Abstract
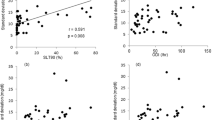
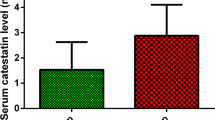
Obstructive sleep apnea (OSA) has been associated with dysregulation of the hypothalamic–pituitary–adrenal axis and alterations in glucose metabolism with increased risk for type 2 diabetes. The aim of the current study was to compare morning plasma cortisol levels and glucose metabolism parameters between moderate (apnea–hypopnea index (AHI): 15–30 events/h) and severe OSA patients (AHI >30 events/h), with respective controls. A total of 56 male OSA patients, 24 moderate (AHI = 21.1 ± 5.3) and 32 severe (AHI = 49.7 ± 18.1), underwent a full-night polysomnography, oral glucose tolerance test (OGTT), and measurement of morning plasma cortisol levels. These groups were compared to 20 matched subjects in a control group. Morning plasma cortisol levels were statistically lower in severe OSA group than in moderate OSA and control groups (303.7 ± 93.5 vs. 423.9 ± 145.1 vs. 417.5 ± 99.8 pmol/L, P < 0.001). Significant negative correlations were found between morning plasma cortisol levels and AHI (r = −0.444, P = 0.002), as well as oxygen desaturation index (r = −0.381, P = 0.011). Fasting plasma glucose (5.0 ± 0.5 vs. 5.4 ± 0.7 vs. 4.9 ± 0.6 mmol/L, P = 0.009) was higher in the severe OSA group compared to moderate OSA and controls. Homeostasis model assessment insulin resistance (HOMA-IR) was higher in the severe OSA group compared to moderate OSA and controls (4.6 ± 3.7 vs. 2.7 ± 2.0 and 2.2 ± 1.8, respectively, P = 0.006). In conclusion, our study showed that morning plasma cortisol levels measured at 8 a.m. were significantly lower in severe OSA patients than those in moderate OSA group and controls. Morning plasma cortisol levels showed a negative correlation with AHI and oxygen desaturation index. Additionally, this study confirmed the evidence of glucose metabolism impairment in moderate and severe OSA patients, with more pronounced effect in the severe OSA patients group.


Similar content being viewed by others
References
A.S. Jordan, D.G. McSharry, A. Malhorta, Adult obstructive sleep apnoea. Lancet 383, 736–747 (2014)
C. Guilleminault, L. Eldridge, A. Tilkian, B. Simmons, W. Dement, Sleep apnoea syndrome due to upper airway obstruction. Arch. Intern. Med. 137, 296–300 (1997)
W.T. McNicholas, Sleep-related breathing disorders: nosological classification, definitions, epidemiology, in Sleep Medicine Textbook, ed. by C. Bassetti, Z. Dogas, P. Peigneux (European Sleep Research Society, Regensburg, 2014), pp. 215–220
J.A. Dempsey, S.C. Veasey, B.J. Morgan, C.P. O’Donnell, Pathophysiology of sleep apnea. Physiol. Rev. 90, 47–112 (2010)
K. Stamatakis, M.H. Sanders, B. Caffo et al., Fasting glycemia in sleep disordered breathing: lowering the threshold on oxyhemoglobin desaturation. Sleep 31, 1018–1024 (2008)
J.L. Pepin, J.C. Borel, A.L. Borel, P. Levy, R. Tamisier, Sleep-related breathing disorders: comorbidities and special populations, in Sleep Medicine Textbook, ed. by C. Bassetti, Z. Dogas, P. Peigneux (European Sleep Research Society, Regensburg, 2014), pp. 251–258
M.L. Tomfohr, K.M. Edwards, J.E. Dimsdale, Is obstructive sleep apnea associated with cortisol levels? A systematic review of the research evidence. Sleep Med. Rev. 16, 243–249 (2012)
N.A. Dewan, F.J. Nieto, V.K. Somers, Intermittent hypoxemia and OSA: implications for comorbidities. Chest 147, 266–274 (2015)
S. Khani, J.A. Tayek, Cortisol increases gluconeogenesis in humans: its role in the metabolic syndrome. Clin. Sci. 101, 739–747 (2001)
Z. Lattova, M. Keckeis, E. Maurovich-Horvat et al., The stress hormone system in various sleep disorders. J. Psychiatr. Res. 45, 1223–1228 (2011)
E. Crawford-Achour, M. Saint Martin, F. Roche, Stress hormones in obstructive sleep apnea complications: the role of cortisol. Sleep Med. 15, 3–4 (2014)
S.L. Appleton, A. Vakulin, R.D. McEvoy et al., Nocturnal hypoxemia and severe obstructive sleep apnea are associated with incident type 2 diabetes in a population cohort of men. J. Clin. Sleep Med. 11, 609–614 (2015)
N.H. Kim, N.H. Cho, C.H. Yun et al., Association of obstructive sleep apnea and glucose metabolism in subjects with or without obesity. Diabetes Care 36, 3909–3915 (2013)
S. Seicean, H.L. Kirchner, D.J. Gottlieb et al., Sleep-disordered breathing and impaired glucose metabolism in normal-weight and overweight/obese individuals. Diabetes Care 31, 1001–1006 (2008)
N.M. Punjabi, V.Y. Polotsky, Disorders of glucose metabolism in sleep apnea. J. Appl. Physiol. 99, 1998–2007 (2005)
A.A. Tahrani, A. Ali, M.J. Stevens, Obstructive sleep apnoea and diabetes: an update. Curr. Opin. Pulm. Med. 19, 631–638 (2013)
X. Wang, Y. Bi, Q. Zhang, F. Pan, Obstructive sleep apnea and the risk of type 2 diabetes: a meta-analysis of prospective cohort studies. Respirology 18, 140–146 (2013)
L.F. Drager, S.M. Togeiro, V.Y. Polotsky, G. Lorenzi-Filho, Obstructive sleep apnea: a cardiovascular risk in obesity and metabolic syndrome. J. Am. Coll. Cardiol. 62, 569–576 (2013)
B.D. Kent, L. Grote, S. Ryan et al., Diabetes mellitus prevalence and control in sleep disordered breathing: the European sleep apnea cohort (ESADA) study. Chest 146, 982–990 (2014)
The Report of an American Academy of Sleep Medicine Task Force, Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep 22, 667–689 (1999)
L.J. Epstein, D. Kristo, P.J. Strollo Jr et al., Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J. Clin. Sleep Med. 5, 263–276 (2009)
R. Pecotic, I.P. Dodig, M. Valic, N. Ivkovic, Z. Dogas, The evaluation of the Croatian version of the Epworth sleepiness scale and STOP questionnaire as screening tools for obstructive sleep apnea syndrome. Sleep Breath. 16, 793–802 (2012)
J. Fischer, Z. Dogas, C.L. Bassetti et al., Standard procedures for adults in accredited sleep medicine centres in Europe. J. Sleep Res. 21, 357–368 (2012)
C.A. Kushida, M.R. Littner, T. Morgenthaler et al., Practice parameters for the indications for polysomnography and related procedures: an update for 2005. Sleep 28, 449–521 (2005)
American Diabetes Association, Diagnosis and classification of diabetes mellitus. Diabetes Care 35, 64–71 (2012)
American Diabetes Association, Standards of medical care in diabetes—2014. Diabetes Care 37, 14–80 (2014)
D.R. Matthews, J.P. Hosker, A.S. Rudenski et al., Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28, 412–419 (1985)
H. Raff, S.L. Ettema, D.C. Eastwood, B.T. Woodson, Salivary cortisol in obstructive sleep apnea: the effect of CPAP. Endocrine 40, 137–139 (2011)
C.M. Ghiciuc, L.C. Dima Cozma, R.M. Bercea et al., Restoring the salivary cortisol awakening response through nasal continuous positive airway pressure therapy in obstructive sleep apnea. Chronobiol. Int. 30, 1024–1031 (2013)
B. Panaree, M. Chantana, S. Wasana, N. Chairat, Effects of obstructive sleep apnea on serum brain-derived neurotrophic factor protein, cortisol, and lipid levels. Sleep Breath. 15, 649–656 (2011)
G. Malakasioti, E.I. Alexopoulos, V. Varlami et al., Low morning serum cortisol levels in children with tonsillar hypertrophy and moderate-to-severe OSA. Sleep 36, 1349–1354 (2013)
K.M. Edwards, R. Kamat, L.M. Tomfohr, S. Ancoli-Israel, J.E. Dimsdale, Obstructive sleep apnea and neurocognitive performance: the role of cortisol. Sleep Med. 15, 27–32 (2014)
G. Carneiro, S.M. Togeiro, L.F. Hayashi et al., Effect of continuous positive airway pressure therapy on hypothalamic–pituitary–adrenal axis function and 24-h blood pressure profile in obese men with obstructive sleep apnea syndrome. Am. J. Physiol. Endocrinol. Metab. 295, E380–E384 (2008)
Z. Karaca, S. Ismailogullari, S. Korkmaz et al., Obstructive sleep apnoea syndrome is associated with relative hypocortisolemia and decreased hypothalamo–pituitary–adrenal axis response to 1 and 250 μg ACTH and glucagon stimulation tests. Sleep Med. 14, 160–164 (2013)
C. Heim, U. Ehlert, D.H. Hellhammer, The potential role of hypocortisolism in the pathophysiology of stress-related bodily disorders. Psychoneuroendocrinology 25, 1–35 (2000)
G. Tirabassi, M. Boscaro, G. Arnaldi, Harmful effects of functional hypercortisolism: a working hypothesis. Endocrine 46, 370–386 (2014)
T.M. Buckley, A.F. Schatzberg, On the interactions of the hypothalamic–pituitary–adrenal (HPA) axis and sleep: normal HPA axis activity and circadian rhythm, exemplary sleep disorders. J. Clin. Endocrinol. Metab. 90, 3106–3114 (2005)
L. Plat, R. Leproult, M. L’Hermite-Baleriaux et al., Metabolic effects of short-term elevations of plasma cortisol are more pronounced in the evening than in the morning. J. Clin. Endocrinol. Metab. 84, 3082–3092 (1999)
S. Dube, B.J. Norby, V. Pattan, R.E. Carter, A. Basu, R. Basu, 11β-Hydroxysteroid dehydrogenase types 1 and 2 activity in subcutaneous adipose tissue in humans: implications in obesity and diabetes. J. Clin. Endocrinol. Metab. 100, E70–E76 (2014)
E.A. Lucassen, G. Cizza, The hypothalamic–pituitary–adrenal axis, obesity, and chronic stress exposure: sleep and the HPA axis in obesity. Curr. Obes. Rep. 1, 208–215 (2012)
D.M. Nathan, M.B. Davidson, R.A. DeFronzo et al., Impaired fasting glucose and impaired glucose tolerance: implications for care. Diabetes Care 30, 753–759 (2007)
D. Fisher, G. Pillar, A. Malhotra, N. Peled, P. Lavie, Long-term follow-up of untreated patients with sleep apnoea syndrome. Respir. Med. 96, 337–343 (2002)
A. Dawson, S.L. Abel, R.T. Loving et al., CPAP therapy of obstructive sleep apnea in type 2 diabetics improves glycemic control during sleep. J. Clin. Sleep Med. 4, 538–542 (2008)
T. Galic, J. Bozic, N. Ivkovic, T. Kurir Ticinovic, Z. Dogas, Effects of mandibular advancement device treatment on arterial stiffness and glucose metabolism in patients with mild to moderate obstructive sleep apnea: a prospective 1 year study. Sleep Breath. (2015). doi:10.1007/s11325-015-1186-y
E. Tasali, B. Mokhlesi, E. Van Cauter, Obstructive sleep apnea and type 2 diabetes: interacting epidemics. Chest 133, 496–506 (2008)
Funding
This work was funded by the Croatian Science Foundation Grant #2013-11-5935. This study was performed at the University of Split School of Medicine, Split, Croatia. The funding sources did not have any involvement in study design, writing of the manuscript, and the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Bozic, J., Galic, T., Supe-Domic, D. et al. Morning cortisol levels and glucose metabolism parameters in moderate and severe obstructive sleep apnea patients. Endocrine 53, 730–739 (2016). https://doi.org/10.1007/s12020-016-0925-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-016-0925-6