Abstract
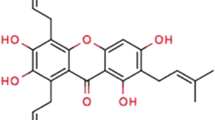
There are numerous therapeutic applications for ginsenoside Rb1 (GRb1), the primary saponin derived from ginseng root. According to earlier research, ginsenoside Rb1 causes apoptosis and reduces the cell cycle. Its adverse effects, especially those on the development of the embryo, still need to be thoroughly studied. A host’s lifestyle choices, including smoking, drinking too much alcohol, using tobacco products, and having an HPV infection, can increase the risk of oral squamous cell carcinoma (OSCC), one of the most prevalent malignancies of the oral cavity. To address this challenge, this investigation focuses on the design of GRb1 for treating OSCC. In vitro cytotoxicity studies confirmed that GRb1 was more effective in PCI-9A and PCI-13 cells, with reduced toxicity in non-cancerous cells. Further verification of cellular morphology was achieved through various biochemical staining methods. The mechanism of cell death was investigated by Annexin V-FITC and PI methods. Additionally, the antimetastatic attributes of GRb1 have been evaluated using both migration scratch and Transwell migration assays, which have collectively revealed excellent antimetastatic potential. The DNA fragmentation of the PCI-9A and PCI-13 cells was assessed using a comet assay. Ginsenoside Rb1 improved ROS levels and caused mitochondrial membrane potential alterations and DNA damage, which resulted in apoptosis. OSCC administration significantly reduced the levels of SOD, GSH, GPx, and CAT, increasing the levels of PCI-9A and PCI-13 cells, while GRb1 improved this situation. Therefore, we propose that Ginsenoside Rb1 could be an alternative therapeutic strategy for OSCC therapy.











Similar content being viewed by others
Data Availability
All data generated or analyzed during this research are included in this published article.
References
de Mendoza, I. L. I., Mendia, X. M., de la Fuente, A. M. G., Andres, G. Q., & Urizar, J. M. A. (2020). Role of Porphyromonas gingivalis in oral squamous cell carcinoma development: A systematic review. Journal of Periodontal Research, 55, 13–22.
Das, N., Hussain, E., & Mahanta, L. B. (2020). Automated classification of cells into multiple classes in epithelial tissue of oral squamous cell carcinoma using transfer learning and convolutional neural network. Neural Networks, 128, 47–60.
Liu, L., Chen, J., Cai, X., Yao, Z., & Huang, J. (2019). Progress in targeted therapeutic drugs for oral squamous cell carcinoma. Surgical Oncology, 31, 90–97.
Cristaldi, M., Mauceri, R., Di Fede, O., Giuliana, G., Campisi, G., & Panzarella, V. (2019). Salivary biomarkers for oral squamous cell carcinoma diagnosis and follow-up: Current status and perspectives. Frontiers in Physiology, 10, 1476.
Jiang, X., Wu, J., Wang, J., & Huang, R. (2019). Tobacco and oral squamous cell carcinoma: A review of carcinogenic pathways. Tobacco Induced Diseases, 17.
Capote-Moreno, A., Brabyn, P., Muñoz-Guerra, M. F., Sastre-Pérez, J., Escorial-Hernandez, V., Rodríguez-Campo, F. J., García, T., & Naval-Gías, L. (2020). Oral squamous cell carcinoma: Epidemiological study and risk factor assessment based on a 39-year series. International Journal of Oral and Maxillofacial Surgery, 49, 1525–1534.
Alabi, R. O., Youssef, O., Pirinen, M., Elmusrati, M., Mäkitie, A. A., Leivo, I., & Almangush, A. (2021). Machine learning in oral squamous cell carcinoma: Current status, clinical concerns and prospects for future—A systematic review. Artificial Intelligence in Medicine, 115, 102060.
Ling, Z., Cheng, B., & Tao, X. (2021). Epithelial-to-mesenchymal transition in oral squamous cell carcinoma: challenges and opportunities. International Journal of Cancer, 148, 1548–1561.
Bugshan, A., & Farooq, I. (2020). Oral squamous cell carcinoma: metastasis, potentially associated malignant disorders, etiology and recent advancements in diagnosis. F1000Research, 9.
Almangush, A., Mäkitie, A. A., Triantafyllou, A., de Bree, R., Strojan, P., Rinaldo, A., Hernandez-Prera, J. C., Suárez, C., Kowalski, L. P., & Ferlito, A. (2020). Staging and grading of oral squamous cell carcinoma: An update. Oral Oncology, 107, 104799.
Li, H., & Li, H. (2020). Ginsenoside-Rg5 inhibits growth and metastasis of ovarian carcinoma via suppressing expression of fibroblast growth factor-8b (FGF8b). Journal of King Saud University-Science, 32, 1162–1167.
Shan, K., Wang, Y., Hua, H., Qin, S., Yang, A., & Shao, J. (2019). Ginsenoside Rg3 combined with oxaliplatin inhibits the proliferation and promotes apoptosis of hepatocellular carcinoma cells via downregulating PCNA and cyclin D1. Biological and Pharmaceutical Bulletin, 42, 900–905.
Qu, L., Liu, Y., Deng, J., Ma, X., & Fan, D. (2023). Ginsenoside Rk3 is a novel PI3K/AKT-targeting therapeutics agent that regulates autophagy and apoptosis in hepatocellular carcinoma. Journal of Pharmaceutical Analysis, 13, 463–482.
Hong, H., Baatar, D., & Hwang, S. G. (2021). Anticancer activities of ginsenosides, the main active components of ginseng. Evidence-Based Complementary and Alternative Medicine, 2021.
Zhu, H., He, Y.-S., Ma, J., Zhou, J., Kong, M., Wu, C.-Y., Mao, Q., Lin, G., & Li, S.-L. (2021). The dual roles of ginsenosides in improving the anti-tumor efficiency of cyclophosphamide in mammary carcinoma mice. Journal of Ethnopharmacology, 265, 113271.
Zhang, J., Ma, X., & Fan, D. (2021). Ginsenoside CK inhibits hypoxia-induced epithelial–mesenchymal transformation through the HIF-1α/NF-κB feedback pathway in hepatocellular carcinoma. Foods, 10, 1195.
Zhu, H., Wang, S.-Y., Zhu, J.-H., Liu, H., Kong, M., Mao, Q., Zhang, W., & Li, S.-L. (2021). Efficacy and safety of transcatheter arterial chemoembolization combined with ginsenosides in hepatocellular carcinoma treatment. Phytomedicine, 91, 153700.
Hwang, H. J., Hong, S. H., Moon, H. S., Yoon, Y. E., & Park, S. Y. (2022). Ginsenoside Rh2 sensitizes the anti-cancer effects of sunitinib by inducing cell cycle arrest in renal cell carcinoma. Scientific Reports, 12, 19752.
Qu, L., Ma, X., & Fan, D. (2021). Ginsenoside Rk3 suppresses hepatocellular carcinoma development through targeting the gut-liver axis. Journal of Agricultural and Food Chemistry, 69, 10121–10137.
Yang, X., Li, Y., & Qian, H. (2020). Study on the selection of the targets of esophageal carcinoma and interventions of ginsenosides based on network pharmacology and bioinformatics. Evidence-Based Complementary and Alternative Medicine, 2020.
Ren, Z., Chen, X., Hong, L., Zhao, X., Cui, G., Li, A., Liu, Y., Zhou, L., Sun, R., Shen, S., Li, J., Lou, J., Zhou, H., Wang, J., Xu, G., Yu, Z., Song, Y., & Chen, X. (2020). Nanoparticle conjugation of ginsenoside Rg3 inhibits hepatocellular carcinoma development and metastasis. Small, 16, 1905233. https://doi.org/10.1002/smll.201905233
Cai, L., Qin, X., Xu, Z., Song, Y., Jiang, H., Wu, Y., Ruan, H., & Chen, J. (2019). Comparison of cytotoxicity evaluation of anticancer drugs between real-time cell analysis and CCK-8 method. ACS Omega, 4, 12036–12042. https://doi.org/10.1021/acsomega.9b01142
Li, J., Hu, S., Zhang, Z., Qian, L., Xue, Q., & Qu, X. (2020). LASP2 is downregulated in human liver cancer and contributes to hepatoblastoma cell malignant phenotypes through MAPK/ERK pathway. Biomedicine & Pharmacotherapy, 127, 110154. https://doi.org/10.1016/j.biopha.2020.110154
Velmurugan, P., Shim, J., Bang, K.-S., & Oh, B.-T. (2016). Gold nanoparticles mediated coloring of fabrics and leather for antibacterial activity. Journal of Photochemistry and Photobiology B: Biology, 160, 102–109. https://doi.org/10.1016/j.jphotobiol.2016.03.051
Pan, W., Gong, S., Wang, J., Yu, L., Chen, Y., Li, N., & Tang, B. (2019). A nuclear-targeted titanium dioxide radiosensitizer for cell cycle regulation and enhanced radiotherapy. Chemical Communications, 55, 8182–8185. https://doi.org/10.1039/C9CC01651A
Rudrappa, M., Rudayni, H. A., Assiri, R. A., Bepari, A., Basavarajappa, D. S., Nagaraja, S. K., Chakraborty, B., Swamy, P. S., Agadi, S. N., Niazi, S. K., & Nayaka, S. (2022). Plumeria alba-mediated green synthesis of silver nanoparticles exhibits antimicrobial effect and anti-oncogenic activity against glioblastoma U118 MG cancer cell line. Nanomaterials, 12. https://doi.org/10.3390/nano12030493
Li, K. G., Chen, J. T., Bai, S. S., Wen, X., Song, S. Y., Yu, Q., Li, J., & Wang, Y. Q. (2009). Intracellular oxidative stress and cadmium ions release induce cytotoxicity of unmodified cadmium sulfide quantum dots. Toxicology in Vitro, 23, 1007–1013. https://doi.org/10.1016/j.tiv.2009.06.020
Han, Y., Jiang, Y., Li, Y., Wang, M., Fan, T., Liu, M., Ke, Q., Xu, H., & Yi, Z. (2019). An aligned porous electrospun fibrous scaffold with embedded asiatic acid for accelerating diabetic wound healing. Journal of Materials Chemistry B, 7, 6125–6138. https://doi.org/10.1039/C9TB01327J
Chen, Q., Jiao, D., Yan, L., Wu, Y., Hu, H., Song, J., Yan, J., Wu, L., Xu, L., & Shi, J. (2015). Comprehensive gene and microRNA expression profiling reveals miR-206 inhibits MET in lung cancer metastasis. Molecular BioSystems, 11, 2290–2302. https://doi.org/10.1039/C4MB00734D
Author information
Authors and Affiliations
Contributions
Le An, and Yang Yu: conceptualization, writing, data curation, software, writing original draft, methodology. Long He: analyzed and interpreted the data, resources, contributed reagents. Xu Xiao: materials, analysis data, software. Pengcheng Li: conceptualization, project administration, writing—review and editing
Corresponding author
Ethics declarations
Conflict of Interest
No potential conflict of interest was reported by the authors.
Ethics Approval
NA.
Consent to Participate
NA.
Consent for Publication
All authors agreed to publish this paper in this journal.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
An, L., Yu, Y., He, L. et al. Ginsenoside Rb1 Deters Cell Proliferation, Induces Apoptosis, Alleviates Oxidative Stress, and Antimetastasis in Oral Squamous Carcinoma Cells. Appl Biochem Biotechnol (2024). https://doi.org/10.1007/s12010-024-04880-z
Accepted:
Published:
DOI: https://doi.org/10.1007/s12010-024-04880-z