Abstract
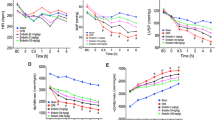
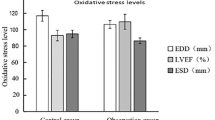
NOS–NO system activity is closely correlated with ischemia–reperfusion injury (IRI) and NOS subtypes were suggested to play different roles in IRI. In this work, the activity of serum NOS, NO levels, and ischemic necrosis after reperfusion in rabbit with AMI at different time was studied. We also explored the NOS–NO system activity changes and its correlation with myocardial ischemia and necrosis. It shows that after reperfusion in rabbits with AMI, NO–NOS system activities present different changes at each time point due to inactivation of NO and iNOS activation, and different experimental animals, ischemia–reperfusion degree, and length of time will also lead to different research results. Therefore, it is necessary to conduct dynamic observation on animals from different species at multi-temporal point under the state of NOS–NO system activities, and simultaneously detect inflammatory factor, MDA, and SOD indexes. Therefore, it is a must to conduct relevant drug research studies to make NOS–NO system activities maintain the level in favor of ideal myocardial ischemia reperfusion.



Similar content being viewed by others
References
Er, F., Dahlem, K. M., Nia, A. M., Erdmann, E., & Waltenberger, J., et al. (2016). Randomized control of sympathetic drive with continuous intravenous esmolol in patients with acute ST-segment elevation myocardial infarction: The BEtA-Blocker Therapy in Acute Myocardial Infarction (BEAT-AMI) Trial. JACC: Cardiovascular Interventions, 9(3), 231–240.
Binder, A., Ali, A., Chawla, R., Aziz, H. A., & Abbate, A., et al. (2015). Myocardial protection from ischemia-reperfusion injury post coronary revascularization. Expert Review of Cardiovascular Therapy, 13(9), 1045–1057.
Ota, S., Tanimoto, T., Hirata, K., Orii, M., & Shiono, Y., et al. (2014). Assessment of circumferential endocardial extent of myocardial edema and infarction in patients with reperfused acute myocardial infarction: A cardiovascular magnetic resonance study. International Heart Journal, 55(3), 234–238.
Anderson, J. L., & Morrow, D. A. (2017). Acute myocardial infarction. The New England Journal of Medicine, 376(21), 2053–2064.
Zhang, J., Qi, X. Y., Wan, Y. F., & Yuan, C. (2011). Establishment of a reperfusion model in rabbits with acute myocardial infarction. Cell Biochemistry and Biophysics, 60(3), 249–258.
He, P., Talukder, M. A. H., & Gao, F. (2020). Oxidative stress and microvessel barrier dysfunction. Frontiers in Physiology, 11, 472.
Hernandez-Resendiz, S., Munoz-Vega, M., Contreras, W. E., Crespo-Avilan, G. E., & Rodriguez-Montesinos, J., et al. (2018). Responses of endothelial cells towards ischemic conditioning following acute myocardial infarction. Conditioning Medicine, 1(5), 247–258.
Lee, J., Bae, E. H., Ma, S. K., & Kim, S. W. (2016). Altered nitric oxide system in cardiovascular and renal diseases. Chonnam Medical Journal, 52(2), 81–90.
Jones, S. P., Greer, J. J., Kakkar, A. K., Ware, P. D., & Turnage, R. H., et al. (2004). Endothelial nitric oxide synthase overexpression attenuates myocardial reperfusion injury. The American Journal of Physiology-Heart and Circulatory Physiology, 286(1), H276–H282.
Mallet, R. T., Manukhina, E. B., Ruelas, S. S., Caffrey, J. L., & Downey, H. F. (2018). Cardioprotection by intermittent hypoxia conditioning: Evidence, mechanisms, and therapeutic potential. The American Journal of Physiology-Heart and Circulatory Physiology, 315(2), H216–H232.
Song, W., Lu, X., & Feng, Q. (2000). Tumor necrosis factor-alpha induces apoptosis via inducible nitric oxide synthase in neonatal mouse cardiomyocytes. Cardiovascular Research, 45(3), 595–602.
Liu, Y., Xia, C., Wang, R., Zhang, J., & Yin, T., et al. (2017). The opposite effects of nitric oxide donor, S-nitrosoglutathione, on myocardial ischaemia/reperfusion injury in diabetic and non-diabetic mice. Clinical and Experimental Pharmacology and Physiology, 44(8), 854–861.
Khojah, H. M., Ahmed, S., Abdel-Rahman, M. S., & Hamza, A. B. (2016). Reactive oxygen and nitrogen species in patients with rheumatoid arthritis as potential biomarkers for disease activity and the role of antioxidants. Free Radical Biology and Medicine, 97, 285–291.
Engel, H., Friedrich, S., Schleich, C., Gebhardt, M. M., & Gross, W., et al. (2017). Enhancing nitric oxide bioavailability via exogen nitric oxide synthase and L-arginine attenuates ischemia-reperfusion-induced microcirculatory alterations. Annals of Plastic Surgery, 79(4), e25–e29.
Wang, Y., Song, X., Yue, X., Su, H., & Gu, Y., et al. (2017). Protection by nitrite against the ischemic effects induced by acute myocardial infarction in mice. The Anatolian Journal of Cardiology, 18(5), 315–320.
Muscari, C., Bonafe, F., Gamberini, C., Giordano, E., & Tantini, B., et al. (2004). Early preconditioning prevents the loss of endothelial nitric oxide synthase and enhances its activity in the ischemic/reperfused rat heart. Life Sciences, 74(9), 1127–37.
Zhang, Y., Bissing, J. W., Xu, L., Ryan, A. J., & Martin, S. M., et al. (2001). Nitric oxide synthase inhibitors decrease coronary sinus-free radical concentration and ameliorate myocardial stunning in an ischemia-reperfusion model. Journal of the American College of Cardiology, 38(2), 546–54.
Yu, X., Ge, L., Niu, L., Lian, X., & Ma, H., et al. (2018). The dual role of inducible nitric oxide synthase in myocardial ischemia/reperfusion injury: Friend or foe? Oxidative Medicine and Cellular Longevity, 2018, 8364848.
Gross, G. J., Hsu, A., Pfeiffer, A. W., & Nithipatikom, K. (2013). Roles of endothelial nitric oxide synthase (eNOS) and mitochondrial permeability transition pore (MPTP) in epoxyeicosatrienoic acid (EET)-induced cardioprotection against infarction in intact rat hearts. Journal of Molecular and Cellular Cardiology, 59, 20–29.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interes.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, J., Chen, C., Li, F. et al. Different Changing Patterns of Three NOS–NO System Activities after Ischemia–Reperfusion in Rabbit with AMI. Cell Biochem Biophys 79, 857–862 (2021). https://doi.org/10.1007/s12013-021-01011-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12013-021-01011-x