Abstract
Purpose of Review
This study reviews contemporary literature on RASP and HoLEP to evaluate perioperative outcomes, common complications, cost analytics, and future directions of both procedures.
Recent Findings
RASP is indicated for prostates > 80 mL, while HoLEP is size-independent. No notable differences were found in operative time, PSA nadir (surrogate for enucleation volume), re-catheterization rates, or long-term durability. Prolonged incontinence and bladder neck contracture rates are low for both surgeries. Patients experience similar satisfaction outcomes and improvements in uroflowmetry and post-void residual volumes. HoLEP demonstrates shorter hospitalizations, lower transfusion rates, lower costs, and higher rates of same-day discharge. RASP offers a shorter learning curve and lower rates of early postoperative urinary incontinence.
Summary
HoLEP is a size-independent surgery that offers advantages for patients seeking a minimally invasive procedure with the potential for catheter-free same-day discharge. Future directions with single-port simple prostatectomy may offer parity in same-day discharge, but further research is needed to determine broader feasibility.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The number of surgical options for patients with lower urinary tract symptoms (LUTS) due to benign prostatic hyperplasia (BPH) has increased significantly in recent years. Treatment choice depends highly on anatomic considerations, patient preference, and risk profile; however, prostate volume remains one of the most important considerations when weighing the ideal surgical modality. Benign prostatic obstruction in large prostate glands (> 80 mL) is best managed with enucleation-based techniques [1]. Although open simple prostatectomy remains a standard treatment, robotic-assisted simple prostatectomy (RASP) and holmium laser enucleation of the prostate (HoLEP) demonstrated superiority to this surgical approach with regard to perioperative morbidity [2]. Mariano et al. [3] reported on the first laparoscopic simple prostatectomy in 2002. By 2008, Sotelo et al. [4] published on the first robotic-assisted simple prostatectomy. Conversely, Peter Gilling was the first to publish on HoLEP in 1996 [5]. Both procedures have undergone reiterations over time with advancements in laser technology and robotic platforms for HoLEP and RASP, respectively. Despite considerable growing interest in these two approaches, prospective randomized control studies are lacking to compare outcomes. This study aims to address contemporary literature to evaluate similarities and differences between RASP and HoLEP. We review recent literature on perioperative and longer-term postoperative outcomes, common complications, cost analytics, and future directions of both procedures.
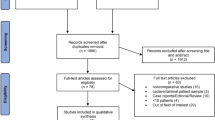
Methods and Materials
A literature search was performed using PubMed and Ovid to identify leading articles for RASP and HoLEP published between 2017 and 2022. 4 major articles directly comparing RASP and HoLEP data were identified. A total of 36 articles citing relevant topics related to both RASP and HoLEP were identified, and the articles were searched for supporting comparative evidence.
Results and Discussion
Perioperative Outcomes
Four publications exist directly comparing outcomes between HoLEP and RASP (Table 1). Of these four articles, only one is a prospective randomized study—published in 2021. The remainder is based on retrospective chart reviews or analysis of prospectively collected data.
Operating Time
Most studies comparing HoLEP to RASP suggest that there is no significant difference in the operating time between the procedures (Tables 2 and 3). Of the included studies, the range of mean operating time ranged from 105 to 140 min. The mean operating time for RASP ranged from 105 to 274 min. The only study that reported a difference in operating time was Zhang et al. [6] who contribute a higher mean operating time to two of their RASP patients that had outlier times from patients with a prostate gland greater than 200 mL. While each procedure has a different learning curve, the same authors also analyzed the dates of each operation with operative time and found no difference, suggesting that the learning curve by trainees may not contribute to the length of the operation.
Length of Hospitalization
Length of hospitalization has been found to be one of the consistent differences between the two surgical techniques among the published literature. All four included studies found a significant difference in the length of hospitalization, with HoLEP patients ranging from 1.3 to 2.5 days, and RASP patients ranging from 3.8 to 7.1 days. While this data is largely influenced by different discharge protocols among the participating institutions, it seems that the shorter length of stay in HoLEP patients results from the advantageous hemostatic control with the endoscopic technique. One reason for hospital admission after these procedures is the need for continuous bladder irrigation (CBI), and HoLEP patients typically only require CBI for less than 24 h, while RASP patients may require CBI for up to 1–2 days [6].
Length of Catheterization
Duration of catheterization has proven to be a significant differentiating factor between HoLEP and RASP. The average catheterization time for HoLEP ranged from 0.7 to 2.5 days, while RASP patients ranged from 3 to 8 days. The wide range observed in published data from patients that underwent RASP is largely due to variations in institutional practices, such as a requirement of in-office cystogram before catheter removal [6]. Despite these discrepancies, the use of a cystotomy during RASP and the previously mentioned hemostatic advantage of HoLEP largely factor into this observed difference between patient populations [7••].
Transfusion Rates
Postoperative blood transfusions are relatively uncommon between these two procedures, and therefore published data is limited by the smaller patient cohorts. Zhang et al. [6] reported a significant difference in transfusion rates between HoLEP and RASP patients (1.8% vs 9.4%, p = 0.03, respectively). Of note, some studies with no observed difference in transfusion rates but did measure significantly lower postoperative changes in hemoglobin among HoLEP patients. Larger patient series may better elucidate if there is an increased risk of blood transfusion following RASP, or if the observed reductions in postoperative hemoglobin are mild enough to not warrant transfusion.
Re-catheterization Rates
Re-catheterization rates for acute urinary retention is another metric of interest for surgical treatment of BPH. Of the three studies that measured re-catheterization rate, no studies found a significant difference between HoLEP patients vs RASP patients. The reported rates ranged from 0 to 2% in HoLEP patients and 0–6% in RASP patients (Tables 1 and 2).
Post-operative Outcomes
Urinary Incontinence Rates
Urinary incontinence can be challenging to accurately quantify and reporting is rarely uniform between institutions. Some authors have attempted to create standardized methods for quantifying SUI severity with systems such as the Male Stress Incontinence Grading Scale (MSIGS), but no uniform survey was utilized among the studies in this article [8]. As such, rates of post-operative incontinence may vary widely among studies due to data collection criteria, but it is important to note that postoperative urinary incontinence is an important consideration for both surgeries.
Transient SUI is a known sequelae of HoLEP that usually resolves within the first year. Kim et al. [7••] reported on the presence of transient stress UI at the 1-month visit being 15.4% and 3% for the HoLEP and RASP groups, respectively (p = 0.09). At 2 months the rate remained at 15.4% for the HoLEP group while zero patients in the RASP group endorsed incontinence (p = 0.03). Alternatively, Kordan et al. [9•] reported urinary incontinence ranging from 10 to 25.7% for RASP patients; however, this was at a less than 3-month follow-up. In other series, urinary incontinence after RASP is reported to be around 1%. Umari et al. [10] note transient urinary incontinence in 8.9% of patients following HoLEP and 1.2% for those after RASP. One notable advantage of RASP is that adenoma is removed without manipulation of the sphincteric mechanism while HoLEP is done via a transurethral approach that increases the risk of transient injury to the external sphincter. Fuschi et al. [11••] reported 4 of their 42 HoLEP patients and 5 of their 32 RASP patients reported stress urinary incontinence at their initial 1-month follow-up, all of which resolved with pelvic floor rehabilitation by the 3-month mark. More recently, Castellani et al. [12] performed a systematic review and meta-analysis of 28 studies characterizing post-operative incontinence rates following transurethral prostate surgery. The study tracked incontinence categories by transient (< 6 months) and persistent (> 6 months) and evaluated for urge, stress, and mixed incontinence. Transient stress, urge and mixed urinary incontinence were 6.0%, 7.3%, and 0.9% among transurethral enucleation patients. Persistent rates for stress, urge, and mixed were reported at 1.7%, 0%, and 0%, respectively.
More recently, en bloc early apical release techniques have been proposed for HoLEP [13]. Some surgeons have theorized this approach may improve early post-operative SUI rates by releasing tension on the external urinary sphincter early in the procedure. Minagawa et al. [14] published on a cohort of 65 patients who underwent en bloc HoLEP and reported 3-month post-operative incontinence in 1 patient. The patient’s continence improved by month 5 post-op. Press et al. [15] recently published a retrospective review of 95 HoLEPs performed by a single surgeon—49 patients underwent standard two-lobe HoLEP and 46 underwent early apical release. This study demonstrated no difference in urinary incontinence rates between the two groups (85.37% vs. 70.0% at 3 months, 73.07% vs. 76.0% at 6 months, and 91.3% and 90.0% at 12 months).
International Prostate Symptom Score (IPSS) Improvements
The IPSS is a well-recognized metric of success after the treatment of BOO. Umari et al. [10] reported no significant difference in symptom scores after HoLEP or RASP with a median of 3 and 5 for HoLEP and RASP, respectively (p = 0.8). In their multicenter prospective randomized study, Fuschi et al. [11••] reported on enucleation procedures for prostates > 120 mL. They found similar symptom scores in patients who underwent HoLEP and RASP (8.26 vs 8.09). Kim et al. [7••] also reported no difference in IPSS with HoLEP patients having a mean score of 9.4 and RASP patients 10.9 (p = 0.29).
Objective Data Measurements: Uroflowmetry and Post-Void Residual
Maximum flow rate (Qmax) and post-void residual urine (PVR) have been reported to be similar after HoLEP and RASP. Kim et al. [7••] reported no difference in mean Qmax (13.2 and 13.4 mL/s, p = 0.92) and mean PVR (98.9 and 127.2 mL, p = 0.38) after HoLEP and RASP, respectively, with a follow-up of at least 6 months. Fuschi et al. [11••] also reported similar functional outcomes with mean Qmax 20.02 ml/s after HoLEP and 19.45 ml/s after RASP at a 3-month follow-up. Mean PVR was also similar with HoLEP patient residuals measuring 35.47 ml and RASP 31.21 ml. Li et al. [16] reported on the efficacy of MISP compared to endoscopic enucleation of the prostate in which they were able to include eight comparative trials with over 1500 patients. In doing so they noted no difference in functional outcomes of Qmax and PVR between MISP and EEP at 3 months. They did note the EEP group had statistically significant lower PVR at the 6-month mark (p < 0.001); however, Qmax was still comparable between the two groups.
PSA Nadir
PSA nadir is a measure used to estimate residual prostatic tissue after prostate surgery. Umari et al. [10] noted similar median PSA nadir in HoLEP vs RASP (1.00 vs 1.09, p = 0.9) consistent with a minimal amount of prostatic tissue being present after either surgery. As an alternative to PSA nadir, other studies reported the PSA drop which can also be used as an adjunct to the amount of prostate tissue removed. Kim et al. [7••] noted a similar decrease in PSA levels between HoLEP and RASP patients (6.39 vs 4.66, respectively, p = 0.14). Comparatively, Fuschi et al. [11••] noted a similar PSA drop between HoLEP and RASP patients as well (3.11 vs 3.09, respectively).
Long-term Durability
Both RASP and HoLEP have demonstrated strong long-term durability due to their similarly high rates of adenoma removal. In a large retrospective analysis of 949 patients, Elmansy et al. [17] reported on 10-year follow-up data for HoLEP and found a 0.7% reoperation rate due to residual adenoma. More recently, 5-year retreatment rates between HoLEP and RASP were compared in a 2022 publication by Wymer et al. [18••] For glands > 80 mL, the probability of retreatment for both HoLEP and simple prostatectomy was 2%. For glands < 80 mL, the HoLEP retreatment rate was 1.3%.
Sexual Function Outcomes
Erectile Dysfunction
Erectile dysfunction has been studied in both RASP and HoLEP. Fuschi et al. [11••] reported statistically significant improvement in both RASP and HoLEP patient’s erectile function with no significant differences between the two groups at 6-, 12-, and 24-month follow-ups. Placer et al. [19] published a retrospective analysis of 202 sexually active patients who underwent HoLEP. Pre and post-operative erection quality scores did not differ significantly for these men; however, 6.9% of patients reported a > 5 point increase on their IIEF-5 scores while 12.4% reported a > 5 decrease in their scores. Elshal et al. [20] performed a prospective study on 80 HoLEP patients and 70 control patients to assess sexual function outcomes following HoLEP. They demonstrated no difference in erectile function scores postoperatively between control patients and HoLEP patients. Li et al. [21] performed a systematic review and meta-analysis of surgical treatments for BPH and reported that all forms of simple prostatectomy yielded no change in erectile function while transurethral enucleation techniques benefited erectile function.
Retrograde Ejaculation
Retrograde ejaculation (RE) is a side effect in the majority of BPH surgeries. The pathophysiology of this surgical outcome is likely due to the removal of periverumontanal prostatic tissue [22]. Gild et al. [23] studied the effects of HoLEP in a retrospective review of 2131 patients who underwent surgery between 2006 and 2015. At a median follow-up of 50 months, 92.5% of patients reported RE. Despite the high percentage of RE, the study reported that it was not associated with overall sexual satisfaction. Studies characterizing ejaculatory dysfunction following RASP are lacking. One prospective study, published in 2021, describes a technique of urethral-sparing RASP to preserve ejaculatory function [24•]. This study reported ejaculatory function outcomes of 92 patients who underwent this procedure and reported that 81% maintained antegrade ejaculation compared to 8.8% in the control group. It is important to note that this novel technique has not been widely adopted yet.
Complication Comparison
Bladder Neck Contracture
Elsaqa et al. [25] reported in their dual center study a development of BNC in 1.87% of HoLEP patients. In their 18-year experience with over 1400 patients and median follow-up of 9 years, Ibrahim et al. [26] reported BNC in 2.1% of their patients. Kordan et al. [9•] reported BNC in less than 1% of patients after RASP in their systematic review with one included study reporting BNC in as few as three out of 487 RASP patients. Kim et al. [7••] reported one of 33 patients required urethrotomy 3 months after RASP for bladder neck contracture. They attributed this to an initial attempt to create a smaller bladder neck similar to open retropubic simple prostatectomy to reduce postoperative hematuria. Once the authors increased the size of the bladder neck no further contractures were noted.
Prolonged Incontinence Rates
Fuschi et al. [11••] reported all patients included in their study of both RASP and HoLEP procedures reported no SUI at 90-day follow-up. Umari et al. [10] report none of the 126 patients in their study suffered from permanent SUI. Similarly, Castellani et al. [12] reported low rates of prolonged SUI in HoLEP patients at around 1.7%—this demonstrated no statistically significant difference to other transurethral procedures.
Special Considerations and Emerging Trends
Anticoagulation
There is no study directly comparing perioperative bleeding risk between RASP and HoLEP. Although several studies have explored the feasibility of HoLEP in the anticoagulated patient population, literature on RASP and anticoagulation is sparse. Deuker et al. [27•] performed a prospective study on 268 HoLEP patients between November 2017 and November 2019. They studied patients in 4 separate groups—no anticoagulation, perioperative platelet aggregation inhibitor (PAI) usage, perioperative novel oral anticoagulant (NOAC) usage, and low molecular weight heparins (LMWH). This publication noted no significant difference in catheter duration or operative time between these groups. The overall 30-day complication rate was 19.5% in the no-anticoagulation group and 26.1% vs. 27.3% vs. 46.2% in patients on PAI, NOACs, and LMWH, respectively. Notably, there was no significant difference in Clavien-Dindo IIIb complications or greater. Only 1 patient (1% of anticoagulation population) required a blood transfusion.
Agarwal et al. [28] performed a retrospective review of 472 HoLEP procedures performed at a single institution between July 2018 to December 2019. Patients were grouped into no anticoagulation/antiplatelet, antiplatelet (AP), and anticoagulant (AC) populations. 90% of the anticoagulation patients and 97% of the antiplatelet patients held their medication perioperatively. There was a statistically significant difference in postoperative complications, but not for postoperative emergency department visits or Clavien 3 or higher complications. Interestingly, there was no significant difference noted between the three groups regarding transfusion rates or clot evacuations. Overall, these studies reinforce that the anticoagulated patient population presents a series of unique challenges to the urologist, but HoLEP is a viable treatment option (Fig. 1).
Same Day Discharge
Rising hospitalization costs and more recent constraints related to the COVID-19 pandemic have increased interest in reducing the length of hospitalization for both RASP and HoLEP. Lwin et al. [29] published the first study on same-day surgery for HoLEP in 2020. This group retrospectively studied 377 HoLEP patients between 2013 and 2018 and identified 199 same-day surgery (SDS) and 178 non-SDS patients. SDS was defined as discharge directly from the post-anesthesia care unit. The average prostate volume of the SDS cohort was 89 mL with an average length of stay of 3.9 h. The average catheterization time was 32 h between both groups. No statistically significant difference was noted in postoperative complication or 30-day readmission rates between SDS and non-SDS patients. In 2022, Slade et al. [30•] reported on outcomes data of same-day catheter removal and discharge for HoLEP patients. Same-day catheter removal for 114 HoLEP patients with a mean prostate volume of 109.2 mL was 87.7%. Patients with ASA 3 or 4 were noted to be at higher risk for failure of the same-day void trial.
Assmus et al. [31•] published on HoLEP same-day discharge on > 175 mL glands in 2021. This study retrospectively reviewed 55 patients with > 175 mL prostates between December 2019 and September 2020. Thirty-eight of fifty-five patients were discharged the same day as surgery with an average length of stay of 2.7 h and catheterization time of 16.7 h. This study reported a 3.6% rate of 30-day postoperative emergency department visits and only 1 post-operative readmission.
With the introduction of the single port Davinci platform in 2018, same-day RASP has been reported. The first SP trans vesical simple prostatectomy was introduced by Kaouk et al. [32] in 2020, and due to the ability to avoid entering the peritoneal cavity, outcomes have demonstrated higher ability to discharge patients on the same day of surgery. Zeinab et al. [33•] recently published on multi-institutional outcomes of 91 patients who underwent SP transvesical RASP. The average prostate volume was 156 mL with mean operative time of 159 min. The median postoperative hospitalization time was 21.0 h with 42% of patients being discharged on the same day of surgery. The average foley catheter duration was 5 days.
Learning Curve
Kampantais et al. [34] published a systematic review in 2018 of 28 studies to estimate the learning curve for HoLEP. They concluded that proficiency with the procedure requires approximately 50 cases with appropriately selected patients (prostates < 80 mL, excluding post-radiotherapy, anticoagulated, or catheter-dependent patients). However, with mentored training, proficiency may be achieved in a few as 25 or fewer cases. Johnson et al. [35] performed a retrospective review of 120 consecutive RASP cases by two experienced robotic surgeons between 2014 and 2017 and estimated the learning curve to be between 10 and 12 cases. However, it is important to note this is a learning curve among experienced robotic surgeons, and we must consider a baseline learning curve for robotic surgery. A reasonable surrogate for this is the current Accreditation Council for Graduate Medical Education (ACGME) procedure numbers for urology that require a minimum of 80 robotic-assisted procedures to graduate with acceptable minimal experience.
Cost Comparison
Holmium laser enucleation requires investment in a holmium laser system and a morcellator. While there are several companies that manufacture laser systems, our institution currently utilizes the 120-W MOSES™ 2.0 system from Boston Scientific and the Wolf Piranha morcellator. Pricing for these machines varies based on health system contracts, but initial investments in both devices are far less than the Davinci surgical system which requires considerably higher upfront costs. Between the various models, the average cost is approximately $1.5 million USD with average annual service costs of around $150,000 [36].
Head-to-head prospective cost comparisons of HoLEP and RASP have not been published to date. Information we can gather about these surgeries can only be compared by independent articles that do not compare costs at the same institution or gather costs from large national databases. Wymer et al. [18••] published on surgical cost-effectiveness between HoLEP and simple prostatectomy for prostates greater than 80 mL. This study evaluated 2021 Medicare reimbursement rates and included costs for the index procedure, complications, and retreatment. HoLEP fees were based on outpatient facilities fees and physicians’ fees determined by CPT codes while SP procedure costs were based on inpatient facility fees through diagnosis-related group coding. Procedural outcome data was based on published metanalyses comparing functional outcomes and complications of these procedures. The 5-year post-index procedure cost for HoLEP was $6585.46 versus $15,404.40. In the less than 80 mL cohort, HoLEP costs average $6531.89. Simple prostatectomy was not included in the smaller gland cohort. Of all procedures included in this study, HoLEP was the most cost-effective among TURP, photovaporization of the prostate, water vapor thermal therapy, and prostatic urethral lift. Due to CPT code limitations, this study did not distinguish between OSP and RASP; however, a 2015 study by Sutherland et al. [37] compared cost outcomes between OSP and RASP and noted RASP to cost on average $2797 more than open simple prostatectomy.
Conclusion
Enucleation is the most definitive method for managing symptomatic large-volume prostate hyperplasia. RASP and HoLEP offer similar treatment outcomes with regards to tissue resected, IPSS improvement, uroflowmetry, and post-void residual values. There appears to be no significant difference in bladder neck contracture rates or long-term post-operative urinary incontinence complications. Data is lacking on comparing rates of retrograde ejaculation, but the published literature cites high rates for both procedures, although urethral sparing simple prostatectomy appears to offer significantly improved antegrade ejaculation rates. The literature reflects that HoLEP offers shorter hospitalizations, lower transfusion rates, shorter catheterization time, lower costs, and higher rates of same-day discharge. Additionally, HoLEP has proven to be a feasible option for therapeutically anticoagulated patients. The demand for safe and effective surgical management in large-volume prostates continues to rise. The urologic community must explore ways to increase patient access to the most appropriate intervention for each patient. As both procedures continue to undergo innovations, prospective randomized trials will be indicated to properly compare their outcomes.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Lerner LB, McVary KT, Barry MJ, Bixler BR, Dahm P, Das AK, et al. Management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA GUIDELINE PART II-Surgical Evaluation and Treatment. J Urol. 2021;206(4):818–26.
Anderson BB, Heiman J, Large T, Lingeman J, Krambeck A. Trends and perioperative outcomes across major benign prostatic hyperplasia procedures from the ACS-NSQIP 2011–2015. J Endourol. 2019;33(1):62–8.
Mariano MB, Graziottin TM, Tefilli MV. Laparoscopic prostatectomy with vascular control for benign prostatic hyperplasia. J Urol. 2002;167(6):2528–9.
Sotelo R, Clavijo R, Carmona O, Garcia A, Banda E, Miranda M, et al. Robotic simple prostatectomy. J Urol. 2008;179(2):513–5.
Gilling PJ, Cass CB, Cresswell MD, Fraundorfer MR. Holmium laser resection of the prostate: preliminary results of a new method for the treatment of benign prostatic hyperplasia. Urology. 1996;47(1):48–51.
Zhang MW, El Tayeb MM, Borofsky MS, Dauw CA, Wagner KR, Lowry PS, et al. Comparison of perioperative outcomes between holmium laser enucleation of the prostate and robot-assisted simple prostatectomy. J Endourol. 2017;31(9):847–50.
•• Kim BH, Byun HJ. Robotic-assisted simple prostatectomy versus holmium laser enucleation of the prostate for large benign prostatic hyperplasia: a single-center preliminary study in Korea. Prostate Int. 2022;10(3):123–8. This is a new article published in September 2022 and is one of only 4 studies to date directly comparing HoLEP and RASP.
Morey A, Singla N, Chung P, Klein A, Tausch T, Siegel J, et al. Male stress incontinence grading scale (MSIGS) for evaluation of men with post-prostatectomy incontinence: a pilot study. Video J Prosthet Urol. 2016;2.
• Kordan Y, Canda AE, Koseoglu E, Balbay D, Laguna MP, de la Rosette J. Robotic-assisted simple prostatectomy: a systematic review. J Clin Med. 2020;9(6). Thorough review article discussing RASP.
Umari P, Fossati N, Gandaglia G, Pokorny M, De Groote R, Geurts N, et al. Robotic assisted simple prostatectomy versus holmium laser enucleation of the prostate for lower urinary tract symptoms in patients with large volume prostate: a comparative analysis from a high volume center. J Urol. 2017;197(4):1108–14.
•• Fuschi A, Al Salhi Y, Velotti G, Capone L, Martoccia A, Suraci PP, et al. Holmium laser enucleation of prostate versus minimally invasive simple prostatectomy for large volume (>/=120 mL) prostate glands: a prospective multicenter randomized study. Minerva Urol Nephrol. 2021;73(5):638–48. This is the only prospective randomized study to date comparing RASP and HoLEP.
Castellani D, Rubilotta E, Fabiani A, Maggi M, Wroclawski ML, Teoh JY, et al. Correlation between transurethral interventions and their influence on type and duration of postoperative urinary incontinence: results from a systematic review and meta-analysis of comparative studies. J Endourol. 2022;36(10):1331–47.
Scoffone CM, Cracco CM. The en-bloc no-touch holmium laser enucleation of the prostate (HoLEP) technique. World J Urol. 2016;34(8):1175–81.
Minagawa S, Okada S, Sakamoto H, Toyofuku K, Morikawa H. En-Bloc technique with anteroposterior dissection holmium laser enucleation of the prostate allows a short operative time and acceptable outcomes. Urology. 2015;86(3):628–33.
Press B, Ghiraldi E, Kim DD, Nair H, Johnson K, Kellner D. “En-Bloc” enucleation with early apical release compared to standard holmium laser enucleation of the prostate: a retrospective pilot study during the initial learning curve of a single surgeon. Urology. 2022;165:275–9.
Li J, Cao D, Meng C, Xia Z, Peng L, Li Y, et al. Comparison of the efficacy and safety of minimally invasive simple prostatectomy and endoscopic enucleation of prostate for large benign prostatic hyperplasia. Front Med (Lausanne). 2021;8:773257.
Elmansy HM, Kotb A, Elhilali MM. Holmium laser enucleation of the prostate: long-term durability of clinical outcomes and complication rates during 10 years of followup. J Urol. 2011;186(5):1972–6.
•• Wymer KM, Narang G, Slade A, Sharma V, Thao V, Borah BJ, et al. Evaluation of the cost-effectiveness of surgical treatment options for benign prostatic hyperplasia. Urology. 2022. Well organized and thought-out article discussing BPH treatment costs.
Placer J, Salvador C, Planas J, Trilla E, Lorente D, Celma A, et al. Effects of holmium laser enucleation of the prostate on sexual function. J Endourol. 2015;29(3):332–9.
Elshal AM, El-Assmy A, Mekkawy R, Taha DE, El-Nahas AR, Laymon M, El-Kappany H, Ibrahiem EH. Prospective controlled assessment of men’s sexual function changes following holmium laser enucleation of the prostate for treatment of benign prostate hyperplasia. Int Urol Nephrol. 2017;49(10):1741–9. https://doi.org/10.1007/s11255-017-1649-0. Epub 2017 Aug 5 PMID: 28780626.
Li Z, Chen P, Wang J, Mao Q, Xiang H, Wang X, et al. The impact of surgical treatments for lower urinary tract symptoms/benign prostatic hyperplasia on male erectile function: a systematic review and network meta-analysis. Medicine (Baltimore). 2016;95(24): e3862.
Couteau N, Duquesne I, Frederic P, Thiounn N, Timsit MO, Mejean A, et al. Ejaculations and benign prostatic hyperplasia: an impossible compromise? A comprehensive review. J Clin Med. 2021;10(24).
Gild P, Dahlem R, Pompe RS, Soave A, Vetterlein MW, Ludwig TA, et al. Retrograde ejaculation after holmium laser enucleation of the prostate (HoLEP)-Impact on sexual function and evaluation of patient bother using validated questionnaires. Andrology. 2020;8(6):1779–86.
• Porpiglia F, Checcucci E, Amparore D, Niculescu G, Volpi G, Piramide F, et al. Urethral-sparing robot-assisted simple prostatectomy: an innovative technique to preserve ejaculatory function overcoming the limitation of the standard millin approach. Eur Urol. 2021;80(2):222–33. Recently published article discussing novel urethral-sparing approach to address retrograde ejaculation in RASP patients.
Elsaqa M, Serag M, Leenlani N, Elsawy MM, Sakr M, Youssif TA, et al. The incidence of urethral stricture and bladder neck contracture with transurethral resection vs. holmium laser enucleation of prostate: a matched, dual-center study. Can Urol Assoc J. 2022.
Ibrahim A, Alharbi M, Elhilali MM, Aube M, Carrier S. 18 years of holmium laser enucleation of the prostate: a single center experience. J Urol. 2019;202(4):795–800.
• Deuker M, Ruhrup J, Karakiewicz PI, Welte M, Kluth LA, Banek S, et al. Holmium laser enucleation of the prostate: efficacy, safety and preoperative management in patients presenting with anticoagulation therapy. World J Urol. 2021;39(4):1219–26. Recently published article discussing feasibility of HoLEP in the anticoagulated patient population.
Agarwal DK, Large T, Stoughton CL, Heiman JM, Nottingham CU, Rivera ME, et al. Real-world experience of holmium laser enucleation of the prostate with patients on anticoagulation therapy. J Endourol. 2021;35(7):1036–41.
Lwin AA, Zeng J, Evans P, Phung MC, Hynes KA, Price ET, et al. Holmium laser enucleation of the prostate is safe and feasible as a same day surgery. Urology. 2020;138:119–24.
• Slade A, Agarwal D, Large T, Sahm E, Schmidt J, Rivera M. Expanded criteria same day catheter removal after holmium laser enucleation of the prostate. J Endourol. 2022;36(7):977–81. Follow-up data discussing a single center experience at same-day catheter removal and discharge for HoLEP patients.
• Assmus MA, Large T, Lee MS, Agarwal DK, Rivera ME, Krambeck AE. Same-day discharge following holmium laser enucleation in patients assessed to have large gland prostates (>/=175 cc). J Endourol. 2021;35(9):1386–92. First of its kind study focusing on same-day discharge following HoLEP for large volume prostates.
Kaouk J, Sawczyn G, Wilson C, Aminsharifi A, Fareed K, Garisto J, et al. Single-port percutaneous transvesical simple prostatectomy using the sp robotic system: initial clinical experience. Urology. 2020;141:173–7.
• Abou Zeinab M, Beksac AT, Corse T, Talamini S, Morgantini L, Kaviani A, et al. The multi-institutional experience in single-port robotic transvesical simple prostatectomy for benign prostatic hyperplasia management. J Urol. 2022;208(2):369–78. Recent publication from leading author on single-port robotic surgery describing outcomes for single-port RASP.
Kampantais S, Dimopoulos P, Tasleem A, Acher P, Gordon K, Young A. Assessing the learning curve of holmium laser enucleation of prostate (HoLEP). A systematic review Urology. 2018;120:9–22.
Johnson B, Sorokin I, Singla N, Roehrborn C, Gahan JC. Determining the learning curve for robot-assisted simple prostatectomy in surgeons familiar with robotic surgery. J Endourol. 2018;32(9):865–70.
Feldstein J, Schwander B, Roberts M, Coussons H. Cost of ownership assessment for a da Vinci robot based on US real-world data. Int J Med Robot. 2019;15(5): e2023.
Sutherland DE, Perez DS, Weeks DC. Robot-assisted simple prostatectomy for severe benign prostatic hyperplasia. J Endourol. 2011;25(4):641–4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Marcelino Rivera is a consultant for Boston Scientific Corporation and Cook Medical. The remaining authors have no disclosures.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Benign Prostatic Hyperplasia
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shelton, T.M., Drake, C., Vasquez, R. et al. Comparison of Contemporary Surgical Outcomes Between Holmium Laser Enucleation of the Prostate and Robotic-Assisted Simple Prostatectomy. Curr Urol Rep 24, 221–229 (2023). https://doi.org/10.1007/s11934-023-01146-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11934-023-01146-9