Abstract
Purpose of Review
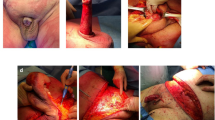
Adult acquired buried penis is a morbid condition characterized by complete entrapment of the phallus as a result of morbid obesity, post-surgical cicatrix formation, or primary genital lymphedema. Hygienic voiding is not possible and urinary dribbling is frequent with accompanying inflammation, skin breakdown, and infection from the chronic moisture. The end result is penile skin fibrosis resulting in permanent functional loss. Herein, we describe the etiology of adult acquired buried penis, advances in its surgical management, and quality of life outcomes with treatment.
Recent Findings
Adult acquired buried penis is increasing in incidence as morbid obesity becomes more prevalent. Frequently comorbid conditions affect treatment including those affecting wound healing such a diabetes mellitus. Functional and cosmetic surgical outcomes are being published in greater volume in recent years leading to more refined treatment algorithms. Patient quality of life is greatly improved by definitive surgical management.
Summary
Adult acquired buried penis is a morbid condition that is increasing in incidence as obesity becomes more commonplace. Surgical management often necessitates surgical lipectomy of the suprapubic fat pad, scrotoplasty, and penile split thickness skin graft. Substantial quality of life improvements have been consistently reported after surgical treatment.




Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Pestana I, Greenfield J, Walsh M, et al. Management of “buried” penis in adulthood: an overview. Plast Reconstr Surg. 2009;124(4):1186–95.
Zimmerman W, Santucci R. Treatment of adult-acquired buried penis. Skin grafts—indications, applications and current research - Chapter 12, InTech. 2011.
Rybak J, Larsen S, Yu M. Levine LA single center outcomes after reconstructive surgical correction of adult acquired buried penis: measurements of erectile function, depression, and quality of life. J Sex Med. 2014;11(4):1806–91.
•• Voznesensky M, Lawrence W, Erickson B. Patient-reported social, psychological, and urologic outcomes after adult buried penis repair. Urology. 2017;103:240–4. There have been several studies on the post-operative psychosocial effects and quality of life improvements on patients after correction of buried penis, however this study specifically highlighted a few of the quality of life measures that we believe should be included as part of the standard post-operative assessment of our buried penis patient population. Particularly in this study, urinary function and sexual function are two important parameters that were added as a modification to the Post-Bariatric Surgery Quality of Life Questionnaire (PBSQoL), a survey that has been used by other groups in studying quality of life in these patients. These are two very important factors that should be considered in all patients pre- and post-operatively and we feel strongly that although there is not currently a standardized quality of life survey for the buried penis population, urinary and sexual function are imperative to include in the evaluation of these patients.
Hughes D, Perez E, Garcia R, et al. Sexual and overall quality of life improvements after surgical correction of “buried penis”. Ann Plast Surg. 2016;76(5):532–5.
• Liaw A, Rickborn L, McClung C Incidence of Urethral Stricture in Patients with Adult Acquired Buried Penis. Adv Urol. Epub 2017. Concomitant urethral stricture disease in patients undergoing evaluation for AABP has not been studied extensively, but given that both urethral stricture disease and buried penis are managed by reconstructive urologists, it seems that this is an important aspect to the evaluation of AABP patients. In this study, 33 percent of patients that met the criteria for buried penis had associated urethral stricture disease, most commonly at the meatus/fossa navicularis (62%). We wanted to highlight an area of buried penis work-up and management that may be grossly under-evaluated in the community.
Donatucci C, Ritter E. Management of the buried penis in adults. J Urol. 1998;159(2):420–4.
Alter GJ, Ehrlich RM. New technique for correction of the hidden penis in children and adults. J Urol. 1999;161(2):455–9.
•• Tausch T, Tahibana I, Siegel J, et al. Classification System for Individualized Treatment of Adult Buried Penis Syndrome. Plast Reconstr Surg. 2016;138(3):703–11. The large number of patients in this study provided an excellent opportunity to further target therapy for Adult Acquired Buried Penis to the individual patient. This study provided a classification system that established appropriate interventions based on physical variations within the spectrum of adult buried penis syndrome. Fifty-six patients were selected and patients were stratified based on whether their penile skin was viable or non-viable, as well as if genital lymphedema was present with further subcategories that influenced surgical decision making – such as whether to use a split thickness skin graft or perform scrotoplasty. More importantly, it highlights the importance of the surgeon’s attention to various pathologic factors and surgical decision-making that ultimately increase the chance of success of this operation.
Tsourdi E, Barthel A, Rietzsch H, et al. Current aspects in the pathophysiology and treatment of chronic wounds in diabetes mellitus. Biomed Res Int. 2013;385641:2013.
Greenhalgh DG. Wound healing and diabetes mellitus. Clin Plast Surg. 2003;30(1):37–45.
Laitiff AA, Teoh SL, Das S. Wound healing in diabetes mellitus: traditional treatment modalities. Clin Ter. 2010;161(4):359–64.
Westerman ME, Tausch TJ, Zhao LC, Siegel JA, Starke N, Klein AK, et al. Ventral slit scrotal flap: a new outpatient surgical option for reconstruction of adult buried penis syndrome. Urology. 2015;85(6):1501–4. https://doi.org/10.1016/j.urology.2015.02.030.
Stokes TH, Follmar KE, Silverstein AD, Weizer AZ, Donatucci CF, Anderson EE, et al. Use of negative-pressure dressings and split-thickness skin grafts following penile shaft reduction and reduction scrotoplasty in the management of penoscrotal elephantiasis. Ann Plast Surg. 2006;56(6):649–53. https://doi.org/10.1097/01.sap.0000202826.61782.c9.
Weinfeld AB, Kelley P, Yuksel E, et al. Circumferential negative-pressure dressing (VAC) to bolster skin grafts in the reconstruction of the penile shaft and scrotum. Ann Plast Surg. 2005;54(2):178–83.
Senchenkov A, Knoetgen J, Chrouser KL, Nehra A. Application of vacuum-assisted closure dressing in penile skin graft reconstruction. Urology. 2006;67(2):416–9. https://doi.org/10.1016/j.urology.2005.08.037.
Tang S, Kamat D, Santucci R. Modern management of adult-acquired buried penis. Urology. 2008;72(1):124–7. https://doi.org/10.1016/j.urology.2008.01.059.
Brown D, Barton B, Young V, Pruitt B. Decreased wound contraction with fibrin glue-treated skin grafts. Arch Surg. 1992;127(4):404–6. https://doi.org/10.1001/archsurg.1992.01420040046007.
Currie L, Sharpe J, Martin R. The use of fibrin glue in skin grafts and tissue-engineered skin replacements: a review. Plast Reconstr Surg. 2001;108(6):1713–26.
Hughes D, Perez E, Garcia R, et al. Sexual and overall quality of life improvements after surgical correction of “buried penis”. Ann Plas Surg. 2016;76(5):532–5. https://doi.org/10.1097/SAP.0000000000000378.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Thomas W. Fuller, Katherine M. Theisen, Anup Shah, and Paul J. Rusilko each declare no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Surgery
Rights and permissions
About this article
Cite this article
Fuller, T.W., Theisen, K.M., Shah, A. et al. Surgical Management of Adult Acquired Buried Penis. Curr Urol Rep 19, 22 (2018). https://doi.org/10.1007/s11934-018-0768-1
Published:
DOI: https://doi.org/10.1007/s11934-018-0768-1