Abstract
Purpose
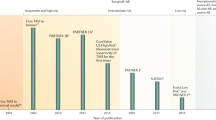
Transcatheter aortic valve implantation (TAVI) has grown in popularity as an alternative to surgical aortic valve replacement (SAVR) for the management of aortic stenosis. In this review, we perform a critical appraisal of the key studies comparing TAVI and SAVR in aortic stenosis patients with intermediate and low risk of operative mortality.
Recent findings
Early data from TAVI vs. SAVR trials in low and intermediate surgical risk patients suggest equivalent outcomes at 2 years, with some hints of superiority for TAVI over SAVR in the low-risk group. Initial mid-term data are a bit less favorable for TAVI with interval dissipation of any early survival/stroke advantages and some new questions about TAVI prosthesis durability.
Summary
The detailed discussion highlights the distinguishing features of several seminal studies, the salient features of major society treatment guidelines, the gaps in the literature, and the critical controversies that will shape the future of the field.

Similar content being viewed by others
References and Recommended Readings
Papers of particular interest, published recently, have been highlighted as:
• Of importance
Siontis GCM, et al. Transcatheter aortic valve implantation vs. surgical aortic valve replacement for treatment of symptomatic severe aortic stenosis: an updated meta-analysis. Eur Heart J. 2019;40(38):3143–53. https://doi.org/10.1093/eurheartj/ehz275.
Carroll JD, et al. STS-ACC TVT registry of transcatheter aortic valve replacement. J Am Coll Cardiol. 2020;76(21):2492–516. https://doi.org/10.1016/j.jacc.2020.09.595.
Nishimura RA, et al. AHA/ACC focused update of the 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017;135(25):e1159–95. https://doi.org/10.1161/CIR.0000000000000503.
Otto CM, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021;143(5):72–227. https://doi.org/10.1161/cir.0000000000000923.
Kaul S. Raising the evidentiary bar for guideline recommendations for TAVR: JACC review topic of the week. J Am Coll Cardiol. 2020;76(8):985–91. https://doi.org/10.1016/j.jacc.2020.05.085.
• Leon MB, et al. Transcatheter or surgical aortic-valve replacement in intermediate-risk patients. N Engl J Med. 2016;374(17):1609–20. https://doi.org/10.1056/NEJMoa1514616. Report from the initial US RCT for TAVI vs. SAVR in intermediate surgical risk patients.
Elmariah S, et al. Transapical transcatheter aortic valve replacement is associated with increased cardiac mortality in patients with left ventricular dysfunction: insights from the PARTNER I trial. JACC Cardiovasc Interv. 2017;10(23):2414–22. https://doi.org/10.1016/j.jcin.2017.09.023.
Moat NE. Will TAVR become the predominant method for treating severe aortic stenosis? N Engl J Med. 2016;374(17):1682–3. https://doi.org/10.1056/nejme1603473.
• Reardon MJ, et al. Surgical or transcatheter aortic-valve replacement in intermediate-risk patients. N Engl J Med. 2017;376(14):1321–31. https://doi.org/10.1056/NEJMoa1700456. Report from the second US RCT for TAVI vs. SAVR in intermediate surgical risk patients.
Van Belle E, et al. Balloon-expandable versus self-expanding transcatheter aortic valve replacement: a propensity-matched comparison from the FRANCE-TAVI registry. Circulation. 2020;243–259. https://doi.org/10.1161/CIRCULATIONAHA.119.043785.
Furer A, et al. Effect of baseline left ventricular ejection fraction on 2-year outcomes after transcatheter aortic valve replacement: analysis of the PARTNER 2 trials. Circ Hear Fail. 2019;12(8). https://doi.org/10.1161/CIRCHEARTFAILURE.118.005809.
Schewel J, Schlüter M, Schmidt T, Kuck KH, Frerker C, Schewel D. Early haemodynamic changes and long-term outcome of patients with severe low-gradient aortic stenosis after transcatheter aortic valve replacement. EuroIntervention. 2020;15(13):1181–9. https://doi.org/10.4244/EIJ-D-19-00399.
Søndergaard L, et al. Comparison of a complete percutaneous versus surgical approach to aortic valve replacement and revascularization in patients at intermediate surgical risk results from the randomized SURTAVI trial. Circulation. 2019;140(16):1296–305. https://doi.org/10.1161/CIRCULATIONAHA.118.039564.
Pibarot P, et al. Structural deterioration of transcatheter versus surgical aortic valve bioprostheses in the PARTNER-2 trial. J Am Coll Cardiol. 2020;76(16):1830–43. https://doi.org/10.1016/j.jacc.2020.08.049.
Makkar RR, et al. Five-year outcomes of transcatheter or surgical aortic-valve replacement. N Engl J Med. 2020;382(9):799–809. https://doi.org/10.1056/NEJMoa1910555.
Maes F, et al. Outcomes from transcatheter aortic valve replacement in patients with low-flow, low-gradient aortic stenosis and left ventricular ejection fraction less than 30%: a substudy from the TOPAS-TAVI registry. JAMA Cardiol. 2019;4(1):64–70. https://doi.org/10.1001/jamacardio.2018.4320.
Piazza N, et al. A 3-center comparison of 1-year mortality outcomes between transcatheter aortic valve implantation and surgical aortic valve replacement on the basis of propensity score matching among intermediate-risk surgical patients. JACC Cardiovasc Interv. 2013;6(5):443–51. https://doi.org/10.1016/j.jcin.2013.01.136.
Latib A, et al. Transcatheter vs surgical aortic valve replacement in intermediate- surgical-risk patients with aortic stenosis: a propensity score-matched case-control study. Am Heart J. 2012;164(6):910–7. https://doi.org/10.1016/j.ahj.2012.09.005.
Tamburino C, et al. 1-year outcomes after transfemoral transcatheter or surgical aortic valve replacement: results from the Italian OBSERVANT study. J Am Coll Cardiol. 2015;66(7):804–12. https://doi.org/10.1016/j.jacc.2015.06.013.
Foroutan F, et al. Prognosis after surgical replacement with a bioprosthetic aortic valve in patients with severe symptomatic aortic stenosis: systematic review of observational studies. BMJ. 2016;354. https://doi.org/10.1136/bmj.i5065.
Bourguignon T, et al. Very long-term outcomes of the carpentier-edwards perimount valve in aortic position. Ann Thorac Surg. 2015;99(3):831–7. https://doi.org/10.1016/j.athoracsur.2014.09.030.
Van Belle E, Delhaye C, Vincent F. Structural valve deterioration at 5 years of TAVR versus SAVR: half full or half empty?. J Am Coll Cardiol. 2020;76(16):1844–47. https://doi.org/10.1016/j.jacc.2020.09.009.
Kumar A, et al. Hemodynamic durability of transcatheter aortic valves using the updated Valve Academic Research Consortium-2 criteria. Catheter Cardiovasc Interv. 2019;93(4):729–38. https://doi.org/10.1002/ccd.27927.
• Mack MJ, et al. Transcatheter aortic-valve replacement with a balloon-expandable valve in low-risk patients. N Engl J Med. 2019;380(18):1695–705. https://doi.org/10.1056/NEJMoa1814052. Initial data on early outcomes from the RCT for TAVI vs. SAVR in low surgical risk patients.
• Popma JJ, et al. Transcatheter aortic-valve replacement with a self-expanding valve in low-risk patients. N Engl J Med. 2019;380(18):1706–15. https://doi.org/10.1056/NEJMoa1816885. Initial data on early outcomes from the RCT for TAVI vs. SAVR in low surgical risk patients.
Leon MB, et al. Outcomes 2 years after transcatheter aortic valve replacement in patients at low surgical risk. J Am Coll Cardiol. 2021;77(9):1149–61. https://doi.org/10.1016/j.jacc.2020.12.052.
Prendergast BD, Redwood SR, Patterson T. TAVR versus SAVR in aortic stenosis: long journey, new roadmap. J Am Coll Cardiol. 2021;77(9):1162–64. https://doi.org/10.1016/j.jacc.2021.01.012.
Thyregod HGH, et al. Transcatheter versus surgical aortic valve replacement in patients with severe aortic valve stenosis: 1-year results from the all-comers NOTION randomized clinical trial. J Am Coll Cardiol. 2015;65(20):2184–94. https://doi.org/10.1016/j.jacc.2015.03.014.
Thyregod HGH, et al. Five-year clinical and echocardiographic outcomes from the NOTION randomized clinical trial in patients at lower surgical risk. Circulation. 2019;139(24):2714–23. https://doi.org/10.1161/CIRCULATIONAHA.118.036606.
Çelik M, Milojevic MM, Durko AP, Oei FBS, Bogers AJJC, Mahtab EAF. Mortality in low-risk patients with aortic stenosis undergoing transcatheter or surgical aortic valve replacement: a reconstructed individual patient data meta-analysis. Interact Cardiovasc Thorac Surg. 2020;31(5):587–94. https://doi.org/10.1093/icvts/ivaa179.
Kolte D, et al. Transcatheter versus surgical aortic valve replacement in low-risk patients. J Am Coll Cardiol. 2019;74(12):1532–40. https://doi.org/10.1016/j.jacc.2019.06.076.
Thourani VH, et al. The international society for minimally invasive cardiothoracic surgery expert consensus statement on transcatheter and surgical aortic valve replacement in low- and intermediate-risk patients: a meta-analysis of randomized and propensity-matched studies. Innovations (Phila). 2021;16(1):3–16. https://doi.org/10.1177/1556984520978316.
Rosato S, et al. Transcatheter aortic valve implantation compared with surgical aortic valve replacement in low-risk patients. Circ Cardiovasc Interv. 2016;9(5). https://doi.org/10.1161/CIRCINTERVENTIONS.115.003326.
Virtanen MPO, et al. Comparison of outcomes after transcatheter aortic valve replacement vs surgical aortic valve replacement among patients with aortic stenosis at low operative risk. JAMA Netw Open. 2019;2(6): e195742. https://doi.org/10.1001/jamanetworkopen.2019.5742.
Frerker C, et al. In-hospital mortality in propensity-score matched low-risk patients undergoing routine isolated surgical or transfemoral transcatheter aortic valve replacement in 2014 in Germany. Clin Res Cardiol. 2017;106(8):610–7. https://doi.org/10.1007/s00392-017-1097-y.
Brennan JM, et al. Transcatheter versus surgical aortic valve replacement: propensity-matched comparison. J Am Coll Cardiol. 2017;70(4):439–50. https://doi.org/10.1016/j.jacc.2017.05.060.
Bekeredjian R, et al. Patients at low surgical risk as defined by the society of thoracic surgeons score undergoing isolated interventional or surgical aortic valve implantation: in-hospital data and 1-year results from the German Aortic Valve Registry (GARY). Eur Heart J. 2019;40(17):1323–30. https://doi.org/10.1093/eurheartj/ehy699.
Schaefer A, et al. Transcatheter aortic valve implantation versus surgical aortic valve replacement in low-risk patients: a propensity score-matched analysis. Eur J Cardio-Thoracic Surg. 2019;56(6):1131–9. https://doi.org/10.1093/ejcts/ezz245.
Forrest JK, et al. Transcatheter aortic valve replacement in bicuspid versus tricuspid aortic valves from the STS/ACC TVT Registry. JACC Cardiovasc Interv. 2020;13(15):1749–59. https://doi.org/10.1016/j.jcin.2020.03.022.
Makkar RR, et al. Association between transcatheter aortic valve replacement for bicuspid vs tricuspid aortic stenosis and mortality or stroke. JAMA - J Am Med Assoc. 2019;321(22):2193–202. https://doi.org/10.1001/jama.2019.7108.
Halim SA. et al. Outcomes of transcatheter aortic valve replacement in patients with bicuspid aortic valve disease: a report from the society of thoracic surgeons/American College of Cardiology Transcatheter valve Therapy registry. Circulation. 2020;1071–79. https://doi.org/10.1161/CIRCULATIONAHA.119.040333.
Waksman R, et al. Transcatheter aortic valve replacement in low-risk patients with symptomatic severe bicuspid aortic valve stenosis. JACC Cardiovasc Interv. 2020;13(9):1019–27. https://doi.org/10.1016/j.jcin.2020.02.008.
Lytvyn L, et al. Patient values and preferences on transcatheter or surgical aortic valve replacement therapy for aortic stenosis: a systematic review. BMJ Open. 2016;6(9): e014327. https://doi.org/10.1136/bmjopen-2016-014327.
Anaya J, et al. Pilot study of a patient decision aid for valve choices in surgical aortic valve replacement. Ann Thorac Surg. 2019;108(3):730–6. https://doi.org/10.1016/j.athoracsur.2019.03.048.
Landes U, et al. Repeat transcatheter aortic valve replacement for transcatheter prosthesis dysfunction. J Am Coll Cardiol. 2020;75(16):1882–93. https://doi.org/10.1016/j.jacc.2020.02.051.
Makkar RR, et al. Determinants and outcomes of acute transcatheter valve-in-valve therapy or embolization: a study of multiple valve implants in the U.S. PARTNER trial (Placement of aortic transcatheter valve trial Edwards SAPIEN transcatheter heart valve). J Am Coll Cardiol. 2013;62(5):418–30. https://doi.org/10.1016/j.jacc.2013.04.037.
Witkowski A, Jastrzebski J, Dabrowski M, Chmielak Z. Second transcatheter aortic valve implantation for treatment of suboptimal function of previously implanted prosthesis: Review of the literature. J Interv Cardiol. 2014;27(3):300–7. https://doi.org/10.1111/joic.12120.
Jawitz OK, et al. Reoperation after transcatheter aortic valve replacement: an analysis of the society of thoracic surgeons database. JACC Cardiovasc Interv. 2020;13(13):1515–25. https://doi.org/10.1016/j.jcin.2020.04.029.
Fukuhara S, et al. Surgical explantation of transcatheter aortic bioprostheses: results and clinical implications. J Thorac Cardiovasc Surg. 2020. https://doi.org/10.1016/j.jtcvs.2019.11.139.
Ochiai T, et al. Coronary access after TAVR. JACC Cardiovasc Interv. 2020;13(6):693–705. https://doi.org/10.1016/j.jcin.2020.01.216.
Tang GHL, Kaneko T, Cavalcante J. Predicting the feasibility of post-TAVR coronary access and redo TAVR: more unknowns than knowns. JACC Cardiovasc Interv. 2020;13(6):736–38. https://doi.org/10.1016/j.jcin.2020.01.222.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
Not required.
Human and animal rights and informed consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Consent for publication
All authors reviewed the manuscript and approved submission to the journal.
Conflict of interest
Asishana A. Osho declares that he has no conflict of interest. Nathaniel B. Langer declares that he has no conflict of interest. Arminder S. Jassar declares that he has no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Valvular Heart Disease
Rights and permissions
About this article
Cite this article
Osho, A.A., Langer, N.B. & Jassar, A.S. Transcatheter Aortic Valve Implantation in Low and Intermediate Surgical Risk Patients: a Critical Appraisal of Seminal Studies. Curr Treat Options Cardio Med 24, 1–11 (2022). https://doi.org/10.1007/s11936-022-00960-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11936-022-00960-7