Abstract
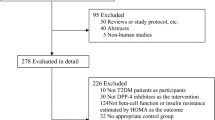
The aim of this study is to compare the efficacy of dipeptidyl peptidase-4 (DPP-4) inhibitor treatment with α-glucosidase inhibitor (AGI) treatment in patients with type 2 diabetes through a meta-analysis. Studies were identified by a literature search of Medline, Embase, and others from the time that recording commenced until December 2014. The meta-analysis was performed by computing the weighted mean difference (WMD) and 95 % confidence interval (CI) for a change from baseline to the study endpoint for DPP-4 inhibitors versus AGIs. Nine randomized controlled trial were judged to be appropriate for inclusion in the meta-analysis. One thousand and forty-six patients were treated with a DPP-4 inhibitor, while 929 patients were treated with AGI treatment; the groups had a comparable baseline body mass index of 25.5 ± 1.3 kg/m2 and mean baseline HbA1c of 7.83 ± 0.53 %. Treatment with DPP-4 inhibitors led to a significantly greater change from baseline in the HbA1c levels (WMD −0.30 %; 95 % CI −0.47 to −0.13 %, p < 0.001) and fasting plasma glucose levels (WMD −0.50 mmol/L; 95 % CI −0.89 to −0.11 mmol/L, p = 0.01) compared with AGI treatment. Compared with AGIs, treatment with DPP-4 inhibitors was associated with a significantly greater increase in the weight change from baseline (WMD 0.89 kg; 95 % CI 0.53–1.25, p < 0.001). Treatment with DPP-4 inhibitors was associated with a significantly greater increase in the fasting insulin level from baseline (WMD 0.63 µU/mL; 95 % CI 0.35–0.90 µU/mL, p < 0.001). DPP-4 inhibitors significantly improved homeostatic model assessment for β-cell function in type 2 diabetes patients compared with AGI treatment (WMD 5.43; 95 % CI 1.01–9.85, p = 0.02). DPP-4 inhibitors were associated with a significantly greater decrease in the cholesterol (CHO) level (WMD −0.19 mmol/L; 95 % CI −0.19 to −0.19 mmol/L, p < 0.001) and a significantly greater decrease in the low-density lipoprotein cholesterol (LDL-C) level (WMD −0.16 mmol/L; 95 % CI −0.26 to −0.05 mmol/L, p = 0.003). Compared with AGIs (813 participants), treatment with DPP-4 inhibitors (1031 participants) was associated with a significantly lower incidence of drug-related adverse event (OR 0.48; 95 % CI 0.36–0.64, p < 0.0001). The efficacy of glucose control and improvement of β-cell function, as well as total CHO and LDL-C decreases, in DPP-4 inhibitor treatment were superior to those with AGI treatment, and there was a lower incidence of drug-related AE.




Similar content being viewed by others
References
J.F. Habener, Insulinotropic glucagon-like peptides, in Diabetes Mellitus: A Fundamental and Clinical Text, 2nd edn., ed. by D. LeRoith, S.I. Taylor, J.M. Olefsky (Lippincott Williams & Wilkins, Philadelphia, 2000)
K. Aaboe, T. Krarup, S. Madsbad, J.J. Holst, GLP-1: physiological effects and potential therapeutic applications. Diabetes Obes. Metab. 10, 994–1003 (2008)
A.J. Garber, Incretin effects on β-cell function, replication, and mass: the human perspective. Diabetes Care 34(Suppl 2), S258–S263 (2011)
F.A. Van de Laar, P.L. Lucassen, R.P. Akkermans, E.H. Van de Lisdonk, G.E. Rutten, C. Van Weel, Alpha-glucosidase inhibitors for type 2 diabetes mellitus. Cochrane Database Syst. Rev. 2, CD003639 (2005)
A. Karasik, P. Aschner, H. Katzeff, M.J. Davies, P.P. Stein, Sitagliptin, a DPP-4 inhibitor for the treatment of patients with type 2 diabetes: a review of recent clinical trials. Curr. Med. Res. Opin. 24, 489–496 (2008)
A.R. Jadad, R.A. Moore, D. Carroll, C. Jenkinson, D.J. Reynolds, D.J. Gavaghan, H.J. McQuay, Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control. Clin. Trials 17, 1–12 (1996)
A. Liberati, D.G. Altman, J. Tetzlaff, C. Mulrow, P.C. Gøtzsche, J.P. Ioannidis, M. Clarke, P.J. Devereaux, J. Kleijnen, D. Moher, The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 6, e1000100 (2009)
Y. Seino, T. Fujita, S. Hiroi, M. Hirayama, K. Kaku, Efficacy and safety of alogliptin in Japanese patients with type 2 diabetes mellitus: a randomized, double-blind, dose-ranging comparison with placebo, followed by a long-term extension study. Curr. Med. Res. Opin. 9, 1781–1792 (2011)
R. Kawamori, N. Inagaki, E. Araki, H. Watada, N. Hayashi, Y. Horie, A. Sarashina, Y. Gong, M. von Eynatten, H.J. Woerle, K.A. Dugi, Linagliptin monotherapy provides superior glycaemic control versus placebo or voglibose with comparable safety in Japanese patients with type 2 diabetes: a randomized, placebo and active comparator-controlled, double-blind study. Diabetes Obes. Metab. 14, 348–357 (2012)
K. Nakamura, H. Oe, H. Kihara, K. Shimada, S. Fukuda, K. Watanabe, T. Takagi, K. Yunoki, T. Miyoshi, K. Hirata, J. Yoshikawa, H. Ito, DPP-4 inhibitor and alpha-glucosidase inhibitor equally improve endothelial function in patients with type 2 diabetes: EDGE study. Cardiovasc. Diabetol. 13, 110–120 (2014)
Y. Iwamoto, N. Tajima, T. Kadowaki, K. Nonaka, T. Taniguchi, M. Nishii, J.M. Amatruda, J.C. Arjona Ferreira, Efficacy and safety of sitagliptin monotherapy compared with voglibose in Japanese patients with type 2 diabetes: a randomized, double-blind trial. Diabetes Obes. Metab. 12, 613–622 (2010)
C. Pan, W. Yang, J.P. Barona, Y. Wang, M. Niggli, P. Mohideen, Y. Wang, J.E. Foley, Comparison of vildagliptin and acarbose monotherapy in patients with Type 2 diabetes: a 24-week, double-blind, randomized trial. Diabetes Med. 25, 435–441 (2008)
Y. Iwamoto, A. Kashiwagi, N. Yamada, S. Terao, N. Mimori, M. Suzuki, H. Tachibana, Efficacy and safety of vildagliptin and voglibose in Japanese patients with type 2 diabetes: a 12-week, randomized, double-blind, active-controlled study. Diabetes Obes. Metab. 12, 700–708 (2010)
K. Okada, H. Yagyu, K. Kotani, H. Yamazaki, K. Ozaki, M. Takahashi, S. Nagashima, J. Osuga, S. Ishibashi, Effects of miglitol versus sitagliptin on postprandial glucose and lipoprotein metabolism in patients with type 2 diabetes mellitus. Endocr. J. 60(7), 913–922 (2013)
A. Mikada, T. Narita, H. Yokoyama, R. Yamashita, Y. Horikawa, K. Tsukiyama, Y. Yamada, Effects of miglitol, sitagliptin, and initial combination therapy with both on plasma incretin responses to a mixed meal and visceral fat in over-weight Japanese patients with type 2 diabetes. “the MASTER randomized, controlled trial”. Diabetes Res. Clin. Pract. 106(3), 538–547 (2014)
K. Kobayashi, H. Yokoh, Y. Sato, M. Takemoto, D. Uchida, A. Kanatsuka, N. Kuribayashi, T. Terano, N. Hashimoto, K. Sakurai, H. Hanaoka, K. Ishikawa, S. Onishi, K. Yokote, SUCCESS Study Group, Efficacy and safety of the dipeptidyl peptidase-4 inhibitor sitagliptin compared with α-glucosidase inhibitor in Japanese patients with type 2 diabetes inadequately controlled on sulfonylurea alone (SUCCESS-2): a multicenter, randomized, open-label, non-inferiority trial. Diabetes Obes. Metab. 16(8), 761–765 (2014)
X. Cai, X. Han, Y. Luo, L. Ji, Comparisons of the efficacy of alpha glucosidase inhibitors on type 2 diabetes patients between Asian and Caucasian. PLoS ONE 8(11), e79421 (2013)
X. Cai, X. Han, Y. Luo, L. Ji, Efficacy of dipeptidyl-peptidase-4 inhibitors and impact on β-cell function in Asian and Caucasian type 2 diabetes mellitus patients: a meta-analysis. J Diabetes. 7, 347–359 (2015)
G.A. Herman, P.P. Stein, N.A. Thornberry, J.A. Wagner, Dipeptidyl peptidase-4 inhibitors for the treatment of type 2 diabetes: focus on sitagliptin. Clin. Pharmacol. Ther. 81, 761–767 (2007)
M. Monami, V. Vitale, M.L. Ambrosio, N. Bartoli, G. Toffanello, B. Ragghianti, F. Monami, E. Mannucci, N. Marchionni, Effects on lipid profile of dipeptidyl peptidase 4 inhibitors, pioglitazone, acarbose, and sulfonylureas: meta-analysis of placebo-controlled trials. Adv. Ther. 29(9), 736–746 (2012)
M. Monami, C. Lamanna, C.M. Desideri, E. Mannucci, DPP-4 inhibitors and lipids: systematic review and meta-analysis. Adv. Ther. 29(1), 14–25 (2012)
X. Dai, H. Wang, Z. Jing, P. Fu, The effect of a dual combination of noninsulin antidiabetic drugs on lipids: a systematic review and network meta-analysis. Curr. Med. Res. Opin. 30(9), 1777–1786 (2014)
J. Hsieh, C. Longuet, C.L. Baker, B. Qin, L.M. Federico, D.J. Drucker, K. Adeli, The glucagon-like peptide 1 receptor is essential for postprandial lipoprotein synthesis and secretion in hamsters and mice. Diabetologia 53, 552–561 (2010)
L. Juntti-Berggren, J. Pigon, F. Karpe, A. Hamsten, M. Gutniak, L. Vignati, S. Efendic, The antidiabetogenic effect of GLP-1 is maintained during a 7-day treatment period and improves diabetic dyslipoproteinemia in NIDDM patients. Diabetes Care 19, 1200–1206 (1996)
F. Giorgino, A. Leonardini, A. Natalicchio, L. Laviola, Multifactorial intervention in Type 2 diabetes: the promise of incretin-based therapies. J. Endocrinol. Invest. 34, 69–77 (2011)
A. Barnett, J. Allsworth, K. Jameson, R. Mann, A review of the effects of antihyperglycaemic agents on body weight: the potential of incretin targeted therapies. Curr. Med. Res. Opin. 23, 1493–1507 (2007)
K. Miyawaki, Y. Yamada, N. Ban, Y. Ihara, K. Tsukiyama, H. Zhou, S. Fujimoto, A. Oku, K. Tsuda, S. Toyokuni, H. Hiai, W. Mizunoya, T. Fushiki, J.J. Holst, M. Makino, A. Tashita, Y. Kobara, Y. Tsubamoto, T. Jinnouchi, T. Jomori, Y. Seino, Inhibition of gastric inhibitory polypeptide signaling prevents obesity. Nat. Med. 8, 738–742 (2002)
P.L. McClean, N. Irwin, R.S. Cassidy, J.J. Holst, V.A. Gault, P.R. Flatt, GIP receptor antagonism reverses obesity, insulin resistance, and associated metabolic disturbances induced in mice by prolonged consumption of high-fat diet. Am. J. Physiol. Endocrinol. Metab. 293, E1746–E1755 (2007)
Acknowledgments
This meta-analysis was supported by the National High-technology Research and Development Program of China (863 Program 2012AA02A509) and National Natural Science Foundation of China (NSFC) (81000334). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. We are grateful to all doctors and staff members for their practical work during the study at Peking University People’s Hospital Endocrinology and Metabolism Department.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cai, X., Yang, W., Zhou, L. et al. Comparisons of the efficacy of glucose control, lipid profile, and β-cell function between DPP-4 inhibitors and AGI treatment in type 2 diabetes patients: a meta-analysis. Endocrine 50, 590–597 (2015). https://doi.org/10.1007/s12020-015-0653-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-015-0653-3