, L.J. Gooren, J.M. Kaufman, J.J. Legros, B. Lunenfeld, A. Morales, J.E. Morley, C. Schulman, I.M. Thompson, W. Weidner, F.C. Wu, Investigation, treatment and monitoring of late-onset hypogonadism in males: ISA, ISSAM, EAU, EAA and ASA recommendations. Eur. J. Endocrinol. 159, 507–514 (2008). https://doi.org/10.1530/EJE-08-0601
R. Blake, S. Rajguru, G. Nolan, B. Ahluwalia, Dexamethasone suppresses sex-hormone binding globulin. Fertil. Steril. 49, 66–70 (1988)
V.S. Lim, V.S. Fang, Gonadal dysfunction in uremic men. A study of the hypothalamo-pituitary-testicular axis before and after renal transplantation. Am. J. Med. 58, 655–662 (1975)
D.J. Handelsman, B. Yeap, L. Flicker, S. Martin, G.A. Wittert, L.P. Ly, Age-specific population centiles for androgen status in men. Eur. J. Endocrinol. 173, 809–817 (2015). https://doi.org/10.1530/EJE-15-0380
B. Lapauw, S. Goemaere, H. Zmierczak, I. Van Pottelbergh, A. Mahmoud, Y. Taes, D. De Bacquer, S. Vansteelandt, J.M. Kaufman, The decline of serum testosterone levels in community-dwelling men over 70 years of age: descriptive data and predictors of longitudinal changes. Eur. J. Endocrinol. 159, 459–468 (2008). https://doi.org/10.1530/EJE-07-0873
E. Orwoll, L.C. Lambert, L.M. Marshall, K. Phipps, J. Blank, E. Barrett-Connor, J. Cauley, K. Ensrud, S. Cummings, Testosterone and estradiol among older men. J. Clin. Endocrinol. Metab. 91, 1336–1344 (2006)
J.S. Brand, I. van der Tweel, D.E. Grobbee, M.H. Emmelot-Vonk, Y.T.Testosterone van der Schouw, Sex hormone-binding globulin and the metabolic syndrome: a systematic review and meta-analysis of observational studies. Int. J. Epidemiol. 40, 189–207 (2011). https://doi.org/10.1093
L. Vandenput, D. Mellström, M.K. Karlsson, E. Orwoll, F. Labrie, O. Ljunggren, C. Ohlsson, Serum estradiol is associated with lean mass in elderly Swedish men. Eur. J. Endocrino1 62, 737–745 (2010). https://doi.org/10.1530/EJE-09-0696
G. Kantarci, S. Sahin, A.R. Uras, H. Ergin, Effects of different calcineurin inhibitors on sex hormone levels in transplanted male patients. No difference CyA vs Tacrolimus. Transpl. Proc. 361, 78–79 (2004)
J.A. Talbot, R.S. Rodger, W.R. Robertson, Pulsatile bioactive luteinizing hormone secretion in men with chronic renal failure and following renal transplantation. Nephron 56, 66–72 (1990)
A. Vermeulen, J.M. Kaufman, S. Goemaere, I. van Pottelberg, Estradiol in elderly men. Aging Male. 5, 98–102 (2002)
S.R. Holdsworth, D.M. de Kretser, R.C. Atkins, A comparison of hemodialysis and transplantation in reversing the uremic disturbance of male reproductive function. Clin. Nephrol. 10, 146–150 (1978)
M.C. Fung, G.C. Wah, W.D. Odell, Effect of prolactin on luteinizing hormone–stimulated testosterone in isolated perfused rat testis. J. Androl. 10, 37–42 (1989)
G.D. Sievertsen, V.S. Lim, C. Nakawatase, L.A. Frohman, Metabolic clearance and secretion rates of human prolactin in normal subjects and in patients with chronic renal failure. J. Clin. Endocrinol. Metab. 50, 846–852 (1980)
R. Peces, C. Horcajada, J.M. López-Novoa, M.A. Frutos, S. Casado, L. Hernando, Hyperprolactinemia in chronic renal failure: impaired responsiveness to stimulation and suppression. Normalization after transplantation. Nephron 28, 11–16 (1981)
I.T. Huhtaniemi, A. Tajar, D.M. Lee, T.W. O’Neill, J.D. Finn, G. Bartfai, S. Boonen, F.F. Casanueva, A. Giwercman, T.S. Han, K. Kula, F. Labrie, M.E. Lean, N. Pendleton, M. Punab, A.J. Silman, D. Vanderschueren, G. Forti, F.C. Wu; EMAS Group, Comparison of serum testosterone and estradiol measurements in 3174 European men using platform immunoassay and mass spectrometry; relevance for the diagnostics in aging men. Eur. J. Endocrinol. 166, 983–991 (2012)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Reinhardt, W., Kübber, H., Dolff, S. et al. Rapid recovery of hypogonadism in male patients with end stage renal disease after renal transplantation. Endocrine 60, 159–166 (2018). https://doi.org/10.1007/s12020-018-1543-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-018-1543-2