Abstract
Methicillin-resistant Staphylococcus aureus (MRSA) is considered one of the most serious multidrug-resistant bacteria worldwide. MRSA resistance to methicillin antibiotics made vancomycin, the acceptable treatment option. Silver nanoparticles (Ag-NPs) are among the well-known antibacterial substances showing multimode antibacterial action. Therefore, Ag-NPs are appropriate applicants for use in combination with vancomycin in order to augment its antibacterial action. This study aimed to biosynthesize silver nanoparticles and to evaluate its antibacterial activity against MRSA alone and when combined with vancomycin both in vitro and in vivo. Agaricus bisporus is used to reduce the silver nitrate salts in solution to yield silver nanoparticles which was characterized by UV-visible spectrophotometric analysis that shows maximum absorption at 420 nm as a preliminary confirmation for nanoparticles synthesis, Energy-Dispersive Analysis of X-ray (EDX) which confirms the crystalline nature of silver nanoparticles and transmission electron microscopy (TEM) image shows the particles in spherical form with mean size 27.45 nm. The synthesized silver nanoparticles were tested for antibacterial activity against MRSA, and the synergetic effects of the combination of silver nanoparticles and vancomycin were evaluated. The results showed a strong synergistic antibacterial effect between Ag-NPs and vancomycin in vitro with fractional inhibitory concentration 0.37 and in vivo against MRSA strain. The result revealed that mycosynthesized silver nanoparticles (NPs) enhance the in vitro and in vivo antibacterial activity of vancomycin against MRSA. These results suggested that sliver nanoparticles have an effective antibacterial activity against MRSA count, histopathology, and liver enzymes as well as protective immune response specially when combined with vancomycin in the lungs of infected rats with MRSA.






Similar content being viewed by others
Data Availability
The original datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Qiu J, Wang D, Xiang H, Feng H, Jiang Y, Xia L et al (2010) Subinhibitory concentrations of thymol reduce enterotoxins A and B and a-hemolysin production in Staphylococcus aureus isolates. PLoS One 5(3):e9736. https://doi.org/10.1371/journal.pone.0009736
Manukumar HM, Umesha S (2017) MALDI-TOF-MS based identification and molecular characterization of food associated methicillin-resistant Staphylococcus aureus. Sci Rep 7:11414. https://doi.org/10.1038/s41598-017-11597-z
Price JR, Cole K, Bexley A, Kostiou V, Eyre DW, Golubchik T, Wilson DJ, Crook DW, Walker AS, Peto TEA, Llewelyn MJ, Paul J, Modernising Medical Microbiology informatics group (2017) Transmission of Staphylococcus aureus between health-care workers, the environment, and patients in an intensive care unit: a longitudinal cohort study based on whole-genome sequencing. Lancet Infect Dis 17:207–214. https://doi.org/10.1016/S1473-3099(16)30413-3
Fraunholz M, Sinha B (2012) Intracellular Staphylococcus aureus: live-in and let die. Front Cell Infect Microbiol 2:43. https://doi.org/10.3389/fcimb.2012.00043
Poovelikunnel T, Gethin G, Humphreys H (2015) Mupirocin resistance: clinical implications and potential alternatives for the eradication of MRSA. J Antimicrob Chemother 70(10):2681–2692. https://doi.org/10.1093/jac/dkv169
Zhang S, Sun X, Chang W, Dai Y, Ma X (2015 Aug 19) Systematic review and meta-analysis of the epidemiology of vancomycin-intermediate and heterogeneous vancomycin-intermediate Staphylococcus aureus isolates. PLoS One 10(8):e0136082. https://doi.org/10.1371/journal.pone.0136082
Martin MA (1994) Methicillin-resistant Staphylococcus aureus: the persistent nosocomial pathogen. Curr Clin Top Infect Dis 14:170–191 https://academic.oup.com/jac/article/41/3/325/680999
Gardete S, Tomasz A (2014) Mechanisms of vancomycin resistance in Staphylococcus aureus. J Clin Invest 124:2836–2840. https://doi.org/10.5772/67338
Gebreyohannes G, Nyerere A, Bii C, Sbhatu DB (2019) Challenges of intervention, treatment, and antibiotic resistance of biofilm-forming microorganisms. Heliyon 5:02192. https://doi.org/10.1016/j.heliyon.2019.02192
Baptista PV, McCusker MP, Carvalho A, Ferreira DA, Mohan NM, Martins M, Fernandes AR (2018) Nano-strategies to fight multidrug resistant bacteria- “a battle of the titans”. Front Microbiol 9:1441. https://doi.org/10.3389/fmicb.2018.01441
Prabhu S, Poulose EK (2012) Silver nanoparticles: mechanism of antimicrobial action, synthesis, medical applications, and toxicity effects. Int Nano Lett 2:32. https://doi.org/10.1186/2228-5326-2-32
Rai M, Kon K, Ingle A, Duran N, Galdiero S, Galdiero M (2014) Broad-spectrum bioactivities of silver nanoparticles: the emerging trends and future prospects. Appl Microbiol Biotechnol 98:1951–1961. https://doi.org/10.1007/s00253-013-5473-x
Gupta RK, Kumar V, Gundampati RK, Malviya M, Hasan SH, Jagannadham MV et al (2017) Biosynthesis of silver nanoparticles from the novel strain of Streptomyces Sp. BHUMBU-80 with highly efficient electroanalytical detection of hydrogen peroxide and antibacterial activity. J. Environ. Chem. Eng 5:5624–5635. https://doi.org/10.1016/j.jece.2017.09.029
Loo YY, Rukayadil Y, Nor-Khaizura MAR, Kuan CH, Chieng BW, Nishibuchi M et al (2018) In vitro antimicrobial activity of green synthesized silver nanoparticles against selected gram-negative foodborne pathogens. Front Microbiol 9:1555. https://doi.org/10.3389/fmicb.2018.01555
Huang JQ, Li D, Sun Y, Lu Y, Su X, Yang H, Wang Y, Wang W, Shao N, He J, Hong, Chen C (2007) Biosynthesis of silver and gold NPs by novel sundried Cinnamomum camphora leaf. Nanotechnology 18:105104. https://doi.org/10.1088/0957-4484/18/10/105104
Austin LA, Mackey MA, Dreaden EC, ElSayed MA (2014 Jul) The optical, photothermal, and facile surface chemical properties of gold and silver nanoparticles in biodiagnostics, therapy, and drug delivery. Arch Toxicol 88(7):1391–1417. https://doi.org/10.1007/s00204-014-1245-3
Ahmed S, Ahmad M, Swami BL, Ikram S (2016) A review on plants extract mediated synthesis of silver nanoparticles for antimicrobial applications: a green expertise. J Adv Res 5:17–28. https://doi.org/10.1016/j.jare.2015.02.007
Zhang XF, Liu ZG, Shen W, Gurunathan S (2016) Silver nanoparticles: synthesis, characterization, properties, applications, and therapeutic approaches. Int J Mol Sci 17:E1534. https://doi.org/10.3390/ijms17091534
Khan AU, Malik N, Khan M, Cho MH, Khan MN (2018) Fungi-assisted silver nanoparticle synthesis and their applications. Bioprocess Biosyst Eng 41(1):1–20
Salem SS, Fouda A (2021) Green synthesis of metallic nanoparticles and their prospective biotechnological applications: an overview. Biol Trace Elem Res 199:344–370. https://doi.org/10.1007/s12011-020-02138-3
Azmath P, Baker S, Rakshith D, Satish S (2016) Mycosynthesis of silver nanoparticles bearing antibacterial activity. Saudi Pharm J 24:140–146. https://doi.org/10.1016/j.jsps.2015.01.008
Balaji DS, Basavaraja S, Deshpande R, Mahesh DB, Prabhakar BK, Venkataraman A (2009) Extracellular biosynthesis of functionalized silver nanoparticles by strains of Cladosporium cladosporioides fungus. Colloids Surf B Biointerfaces 68:88–92. https://doi.org/10.1016/j.colsurfb.2008.09.022
Du L, Xu Q, Huang M, Xian L, Feng JX (2015) Synthesis of small silver nanoparticles under light radiation by fungus Penicillium oxalicum and its application for the catalytic reduction of methylene blue. Mater Chem Phys 160:40–47. https://doi.org/10.1016/j.matchemphys.2015.04.003
Netala VR, Bethu MS, Pushpalatah B, Baki VB, Aishwarya S, Rao JV et al (2016) Biogenesis of silver nanoparticles using endophytic fungus Pestalotiopsis microspora and evaluation of their antioxidant and anticancer activities. Int J Nanomedicine 11:5683–5696. https://doi.org/10.2147/IJN.S112857
Blackwell M (2011) The Fungi: 1, 2, 3 ... 5.1 million species? Am J Bot 98(3):426–438. https://doi.org/10.3732/ajb.1000298
PM. Kirk, PF. Cannon, JC. David, JA. Stalpers, Ainsworth and Brisby’s Dictionary of the Fungi. 10th ed. Wallingford: CAB International (2008). http://www.slideshare.net/fitolima/dictionary-of-fungi-kirk-et-al-2008-10a-edicao
Wasser SP (2011) Medicinal mushroom science: history, current status, future trends, and unsolved problems in studies of medicinal mushrooms. Appl Microbiol Biotechnol 89:1323–1332. https://doi.org/10.1007/s00253-010-3067-4
Younis Ahmed M, Abdel-Aziz Marwa M, Mohammed Y (2019) Evaluation of some biological applications of Pleurotus citrinopileatus and Boletus edulis fruiting bodies extracts. Current Pharmaceutical Biotechnology Journal 20(15):1309–1320. https://doi.org/10.2174/1389201020666190904162403
Gregori A, Svagelj M, Pohleven F (2007) Cultivation techniques and medicinal properties of Pleu-rotus spp. Food Technol Biotechnol 45(3):236–247
Younis AM, Wu FS, El Shikh HH (2015) Antimicrobial activity of extracts of the oyster culinary medicinal mushroom Pleurotus ostreatus (higher Basidiomycetes) and identification of a new antimicrobial compound. Int J Med Mushrooms 17(6):579–590. https://doi.org/10.1615/intjmedmushrooms.v17.i6.80
Gurunathan S, Raman J, Abd Malek SN, John PA, Vikineswary S (2013) Green synthesis of silver nanoparticles using Ganoderma neo-japonicum Imazeki: a potential cytotoxic agent against breast cancer cells. Int J Nanomedicine 8:4399–4413. https://doi.org/10.2147/IJN.S51881
Abdel-Aziz MM, Yosri M, Amin BH (2017) Control of imipenem resistant -Klebsiella pneumoniae pulmonary infection by oral treatment using a combination of mycosynthesized Ag-nanoparticles and imipenem. Journal of Radiation Research and Applied Sciences 10(4):353–360. https://doi.org/10.1016/j.jrras.2017.09.002
National Committee for Clinical Laboratory Standards NCCLS (2000): Methods for Dilution antimicrobial susceptibility tests for bacteria that grow aerobically: approved standards- fifth edition. NCCLS document M7-A5. NCCLS: Wayne, PA, USA
Lorian 5th edition, Chapter 9 (2005) Antimicrobial combinations, in Antibiotics in laboratory medicine, pp. 365–441. Lippincott Williams and Wilkins, Philadelphia, PA 19106 USA http://www.lww.com/0-7817-4983-2
Michal Olszewski A, Nicole Falkowski R, Surana R, Sonstein J, Anne H, Bethany B, Moore BGH, Toews BG (2007 Nov 1) Effect of laparotomy on clearance and cytokine induction in Staphylococcus aureus–infected lungs. Am J Respir Crit Care Med 176(9):921–929. https://doi.org/10.1164/rccm.200606-763OC
Shatzkes K, Singleton E, Tang C, Zuena M, Shukla S, Gupta S, Dharani S, Onyile O, Rinaggio J, Connell ND, Kadouri DE (2016) Predatory bacteria attenuate Klebsiella pneumoniae burden in rat lungs. M. Bio 7(6):e01847–e01816. https://doi.org/10.1128/mBio.01847-16
Bancroft JD, Gamble M (2008) Theory and practice of histological techniques, 6th edn. Churchill Livingstone, Philadelphia
Rahisuddin SA, AL-Thabaiti Z, Khan N (2015) Manzoor, biosynthesis of silver nanoparticles and its antibacterial and antifungal activities towards gram-positive, gram-negative bacterial strains and different species of Candida fungus. Bioprocess Biosyst Eng 38(9):1773–1781. https://doi.org/10.1007/s00449-015-1418-3
Kumar SA, Abyaneh MK, Gosavi SW et al (2007). 439–45) Nitrate reductase-mediated synthesis of silver nanoparticles from AgNO3. Biotechnol Lett 29(3):439–445. https://doi.org/10.1007/s10529-006-9256-7
Vigneshwaran N, Kathe AA, Varadarajan PV, Nachane RP, Balasubramanya RH (2006) Biomimetics of silver nanoparticles by white rot fungus, Phaenerochaete chrysosporium. Colloids Surf B Biointerfaces 53(1):55–59. https://doi.org/10.1016/j.colsurfb.2006.07.014
Narasimha G, Janardhan, Alzohairy M, Khadr H, Mallikarjuna K (2013) Extracellular synthesis, characterization and antibacterial activity of silver nanoparticles by Actinomycetes isolative. Int. J. Nanodimens 4:77–83. https://doi.org/10.7508/IJND.2013.01.010
Slavin YN, Asnis J, Häfeli UO, Bach H (2017) Metal nanoparticles: understanding the mechanisms behind antibacterial activity. J Nanobiotechnol 15:65. https://doi.org/10.1186/s12951-017-0308-z
Sudhakar T, Nanda A, Babu SG, Janani S, Evans MD, Markose TK (2014) Synthesis of silver nanoparticles from edible mushroom and its antimicrobial activity against human pathogens. International Journal of PharmTech Research 6(5):1718–1723
Aruguete DM, Hochella MF Bacteria-nanoparticle interactions and their environmental implications. Environ. Chem. 7:3–9. https://doi.org/10.1071/EN09115
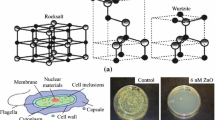
Zhang L, Jiang Y, Ding Y, Povey M, York D (2007) Investigation into the antibacterial behavior of suspensions of ZnO nanoparticles (ZnO nanofluids). J Nanopart Res 9:479–489. https://doi.org/10.1007/s11051-006-9150-1
Pareek V, Gupta R, Panwar J (2018) Do physico-chemical properties of silver nanoparticles decide their interaction with biological media and bactericidal action? A review. Mater Sci Eng C Mater Biol Appl 90:739–749. https://doi.org/10.1016/j.msec.2018.04.093
Wagner H, Ulrich-Merzenich G Synergy research: approaching a new generation of phytopharmaceuticals. Phytomedicine 16(2–3):97–110. https://doi.org/10.1016/j.phymed.2008.12.018
Dhanasekaran D, Latha S, Saha S, Thajuddin N, Panneerselvam A (2013) Extracellular biosynthesis, characterisation and in-vitro antibacterial potential of silver nanoparticles using Agaricus bisporus. J Experim Nanosci 8(4):579–588. https://doi.org/10.1080/17458080.2011.577099
Hwang IS, Hwang JH, Choi H, Kim K-J, Lee DG (2012) Synergistic effects between silver nanoparticles and antibiotics and the mechanisms involved. Journal of medical microbiology 61:1719–1726. https://doi.org/10.1099/jmm.0.047100-0
Hassanen EI, Ragab E (2021) In vivo and in vitro assessments of the antibacterial potential of chitosan-silver Nanocomposite against methicillin-resistant Staphylococcus aureus–induced infection in rats. Biol Trace Elem Res 199:244–257. https://doi.org/10.1007/s12011-020-02143-6
Panacek A, Kolar M, Vecerova R, Prucek R, Soukupova J, Krystof V et al (2009) Antifungal activity of silver nanoparticles against Candida spp. Biomaterials 30:6333e6340–6333e6340. https://doi.org/10.1016/j.biomaterials.2009.07.065
Panacek A, Prucek R, Safarova D, Dittrich M, Richtrova J, Benickova K, Zboril R, Kvitek L (2011) Acute and chronic toxicity effects of silver nanoparticles (Nps) on drosophila melanogaster. Environ Sci Technol 45:4974e4979–4974e4979. https://doi.org/10.1021/es104216b
Kvitek L, Vanickova M, Panacek A, Soukupova J, Dittrich M, Valentova E, Prucek R, Bancirova M, Milde D, Zboril R (2009) Initial study on the toxicity of silver nanoparticles (Nps) against Paramecium caudatum. J Phys Chem C 113:4296e4300–4296e4300. https://doi.org/10.1021/jp808645e
Krajewski S, Prucek R, Panacek A, Avci-Adali M, Nolte A, Straub A, Zboril R, Wendel HP, Kvitek L (2013) Hemocompatibility evaluation of different silver nanoparticle concentrations employing a modified chandler-loop in vitro assay on human blood. Acta Biomater 9:7460e7468–7460e7468. https://doi.org/10.1016/j.actbio.2013.03.016
Reidy B, Haase A, Luch A, Dawson KA, Lynch I (2013) Mechanisms of silver nanoparticle release, transformation and toxicity: a critical review of current knowledge and recommendations for future studies and applications. Mater. 6(6):2295–2350. https://doi.org/10.3390/ma6062295
Rai M, Deshmukh S, Ingle A, Gade A (2012) Silver nanoparticles: the powerful nanoweapon against multidrug-resistant bacteria. J Appl Microbiol 112(5):841–852. https://doi.org/10.1111/j.1365-2672.2012.05253.x
Wypij M, Czarnecka J, Świecimska M, Dahm H, Rai M, Golinska P (2018) Synthesis, characterization and evaluation of antimicrobial and cytotoxic activities of biogenic silver nanoparticles synthesized from Streptomyces xinghaiensis OF1 strain. World J Microbiol Biotechnol 34(2):23–29. https://doi.org/10.1007/s11274-017-2406-3
Dahm H (2020) Silver nanoparticles in wound infections: present status and future prospects. In: Rai M (ed) Nanotechnology in skin, soft tissue, and bone infections. Springer International Publishing, Cham, pp 151–168
Alavi M, Rai M (2019) Recent advances in antibacterial applications of metal nanoparticles (MNPs) and metal nanocomposites (MNCs) against multidrug-resistant (MDR) bacteria. Expert Rev Anti-Infect Ther 17(6):419–428. https://doi.org/10.1080/14787210.2019.1614914
Pumerantz A, Muppidi K, Agnihotri S, Guerra C, Venketaraman V, Wang J, Betageri G (2011) Preparation of liposomal vancomycin and intracellular killing of meticillin-resistant Staphylococcus aureus (MRSA). Int J Antimicrob Agents 37:140–144 10 .1016/j.ijantimicag.2010.10.011
Kolaczkowska E, Jenne CN, Surewaard BG, Thanabalasuriar A, Lee WY, Sanz MJ, Mowen K, Opdenakker G, Kubes P (2015) Molecular mechanisms of NET formation and degradation revealed by intravital imaging in the liver vasculature. Nat Commun 6:6673. https://doi.org/10.1038/ncomms7673
Ramaiah SK (2007) A toxicologist guide to the diagnostic interpretation of hepatic biochemical parameters. Food Chem Toxicol 45:1551–1557. https://doi.org/10.1016/j.fct.2007.06.007
Hassanen EI, Khalaf AA, Tohamy AF, Mohammed ER, Farroh KY (2019) Toxicopathological and immunological studies on different concentrations of chitosan-coated silver nanoparticles in rats. Int J Nanomedicine:4723–4739. https://doi.org/10.2147/IJN.S207644
Vasquez RD, Apostol JG, de Leon JD et al (2016) Polysaccharide-mediated green synthesis of silver nanoparticles from Sargassum siliquosum JG Agardh: assessment of toxicity and hepatoprotective activity. OpenNano 1:16–24. https://doi.org/10.1016/j.onano.2016.03.001
Roy N, Gaur A, Jain A, Bhattacharya S, Rani V (2013) Green synthesis of silver nanoparticles: an aproach to overcome toxicity. Environ Toxicol Pharmacol 36(3):807–812. https://doi.org/10.1016/j.etap.2013.07.005
Chatterjee S, Dey A, Dutta R, Dey S, Acharya K (2011) Hepatoprotective effect of the ethanolic extract of Calocybe indica on mice with CCl4 hepatic intoxication. Int J PharmTech Res 3(4):2162–2168 https://www.researchgate.net/publication/259479079
Bartlett AH, Foster TJ, Hayashida A, Park PW (2008) Alphatoxin facilitates the generation of CXC chemokine gradients and stimulates neutrophil homing in Staphylococcus aureus pneumonia. J Infect Dis 198:1529–1535. https://doi.org/10.1086/592758
Small CL, McCormick S, Gill N, Kugathasan K, Santosuosso M, Donaldson N, Heinrichs DE, Ashkar A, Xing Z (2008) NK cells play a critical protective role in host defense against acute extracellular Staphylococcus aureus bacterial infection in the lung. J. Immunol:1805558–1805568. https://doi.org/10.4049/jimmunol.180.8.5558
Ventura CL, Higdon R, Hohmann L, Martin D, Kolker E, Liggitt HD, Skerrett SJ, Rubens CE (2008) Staphylococcus aureus elicits marked alterations in the airway proteome during early pneumonia. Infect. Immun:765862–765872. https://doi.org/10.1128/IAI.00865-08
Kiem S, Schentag JJ (2008) Interpretation of antibiotic concentration ratios measured in epithelial lining fluid. Antimicrob Agents Chemother 52:24–36. https://doi.org/10.1128/AAC.00133-06
Rello J, Mallol J (2006) Optimal therapy for methicillin-resistant Staphylococcus aureus pneumonia: what is the best dosing regimen? Chest 130:938–940. https://doi.org/10.1378/chest.130.4.938
Theuretzbacher U (2007) Tissue penetration of antibacterial agents: how should this be incorporated into pharmacodynamic analyses? Curr Opin Pharmacol 7:498–504. https://doi.org/10.1016/j.coph.2007.05.003
Bhattacharjee M (2016) Chemistry of antibiotics and related drugs. Springer Science and Business Media, New York
Author information
Authors and Affiliations
Contributions
M.Y and M. M guided the research, performed the experiments, performed data analysis, and wrote the manuscript. M A is a research scholar who performed the experiments. A. Y assisted in the experiments. N S is the professor of Microbiology who supervised the whole studies and revised the manuscript. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
The experimental protocol has been accepted by the Faculty of Medicines Scientific Research Ethics Committee, Al-Azhar University.
Consent for Publication
Not applicable.
Competing Interests
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Awad, M., Yosri, M., Abdel-Aziz, M.M. et al. Assessment of the Antibacterial Potential of Biosynthesized Silver Nanoparticles Combined with Vancomycin Against Methicillin-Resistant Staphylococcus aureus–Induced Infection in Rats. Biol Trace Elem Res 199, 4225–4236 (2021). https://doi.org/10.1007/s12011-020-02561-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-020-02561-6