Abstract
Vitamin D status assessed by serum 25-hydroxyvitamin D levels (25(OH)D) has been shown to be inversely associated with insulin resistance. The underlying basis for such association is less clear. In the present study, we assessed the prevalence of inadequate vitamin D levels and its relationship to glucose tolerance status and circulating adiponectin in healthy Thai population. The cohort of 246 subjects was classified into two groups according to 75 g oral glucose tolerance test (OGTT) results. There were 86 subjects and 160 subjects in normal glucose tolerance group (NGT) and abnormal glucose tolerance group (AGT), respectively. Anthropometric variables were recorded for each individual. Fasting blood samples were assayed for 25(OH)D, adiponectin, glucose, and insulin levels. Insulin resistance (HOMA-IR) and insulin secretion index (HOMA-B) were calculated by the homeostasis model assessment. Pearson and partial correlation analyses were performed. There were 35 males and 211 females with a mean age of 62.4 ± 7.2 years in this study. The mean levels of 25(OH)D were 21.4 ± 6.6 ng/ml. The prevalence of vitamin D deficiency defined by 25(OH)D levels less than 20 ng/ml and vitamin D inadequacy defined by 25(OH)D levels less than 30 ng/ml were 44.3 and 91.9%, respectively. The mean levels of 25(OH)D obtained from samples collected in the rainy season (19.4 ± 4.6 ng/ml) were significantly lower than those collected in the winter (22.6 ± 8.3 ng/ml) and summer period (23.1 ± 4.6 ng/ml). AGT subjects had slightly lower average 25(OH)D levels than the NGT group (21.0 ± 6.8 vs. 22.1 ± 6.2 ng/ml, P = 0.09). 25(OH)D levels were positively associated with adiponectin levels (r = 0.20, P < 0.05) and negatively associated with HOMA-IR and BMI (r = −0.22, P < 0.01 and r = −0.22, P < 0.01, respectively) only in AGT subjects. An independent association between 25(OH)D and adiponectin levels was demonstrated after controlling for BMI (r = 0.17, P < 0.05). High prevalence of vitamin D inadequacy and seasonal variation of vitamin D status are found in Thai population. We demonstrated an association between insufficient vitamin D status and lower circulating adiponectin in subjects with abnormal glucose tolerance independently of adiposity which may indicate the role of adiponectin as a link between vitamin D status and insulin resistance.
Similar content being viewed by others
Introduction
The well established function of vitamin D is to maintain calcium and phosphorus homeostasis as well as promote bone mineralization. During childhood, vitamin D deficiency can cause growth retardation and skeletal deformities. Besides osteomalacia, vitamin D deficiency in adult can exacerbate osteopenia or osteoporosis and increase the risk of fractures due to the associated secondary hyperparathyroidism [1]. 25-Hydroxyvitamin D (25(OH)D) levels are inversely associated with parathyroid hormone levels until the former reach 30–40 ng/ml, at which point parathyroid hormone levels begin to level off [2–4]. Furthermore, intestinal calcium transport increased by 45–65% in women when 25(OH)D levels were increased from an average of 20–32 ng/ml [5]. Given such data, most experts define a level of 25(OH)D of 21–29 ng/ml as relative insufficiency of vitamin D and 25(OH)D less than 20 ng/ml as deficiency of vitamin D [6]. With these definitions, vitamin D deficiency has become highly prevalent for all age groups in the United States and Europe. Likewise, an international study found that 71% of postmenopausal women with osteoporosis in Eastern Asia had vitamin D inadequacy [7].
Discovery of the presence of vitamin D receptors in numerous tissues has provided new insights into the nonskeletal function of this vitamin. Accumulating evidences suggested that the inadequacy of vitamin D may play role in the development of type 2 diabetes [8–10]. Vitamin D status has also been found to be a modifier of diabetes risk in that the levels of 25(OH)D are inversely associated with insulin resistance [10, 11]. The underlying basis for such association is less clear. One of the hypothesis may be related to adiponectin which is related to insulin sensitivity [12]. Although it is well established that patients with type 2 diabetes have low adiponectin levels [13], there is no existing data with regard to the relationship between vitamin D status and adiponectin. It is therefore, the objectives of our study to determine the relationship between vitamin D status and circulating adiponectin to assess its role as one of the factors mediating influence of vitamin D on insulin sensitivity.
Results
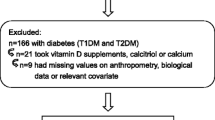
Among 246 subjects, 35 (14%) were males and 211 (85.8%) were females. The mean age was 62.4 ± 7.2 years (age ± SD). With regard to glucose tolerance status, 86 subjects had normal glucose tolerance group (NGT) and 160 subjects had abnormal glucose tolerance group (AGT). Subjects in the NGT group had lower FPG levels, BMI, WC, waist hip ratio (WHR), and insulin resistance (HOMA-IR) and had higher insulin secretion index (HOMA-B), disposition index, adiponectin, and HDL-C than those with AGT as shown in Table 1. After controlling for the difference in the gender distribution in subjects with AGT and NGT, the significant difference in adiponectin no longer existed. Likewise, BMI and HOMA-IR did not significantly differ after adjusting for gender. However, the differences in FPG level, WC, WHR, HOMA-B, disposition index, and HDL still existed after gender was taken into account.
Overall the mean levels of 25(OH)D was 21.4 ± 6.6 ng/ml. 25(OH)D in the AGT group was slightly lower than the NGT subjects but did not reach statistical significance (21.0 ± 6.8 vs. 22.1 ± 6.2 ng/ml, P = 0.09). The prevalence of vitamin D deficiency and vitamin D inadequacy were 44.3 and 91.9%, respectively. There was no significant difference in the frequency of vitamin D inadequacy between each group. Mean vitamin D level from blood samples obtained in the rainy season (n = 102, 19.4 ± 4.6 ng/ml) was the lowest and was significantly different from those collected in winter (n = 97, 22.6 ± 8.3 ng/ml, P < 0.05) and summer (n = 47, 23.1 ± 4.6 ng/ml, P < 0.01). The prevalence of vitamin D inadequacy according to different glucose tolerance status and season of sampling was demonstrated in Table 2.
25(OH)D levels were directly correlated to adiponectin levels only in the AGT group (r = 0.20, P < 0.05) and inversely associated with log HOMA-IR and BMI (r = −0.22, P < 0.01 and r = −0.22, P < 0.01, respectively) as shown in Fig. 1. In the NGT group, 25(OH)D levels were not significantly associated with any biochemical and clinical parameters as shown in Table 3. Using partial correlation analysis, the association between 25(OH)D and adiponectin levels still persisted after controlling for BMI (r = 0.17, P < 0.05). The correlation between 25(OH)D and HOMA-IR no longer existed after controlling for adiponectin levels. Adiponectin levels were significantly associated with log HOMA-IR in both AGT and NGT group (r = −0.33, P ≤ 0.01 and r = −0.36, P ≤ 0.01, respectively). There was no correlation between vitamin D status and insulin secretion index in either group.
Discussion
Vitamin D inadequacy is common in western countries [14, 15] particularly during winter when sunlight is insufficient to induce cutaneous vitamin D3 synthesis [16] at latitudes above 37°N or below 37°S. We demonstrated in the present study that vitamin D inadequacy is not uncommon in Thailand despite the geographical location close to the equator. This is in agreement with other previous studies in Thailand which showed the high prevalence of vitamin D inadequacy varied from 32 to 66.3% when using 25(OH)D cutoff levels of 24–30 ng/ml [17–19]. In the present study, we also demonstrated the seasonal variation of vitamin D status in Thai population. Subjects having their blood samples collected in the rainy season showed the highest prevalence of vitamin D inadequacy. Explanations for this observation may be related to the cloudy environment and less sun exposure during this season in addition to the fact that there is less vitamin D fortified food, such as some kinds of milk and yogurts, available in our country. Seasonal variation of vitamin D status has also been revealed in other Asian countries. For examples, healthy Japanese and Taiwanese women who had serum sampled during summer showed 4–7.5 ng/ml higher levels of serum 25(OH)D than those who had serum sampled during winter [20, 21]. Furthermore, significant seasonal variation of serum 25(OH)D was also noted in Korean subjects and the serum 25(OH)D levels also correlated with sunlight exposure especially at 12.00 to 2.00 p.m. as assessed by the time spent outdoors [22]. Nevertheless, none of mentioned countries are as close to the equator as Thailand.
The influence of vitamin D on the risk of diabetes has been suggested. A number of studies including systematic reviews have shown greater insulin sensitivity in subjects who had higher levels of 25(OH)D [11, 23–26]. But whether there is a causal relationship still needs to be established. The finding of the association between vitamin D status and circulating adiponectin independently of adiposity in the present study suggests adiponectin as one of the underlying basis for the inverse association between 25(OH)D levels and insulin resistance. On the other hand, a few recent studies have demonstrated the association between 25(OH)D levels and adiponectin levels [27, 28]. However, after adjustment for sex and BMI, this association was not statistically significant. It is of note that the association between vitamin D status and circulating adiponectin was demonstrated only in subjects with abnormal glucose tolerance. Abnormal glucose tolerance is a proinflammatory state causing reduced adiponectin levels probably through the action of proinflammatory cytokines such as tumor necrotic factor-α and interleukin-1 [12]. Vitamin D possesses anti-inflammation effect and may thus ameliorate the effect of proinflammatory cytokines on circulating adiponectin. Due to the cross-sectional design and small sample size of the present study, our result should be considered preliminary. Further clinical study to directly address the effect of vitamin D supplementation on circulating adiponectin in subjects with type 2 diabetes or impaired glucose tolerance is therefore warrant.
Another mechanism for the relationship between vitamin D status and adiponectin may be related to osteocalcin. 1α,25-dihydroxy vitamin D3 binds to C-terminal domain of vitamin D receptors and enhances osteocalcin gene transcription [29]. More recent evidences showed that uncarboxylated form of osteocalcin regulates glucose homeostasis [30, 31]. Study in osteocalcin knockout mice demonstrated higher plasma glucose compared to wild-type mice [30]. Insulin secretion, insulin sensitivity, glucose tolerance, and energy expenditure were decreased as well. Adiponectin gene expression in adipocytes also declined as did serum adiponectin. Additional data from human study revealed significantly lower serum osteocalcin values in patients with type 2 diabetes compared to healthy person [32, 33], and restoration of glycemic control resulted in increased osteocalcin levels [34, 35]. This data support the hypothesis that osteocalcin is one of the osteoblast hormones that regulates glucose homeostasis and adiponectin expression. It is likely that the lower adiponectin levels found to be associated with inadequate vitamin D status in the present study can be a result of the influence of vitamin D on osteocalcin. In addition, vitamin D affects adipogenesis through vitamin D receptor dependent mechanism [36] and direct action of vitamin in affecting adiponectin transcription in adipocyte cannot be entirely ruled out.
This is a cross-sectional study with a small sample size and each subject was sampled only once in different seasons. Therefore, some of the difference between vitamin D levels can also be related to some difference factors between subjects, such as the usage of sunscreen, the amount of vitamin D intake from food or vitamin supplementation, which we did not have data about these.
In conclusion, we demonstrated in the present study not only a high prevalence of vitamin D inadequacy but also the seasonal variation of vitamin D status in healthy Thai population. An association between insufficient vitamin D status and lower circulating adiponectin in subjects with abnormal glucose tolerance independently of adiposity may indicate the role of adiponectin as a link between vitamin D status and insulin resistance.
Materials and methods
The study was conducted at Ramathibodi Hospital, Mahidol University, Bangkok, Thailand. It was approved by the Institutional Review Board and all participants provided written informed consent prior to the study. Subjects consisting of 246 healthy volunteers with aged at least 50 years were recruited by advertisement for the screening of type 2 diabetes from February 2004 through February 2005. A 75 g oral glucose tolerance test (OGTT) was performed in the morning after an 8 h overnight fast. Blood samples were collected and stored at −80°C until the time of analysis. Glucose levels were measured by hexokinase method at fasting and 2 h post-oral glucose loading. Serum insulin, 25(OH)D, adiponectin levels, and lipid profile were assayed during fasting state. Plasma insulin was measured by immunochemiluminescence method (Diagnostic Products Corp., Los Angeles, CA, USA) using automated machine. Plasma triglyceride (TG), HDL-cholesterol (HDL-C), LDL-cholesterol (LDL-C), and total cholesterol levels were measured by enzymatic method (Dimention RxL, Dadebearing Co. Ltd., New York, USA). Circulating adiponectin was measured as total adiponectin by RIA method (LINCO Research, Missouri, USA). Insulin sensitivity (HOMA-IR) and insulin secretion index (HOMA-B) were assessed by HOMA-2 model. 25(OH)D level was measured with an automated immunochemiluminescence method (Liaison®, DiaSorin, Saluggia, Italy).
Glucose tolerance status was classified according to fasting and 2-h glucose levels. Normal glucose tolerance (NGT) was defined as fasting plasma glucose levels <100 mg/dl and 2-h glucose levels <140 mg/dl, while abnormal glucose tolerance (AGT) was defined as fasting plasma glucose levels ≥100 mg/dl and/or 2-h glucose levels ≥140 mg/dl [37]. In this study, we defined vitamin D inadequacy as 25(OH)D levels less than 30 ng/ml and vitamin D deficiency as 25(OH)D levels less than 20 ng/ml.
Body weight, height were measured following standard procedures. Waist circumference was measured according to the guideline of International Diabetes Federation. None of the subjects received hormonal replacement therapy.
Statistical analysis
Normality of different variables was assessed by Kolmogorov–Smirnov test. HOMA-IR and adiponectin data were log-transformed prior to analysis. Student unpaired t test was used to compare serum 25(OH)D, adiponectin and other metabolic parameters between NGT and AGT groups. ANOVA was performed to compare 25(OH)D levels obtained from different seasons. Pearson and partial correlation analyses of 25(OH)D, adiponectin and metabolic parameters were performed. P-values <0.05 were considered statistically significant.
References
M.F. Holick, N. Engl. J. Med. 357, 266–281 (2007)
M.F. Holick, E.S. Siris, N. Binkley, M.K. Beard, A. Khan, J.T. Katzer, R.A. Petruschke, E. Chen, A.E. de Papp, J. Clin. Endocrinol. Metab. 90, 3215–3224 (2005)
M.K. Thomas, D.M. Lloyd-Jones, R.I. Thadhani, A.C. Shaw, D.J. Deraska, B.T. Kitch, E.C. Vamvakas, I.M. Dick, R.L. Prince, J.S. Finkelstein, N. Engl. J. Med. 338, 777–783 (1998)
M.C. Chapuy, P. Preziosi, M. Maamer, S. Arnaud, P. Galan, S. Hercberg, P.J. Meunier, Osteoporos. Int. 7, 439–443 (1997)
R.P. Heaney, M.S. Dowell, C.A. Hale, A. Bendich, J. Am. Coll. Nutr. 22, 142–146 (2003)
B. Dawson-Hughes, R.P. Heaney, M.F. Holick, P. Lips, P.J. Meunier, R. Vieth, Osteoporos. Int. 16, 713–716 (2005)
S.K. Lim, A.W. Kung, S. Sompongse, S. Soontrapa, K.S. Tsai, Curr. Med. Res. Opin. 24, 99–106 (2008)
C. Mattila, P. Knekt, S. Mannisto, H. Rissanen, M.A. Laaksonen, J. Montonen, A. Reunanen, Diabetes Care 30, 2569–2570 (2007)
W.B. Grant, Prog. Biophys. Mol. Biol. 92, 65–79 (2006)
A.G. Pittas, J. Lau, F.B. Hu, B. Dawson-Hughes, J. Clin. Endocrinol. Metab. 92, 2017–2029 (2007)
K.C. Chiu, A. Chu, V.L. Go, M.F. Saad, Am. J. Clin. Nutr. 79, 820–825 (2004)
T. Kadowaki, T. Yamauchi, N. Kubota, K. Hara, K. Ueki, K. Tobe, J. Clin. Invest. 116, 1784–1792 (2006)
M. Daimon, T. Oizumi, T. Saitoh, W. Kameda, A. Hirata, H. Yamaguchi, H. Ohnuma, M. Igarashi, M. Tominaga, T. Kato, Diabetes Care 26, 2015–2020 (2003)
A. Malabanan, I.E. Veronikis, M.F. Holick, Lancet 351, 805–806 (1998)
V. Tangpricha, E.N. Pearce, T.C. Chen, M.F. Holick, Am. J. Med. 112, 659–662 (2002)
M.F. Holick, Mayo Clin. Proc. 81, 353–373 (2006)
S. Soontrapa, C. Pongchaiyakul, C. Somboonporn, W. Somboonporn, L.O. Chailurkit, J. Med. Assoc. Thai. 84(Suppl 2), S534–S541 (2001)
D. Warodomwichit, R. Leelawattana, N. Luanseng, N. Thammakumpee, J. Med. Assoc. Thai. 85, 990–997 (2002)
S. Soontrapa, L.O. Chailurkit, J. Med. Assoc. Thai. 88(Suppl 5), S17–S20 (2005)
K. Nakamura, M. Nashimoto, M. Yamamoto, Int. J. Biometeorol. 44, 186–189 (2000)
K.S. Tsai, S.H. Hsu, J.P. Cheng, R.S. Yang, Bone 20, 371–374 (1997)
J.H. Kim, S.J. Moon, Int. J. Food Sci. Nutr. 51, 439–451 (2000)
R. Scragg, M. Sowers, C. Bell, Diabetes Care 27, 2813–2818 (2004)
A.M. Borissova, T. Tankova, G. Kirilov, L. Dakovska, R. Kovacheva, Int. J. Clin. Pract. 57, 258–261 (2003)
L. Lind, A. Hanni, H. Lithell, A. Hvarfner, O.H. Sorensen, S. Ljunghall, Am. J. Hypertens. 8, 894–901 (1995)
E. Orwoll, M. Riddle, M. Prince, Am. J. Clin. Nutr. 59, 1083–1087 (1994)
E. Liu, J.B. Meigs, A.G. Pittas, N.M. McKeown, C.D. Economos, S.L. Booth, P.F. Jacques, J. Nutr. 139, 329–334 (2009)
M.H. Gannage-Yared, R. Chedid, S. Khalife, E. Azzi, F. Zoghbi, G. Halaby, Eur. J. Endocrinol. 160, 965–971 (2009)
L. Carvallo, B. Henriquez, J. Olate, A.J. van Wijnen, J.B. Lian, G.S. Stein, S. Onate, J.L. Stein, M. Montecino, J. Steroid Biochem. Mol. Biol. 103, 420–424 (2007)
N.K. Lee, H. Sowa, E. Hinoi, M. Ferron, J.D. Ahn, C. Confavreux, R. Dacquin, P.J. Mee, M.D. McKee, D.Y. Jung, Z. Zhang, J.K. Kim, F. Mauvais-Jarvis, P. Ducy, G. Karsenty, Cell 130, 456–469 (2007)
G. Wolf, Nutr. Rev. 66, 229–233 (2008)
P. Pietschmann, G. Schernthaner, W. Woloszczuk, Diabetologia 31, 892–895 (1988)
H. Dobnig, J.C. Piswanger-Solkner, M. Roth, B. Obermayer-Pietsch, A. Tiran, A. Strele, E. Maier, P. Maritschnegg, C. Sieberer, A. Fahrleitner-Pammer, J. Clin. Endocrinol. Metab. 91, 3355–3363 (2006)
M.T. Rosato, S.H. Schneider, S.A. Shapses, Calcif. Tissue Int. 63, 107–111 (1998)
S. Sayinalp, O. Gedik, Z. Koray, Calcif. Tissue Int. 57, 422–425 (1995)
R.J. Wood, Nutr. Rev. 66, 40–46 (2008)
Diabetes Care 20, 1183–1197 (1997)
Acknowledgment
This study was supported by The Thailand Research Fund.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nimitphong, H., Chanprasertyothin, S., Jongjaroenprasert, W. et al. The association between vitamin D status and circulating adiponectin independent of adiposity in subjects with abnormal glucose tolerance. Endocr 36, 205–210 (2009). https://doi.org/10.1007/s12020-009-9216-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-009-9216-9