Abstract
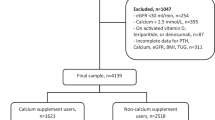
Osteoporosis is a major clinical problem in many autoimmune diseases, including primary biliary cholangitis (PBC), the most common autoimmune liver disease. Osteoporosis is a major cause of fracture and related mortality. However, it remains unclear whether PBC confers a causally risk-increasing effect on osteoporosis. Herein, we aimed to investigate the causal relationship between PBC and osteoporosis and whether the relationship is independent of potential confounders. We performed bidirectional Mendelian randomization (MR) analyses to investigate the association between PBC (8021 cases and 16,489 controls) and osteoporosis in Europeans (the UK Biobank and FinnGen Consortium: 12,787 cases and 726,996 controls). The direct effect of PBC on osteoporosis was estimated using multivariable MR analyses. An independent replication was conducted in East Asians (PBC: 2495 cases and 4283 controls; osteoporosis: 9794 cases and 168,932 controls). Trans-ethnic meta-analysis was performed by pooling the MR estimates of Europeans and East Asians. Inverse-variance weighted analyses revealed that genetic liability to PBC was associated with a higher risk of osteoporosis in Europeans (OR, 1.040; 95% CI, 1.016–1.064; P = 0.001). Furthermore, the causal effect of PBC on osteoporosis persisted after adjusting for BMI, calcium, lipidemic traits, and sex hormones. The causal relationship was further validated in the East Asians (OR, 1.059; 95% CI, 1.023–1.096; P = 0.001). Trans-ethnic meta-analysis confirmed that PBC conferred increased risk on osteoporosis (OR, 1.045; 95% CI, 1.025–1.067; P = 8.17 × 10−6). Our data supports a causal effect of PBC on osteoporosis, and the causality is independent of BMI, calcium, triglycerides, and several sex hormones.
Graphical Abstract




Similar content being viewed by others
Data Availability
See Table S1.
Abbreviations
- BMI:
-
Body mass index
- BAT:
-
Bioavailable testosterone
- CAUSE:
-
Causal analysis using summary effect estimates
- CI:
-
Confidence interval
- GWAS:
-
Genome-wide association study
- IV:
-
Instrumental variable
- IVW:
-
Inverse variance weighted
- LDSC:
-
Linkage disequilibrium score regression
- MR:
-
Mendelian randomization
- MVMR:
-
Multivariable Mendelian randomization
- OR:
-
Odds ratio
- PBC:
-
Primary biliary cholangitis
- PRESSO:
-
Pleiotropy residual sum and outlier
- SHBG:
-
Sex hormone binding globulin
- SNP:
-
Single nucleotide polymorphism
- TT:
-
Total testosterone
- TG:
-
Triglycerides
References
EASL Clinical Practice Guidelines (2017) the diagnosis and management of patients with primary biliary cholangitis. J Hepatol 67(1):145–172
Hirschfield GM, Gershwin ME (2013) The immunobiology and pathophysiology of primary biliary cirrhosis. Annu Rev Pathol 8:303–330
Lleo A et al (2020) Primary biliary cholangitis. Lancet 396(10266):1915–1926
Trivedi PJ, Hirschfield GM (2021) Recent advances in clinical practice: epidemiology of autoimmune liver diseases. Gut 70(10):1989–2003
Zeng N et al (2019) Epidemiology and clinical course of primary biliary cholangitis in the Asia-Pacific region: a systematic review and meta-analysis. Hepatol Int 13(6):788–799
Parés A, Guañabens N (2018) Primary biliary cholangitis and bone disease. Best Pract Res Clin Gastroenterol 34–35:63–70
Chen JL et al (2023) Prevalence and risk factors of osteoporosis detected by dual-energy X-ray absorptiometry among Chinese patients with primary biliary cholangitis. World J Gastroenterol 29(29):4580–4592
Liao CY et al (2018) Increased risk of osteoporosis in patients with primary biliary cirrhosis. PLoS ONE 13(3):e0194418
Schmidt T et al (2018) Disease duration and stage influence bone microstructure in patients with primary biliary cholangitis. J Bone Miner Res 33(6):1011–1019
Guañabens N et al (2005) Severity of cholestasis and advanced histological stage but not menopausal status are the major risk factors for osteoporosis in primary biliary cirrhosis. J Hepatol 42(4):573–577
Guañabens N et al (2010) Low bone mass and severity of cholestasis affect fracture risk in patients with primary biliary cirrhosis. Gastroenterology 138(7):2348–2356
Schönau J et al (2023) Risk of fractures and postfracture mortality in 3980 people with primary biliary cholangitis: a population-based cohort study. J Intern Med 294(2):164–177
Curry SJ et al (2018) Screening for osteoporosis to prevent fractures: US Preventive Services Task Force Recommendation Statement. JAMA 319(24):2521–2531
Pouresmaeili F et al (2018) A comprehensive overview on osteoporosis and its risk factors. Ther Clin Risk Manag 14:2029–2049
Cosman F et al (2014) Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 25(10):2359–2381
Danford CJ et al (2020) The Pharmacologic management of osteoporosis in primary biliary cholangitis: a systematic review and meta-analysis. J Clin Densitom 23(2):223–236
Boonstra K, Beuers U, Ponsioen CY (2012) Epidemiology of primary sclerosing cholangitis and primary biliary cirrhosis: a systematic review. J Hepatol 56(5):1181–1188
Estrada K et al (2012) Genome-wide meta-analysis identifies 56 bone mineral density loci and reveals 14 loci associated with risk of fracture. Nat Genet 44(5):491–501
Roshandel D et al (2010) Genetic variation in the RANKL/RANK/OPG signaling pathway is associated with bone turnover and bone mineral density in men. J Bone Miner Res 25(8):1830–1838
Juran BD et al (2012) Immunochip analyses identify a novel risk locus for primary biliary cirrhosis at 13q14, multiple independent associations at four established risk loci and epistasis between 1p31 and 7q32 risk variants. Hum Mol Genet 21(23):5209–5221
Tang R et al (2016) A common variant in CLDN14 is associated with primary biliary cirrhosis and bone mineral density. Sci Rep 6:19877
Wu S et al (2023) The causal relationship between autoimmune diseases and osteoporosis: a study based on Mendelian randomization. Front Endocrinol (Lausanne) 14:1196269
Davey Smith G, Hemani G (2014) Hemani, Mendelian randomization: genetic anchors for causal inference in epidemiological studies. Hum Mol Genet 23(R1):89–98
Skrivankova VW et al (2021) Strengthening the reporting of observational studies in epidemiology using mendelian randomisation (STROBE-MR): explanation and elaboration. BMJ 375:n2233
Emdin CA, Khera AV, Kathiresan S (2017) Mendelian randomization. JAMA 318(19):1925–1926
Cordell HJ et al (2021) An international genome-wide meta-analysis of primary biliary cholangitis: novel risk loci and candidate drugs. J Hepatol 75(3):572–581
Zhou W et al (2018) Efficiently controlling for case-control imbalance and sample relatedness in large-scale genetic association studies. Nat Genet 50(9):1335–1341
Sakaue S et al (2021) A cross-population atlas of genetic associations for 220 human phenotypes. Nat Genet 53(10):1415–1424
Lam M et al (2020) RICOPILI: Rapid Imputation for COnsortias PIpeLIne. Bioinformatics 36(3):930–933
Watanabe K et al (2017) Functional mapping and annotation of genetic associations with FUMA. Nat Commun 8(1):1826
Pulit SL et al (2019) Meta-analysis of genome-wide association studies for body fat distribution in 694 649 individuals of European ancestry. Hum Mol Genet 28(1):166–174
Revez JA et al (2020) Genome-wide association study identifies 143 loci associated with 25 hydroxyvitamin D concentration. Nat Commun 11(1):1647
Mbatchou J et al (2021) Computationally efficient whole-genome regression for quantitative and binary traits. Nat Genet 53(7):1097–1103
Graham SE et al (2021) The power of genetic diversity in genome-wide association studies of lipids. Nature 600(7890):675–679
Schmitz D et al (2021) Genome-wide association study of estradiol levels and the causal effect of estradiol on bone mineral density. J Clin Endocrinol Metab 106(11):e4471–e4486
Ruth KS et al (2020) Using human genetics to understand the disease impacts of testosterone in men and women. Nat Med 26(2):252–258
Burgess S, Davies NM, Thompson SG (2016) Bias due to participant overlap in two-sample Mendelian randomization. Genet Epidemiol 40(7):597–608
Bulik-Sullivan BK et al (2015) LD Score regression distinguishes confounding from polygenicity in genome-wide association studies. Nat Genet 47(3):291–295
Mounier N, Kutalik Z (2023) Bias correction for inverse variance weighting Mendelian randomization. Genet Epidemiol 47(4):314–331
Davies NM, Holmes MV, Davey Smith G (2018) Reading Mendelian randomisation studies: a guide, glossary, and checklist for clinicians. Bmj 362:k601
Hemani G, Tilling K, Davey Smith G (2017) Orienting the causal relationship between imprecisely measured traits using GWAS summary data. PLoS Genet 13(11):e1007081
Staley JR et al (2016) PhenoScanner: a database of human genotype-phenotype associations. Bioinformatics 32(20):3207–3209
Kamat MA et al (2019) PhenoScanner V2: an expanded tool for searching human genotype-phenotype associations. Bioinformatics 35(22):4851–4853
Bowden J et al (2017) A framework for the investigation of pleiotropy in two-sample summary data Mendelian randomization. Stat Med 36(11):1783–1802
Palmer TM et al (2011) Instrumental variable estimation of causal risk ratios and causal odds ratios in Mendelian randomization analyses. Am J Epidemiol 173(12):1392–1403
Sanderson E (2021) Multivariable Mendelian Randomization and mediation. Cold Spring Harb Perspect Med 11(2)
Bowden J et al (2016) Consistent estimation in Mendelian randomization with some invalid instruments using a weighted median estimator. Genet Epidemiol 40(4):304–314
Bowden J, Davey Smith G, Burgess S (2015) Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol 44(2):512–25
Burgess S, Thompson SG (2017) Interpreting findings from Mendelian randomization using the MR-Egger method. Eur J Epidemiol 32(5):377–389
Verbanck M et al (2018) Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat Genet 50(5):693–698
Morrison J et al (2020) Mendelian randomization accounting for correlated and uncorrelated pleiotropic effects using genome-wide summary statistics. Nat Genet 52(7):740–747
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11):1539–1558
Burgess S et al (2019) Guidelines for performing Mendelian randomization investigations: update for summer 2023. Wellcome Open Res 4:186
Bowden J et al (2018) Improving the visualization, interpretation and analysis of two-sample summary data Mendelian randomization via the Radial plot and radial regression. Int J Epidemiol 47(4):1264–1278
Raszeja-Wyszomirska J, Miazgowski T (2014) Osteoporosis in primary biliary cirrhosis of the liver. Prz Gastroenterol 9(2):82–87
Imamudeen N et al (2022) Management of osteoporosis and spinal fractures: contemporary guidelines and evolving paradigms. Clin Med Res 20(2):95–106
Trivedi HD et al (2020) Osteoporosis in primary biliary cholangitis: prevalence, impact and management challenges. Clin Exp Gastroenterol 13:17–24
Ruiz-Gaspà S et al (2011) Effects of bilirubin and sera from jaundiced patients on osteoblasts: contribution to the development of osteoporosis in liver diseases. Hepatology 54(6):2104–2113
Kitaura H et al (2020) Osteocyte-Related cytokines regulate osteoclast formation and bone resorption. Int J Mol Sci 21(14)
Chen X et al (2023) Vitamin D status and its associations with bone mineral density, bone turnover markers, and parathyroid hormone in Chinese postmenopausal women with osteopenia and osteoporosis. Front Nutr 10:1307896
Adejuyigbe B et al (2023) Osteoporosis: molecular pathology, diagnostics, and therapeutics. Int J Mol Sci 24(19)
Stokes CS et al (2013) Vitamin D in chronic liver disease. Liver Int 33(3):338–352
Acknowledgements
The authors thank all of the investigators participants for sharing genetic association estimates for PBC and osteoporosis. We acknowledge the use of Biorender to create graphic abstract and Fig. 1.
Funding
This study was funded by the National Natural Science Foundation of China grants (#82270554 and 81922010 to RT; #81830016 and 82130017 to XM) and Shanghai Municipal Education Commission and Shanghai Education Development Foundation (No. 20XD1422500 to RT). The funding source was not involved in study design, analysis, and interpretation of the data.
Author information
Authors and Affiliations
Contributions
Dr. Tang and Dr. Ma had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: Ruqi Tang, Xiong Ma, Zhiqiang Li, and M. Eric Gershwin. Acquisition, analysis, or interpretation of data: Yi Wu, Qiwei Qian, Minoru Nakamura, Qiaoyan Liu, Rui Wang, Xiting Pu, Yao Li, and Huayang Zhang. Drafting of the manuscript: Yi Wu and Qiwei Qian. Critical review of the manuscript for important intellectual content: Ruqi Tang, Xiong Ma, Zhiqiang Li, and M. Eric Gershwin. Statistical analysis: Yi Wu, Qiwei Qian, and Zhiqiang Li. Obtained funding: Xiong Ma and Ruqi Tang. Administrative, technical, or material support: Zhengrui You, Qi Miao, Xiao Xiao, Min Lian, and Qixia Wang. Supervision: Ruqi Tang and Xiong Ma.
Corresponding authors
Ethics declarations
Ethical Approval
Ethical approval and participant consent to participate, originally obtained in these patient cohorts, were not required here.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wu, Y., Qian, Q., Liu, Q. et al. Osteoporosis and Primary Biliary Cholangitis: A Trans-ethnic Mendelian Randomization Analysis. Clinic Rev Allerg Immunol (2024). https://doi.org/10.1007/s12016-024-08986-4
Accepted:
Published:
DOI: https://doi.org/10.1007/s12016-024-08986-4