Abstract
Purpose of Review
Individuals with post-acute sequelae of SARS-CoV-2 (PASC) complain of persistent musculoskeletal pain. Determining how COVID-19 infection produces persistent pain would be valuable for the development of therapeutics aimed at alleviating these symptoms.
Recent Findings
To generate hypotheses regarding neuroimmune interactions in PASC, we used a ligand-receptor interactome to make predictions about how ligands from PBMCs in individuals with COVID-19 communicate with dorsal root ganglia (DRG) neurons to induce persistent pain. In a structured literature review of -omics COVID-19 studies, we identified ligands capable of binding to receptors on DRG neurons, which stimulate signaling pathways including immune cell activation and chemotaxis, the complement system, and type I interferon signaling. The most consistent finding across immune cell types was an upregulation of genes encoding the alarmins S100A8/9 and MHC-I.
Summary
This ligand-receptor interactome, from our hypothesis-generating literature review, can be used to guide future research surrounding mechanisms of PASC-induced pain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Approximately 30% of individuals infected with COVID-19 will develop post-acute sequelae of SARS-CoV-2 infection (PASC) [1,2,3], which impacts a variety of systems and processes including cardiovascular [4], musculoskeletal [5], gastrointestinal [6], and metabolic [7]. To better understand PASC symptomology, large electronic health record databases and survey studies have identified clusters of individuals based on common PASC symptoms. One cluster that has been identified repeatedly consists of those who have a phenotype involving prolonged musculoskeletal pain, and this group comprises 10–30% of individuals with PASC [2, 3, 8, 9]. This musculoskeletal pain is typically accompanied by fatigue and post-exertional malaise that hinders function and engagement in work and social activities. Individuals with PASC report moderate levels of pain severity and individuals with both fibromyalgia and PASC have a higher level of pain severity than individuals with fibromyalgia alone, suggesting PASC can exacerbate pre-existing musculoskeletal pain [8]. However, it is unknown how an acute infection of COVID-19 could produce the musculoskeletal pain associated with PASC. A better understanding of this underlying mechanism could lead to the development of pharmaceuticals or other treatments aimed at relieving PASC-induced musculoskeletal pain.
The peripheral immune system has been heavily implicated in the production of chronic pain. For example, preclinical models of muscle pain demonstrate macrophages are necessary for the generation of muscle hyperalgesia [10,11,12,13], while both monocytes and T cells are involved in the production of neuropathic pain [14]. Alterations in circulating immune cells and increases in pro-inflammatory cytokines have been found in conditions associated with chronic musculoskeletal pain including rheumatoid arthritis [15, 16], osteoarthritis [17, 18], low back pain [19], and fibromyalgia [20,21,22,23]. These peripheral immune cells can produce prolonged hyperalgesia through neuroimmune interactions by increasing pro-inflammatory cytokines and other ligands that can act directly on nociceptors to drive changes in excitability [24]. Given how crucial immune signaling can be in the development of pain states, it is plausible that alterations in the peripheral immune system induced by COVID-19 infection are driving changes in the peripheral somatosensory system to lead to PASC-induced musculoskeletal pain. To identify potential neuroimmune mechanisms linking COVID-19 to the generation of PASC-induced musculoskeletal pain, we ran publicly available single-cell RNA sequencing data sets from peripheral blood mononuclear cells (PBMCs) from individuals with COVID-19 through a ligand-receptor interactome network that we developed previously and optimized for this study [25]. This comprehensive interaction network was built to identify potential connections between different cell types and human DRG (hDRG) sensory neurons to aid the discovery of drug targets for alleviating pain [25]. In this study, we aimed to use our interactome platform to generate predictions on mechanisms through which specific immune cells could produce PASC-induced musculoskeletal pain following COVID-19 infection.
Methods
To comprehensively explore existing data sets using single-cell RNA sequencing on PBMCs from individuals with COVID-19, the following search strategy was used on January 31, 2023, through PubMed: (Single cell [tiab]) AND ((Sequencing [tiab]) OR (seq [tiab])) AND ((COVID [tiab]) OR (SARS-CoV-2 [tiab])) AND (Peripheral blood mononuclear cell). This search strategy returned 161 articles which were subsequently screened for inclusion. We identified 5 publicly available data sets [26,27,28,29,30] from single-cell RNA sequencing data of PBMCs that included differential gene expression (DEG) analysis between individuals with COVID-19 and healthy controls (Table 1). The DEGs from each article were compiled and genes that had contrasting differential expression between articles, within a given immune cell subset, were removed. Upregulated DEGs from individuals with COVID-19 were then run through our ligand-receptor interactome platform which allows for the identification of interactions between specific cell types and receptors on nociceptors of hDRG [25]. The interactome database contains over 3000 ligand-receptor interactions, including lipid and small molecule ligands like prostaglandins and endocannabinoids [25]. Use of this interactome platform allows for the discovery of novel pain mechanisms, which can lead to testable hypotheses for the development of new therapeutic targets for treating chronic pain. For example, using this interactive platform, we previously identified a novel pro-nociceptive action of heparin-binding epidermal growth factor (HBEGF) [25].
Interactions were identified by intersecting the ligand gene list from each immune cell subtype with corresponding hDRG neuron receptors identified previously [31]. Following identification of all interactions between specific immune cells and different hDRG sensory neuron populations, we filtered the list to exclude those interactions in which the receptor was expressed only in non-nociceptive populations or in nociceptors that do not produce symptoms of musculoskeletal pain consistent with PASC, such as TRPM8 positive nociceptors which are believed to be responsible for detecting cold [32]. Thus, our final list of interactions focused on ligands produced from PBMCs that could activate receptors on 4 subsets of nociceptors (putative low threshold mechanosensitive C fibers, silent nociceptors, pro-enkephalin expressing, and transient receptor potential cation channel subfamily A member 1 (TRPA1) positive). Data is presented by grouping all the interactions for a given immune cell population (i.e., All Monocytes) and the interactions of specific immune cell subsets when data was available (i.e., classic, non-classic, and intermediate monocytes). For each immune cell group, each interaction was ranked by an aggregate score accounting for the adjusted p-value for the ligand’s differential expression in COVID-19, the percentage of cells in the group that expressed the ligand in individuals with COVID-19, and the expression levels (in normalized counts) of the respective receptor in hDRG nociceptors. We then performed Gene Ontology (GO) term analysis for the ligand and receptor genes using Enrichr [33, 34] and classified the genes by the PANTHER classification of their protein products [35]. GO term analysis examines all the biological process or molecular function ontology annotations associated with each of the input genes and determines which terms are most enriched for a given set of DEGs, shedding insight into which signaling pathways and biological systems could be activated by the genes of interest. GO terms for biological processes and molecular function were identified and ranked based on adjusted p-value.
Results
Monocytes
Monocytes have been implicated in the etiology of musculoskeletal pain conditions including rheumatoid arthritis [36,37,38,39], osteoarthritis [40,41,42], fibromyalgia [20, 43], and low back pain [44]. Monocytes could play a role in the production of musculoskeletal pain associated with PASC as increased numbers of circulating classic monocytes is one of the hallmark differences found in PBMCs from individuals with COVID-19 [29, 45,46,47]. In moderate cases of COVID-19, there is also a decrease in non-classic monocytes [29, 45]; however, some report increases in non-classic monocytes in severe and fatal cases [48].
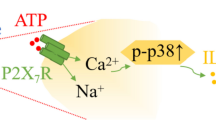
Our interactome analysis revealed similarities and differences between the upregulated genes and pathways in monocyte subsets. Ligands from classic, non-classic, and intermediate monocytes demonstrate increased activation of biological processes with GO terms associated with the immune response, leukocyte chemotaxis, and activation of neutrophils (Fig. 1). Increased circulating neutrophils are also routinely found in individuals with COVID-19 [49]; however, their role in the generation of pain has been debated as some show pro-nociceptive [50, 51] and other anti-nociceptive effects [52]. Classic and intermediate monocytes also show a specific upregulation of the genes S100A8/9 that encode for a class of alarmins that bind to toll-like receptor 4 (TLR4) and drive activation of the innate immune response by increasing cytokine production and release [53] (Fig. 2). S100 proteins are intracellular calcium sensors which are released passively following cellular apoptosis or are actively secreted and signal to initiate pro-inflammatory cascades [54]. S100A8/9 are implicated in the production of pain in animal models of osteoarthritis, rheumatoid arthritis, and intervertebral disc degeneration [55,56,57]. S100A8 administered to cultured mouse DRGs increases production of MCP-1 that promotes a local influx of monocytes in the DRG which could induce sensitization of the DRG neurons and subsequent hypersensitivity [58]. However, recent preclinical work demonstrates that S100A8/9 can reduce pain duration in an animal model of inflammation induced pain, suggesting a potential role in pain resolution [52]. Ligands from classic monocytes also demonstrate activation of antigen processing and presentation through major histocompatibility class I (MHC-I) and an upregulation of the gene PKM both of which suggest increases in phagocytic activity and cell death [59, 60] (Fig. 2). Increases in cell death can cause a release of intracellular contents, notably ATP, which binds to purinergic receptors on nociceptors in the DRGs, which in turn can lead to sensitization and hypersensitivity [61].
Ligand and receptor GO terms from the interactome analysis of immune cells in individuals with COVID-19. Top 5 enriched biological processes and molecular function GO terms based on adjusted p-value for the differentially expressed ligand encoding genes for each PBMC immune cell type. The results are grouped by the ligand and receptor GO terms and then further divided into biological and molecular function and ranked from left to right
Differential expression and interactome analysis of ligands from immune cells in individuals with COVID-19. Differential expression of ligand encoding genes from PBMC immune cells with COVID-19 compared with healthy individuals grouped by immune cell type. The top 5 predicted ligand-receptor interactions are listed for each PBMC immune cell type. Left panel illustrates the percentage of each PBMC immune cell expressing the transcript of the given gene from individuals with COVID-19 (red) and healthy controls (blue). The middle panel illustrates the given differentially expressed ligand gene with its category and the corresponding top receptors for that ligand on human DRGs with its subsequent category. The right panel illustrates the normalized counts of each receptor on different classes of nociceptors (PENK = pro-enkephalin expressing, TRPA1 = transient receptor potential cation channel subfamily A member 1 expressing, silent nociceptors, C_LTMR = putative low threshold mechanoreceptor C fibers) from human DRGs [31]
Non-classic monocytes exhibit upregulation of the gene NAMPT which is involved in producing an inflammatory response through interferon gamma (IFNγ) signaling [62, 63] (Fig. 2). IFNγ is implicated in the production of pain as increased IFNγ-stimulated genes are found in the DRGs of individuals with neuropathic pain [64]. Increased plasma levels of NAMPT are also found in individuals with rheumatoid arthritis [62, 65]. Non-classic monocytes also show an increase in the ligand gene GRN which encodes for the protein progranulin (Fig. 1). This demonstrates the attempted healing action of non-classic monocytes as this gene is involved in wound repair and anti-inflammation [66, 67]. GRN knockout mice demonstrate an increased pain response to nerve injury and progranulin administration shows therapeutic effects in animal models of inflammatory arthritis [68, 69]. In sum, ligands from monocytes show activation of several pathways responsible for leukocyte chemotaxis and pro-inflammatory pathways which could be responsible for the production of musculoskeletal pain. Interestingly, individuals with PASC-induced post-exertional fatigue have increased numbers of monocytes in skeletal muscle, which further supports the notion that alterations in the presence of this cell type, and its signals, could lead to PASC-induced musculoskeletal pain [70].
CD4 T Cells
Following COVID-19 infection, there is an overall decrease in the proportion of CD4 T cells in the blood and further decreases are reported with increased severity of symptoms suggesting dysregulation in immune response in severe cases [47,48,49]. While the total number of CD4 T cells may decrease, there is a reported shift in the phenotype of CD4 T cells with increases in Th1 acutely following infection in those with mild cases [30, 71]. An increase in the proportion of Th2 T cells is reported in severe cases and is a predictor of subsequent hospitalization and death due to COVID-19 [72,73,74]. Animal models of neuropathic pain have extensively studied the role of CD4 T cells in the production of prolonged hypersensitivity and suggest these subsets of CD4 T cells play opposing roles in pain development. Pro-inflammatory Th1 cells seem to promote pain, while anti-inflammatory Th2 cells appear to protect against it. Following nerve injury, there is a subsequent infiltration of CD4 T cells into the DRG [75,76,77] and mice lacking CD4 T cells are protected against the development of hypersensitivity [78]. When rats lacking T cells were reconstituted with Th1 T cells, the pain behaviors were restored but not when reconstitution was performed with Th2 T cells suggesting pro-inflammatory Th1 T cells play a role in the production of pain [79]. Similarly, studies of chronic pain conditions have implicated a causative role for pro-inflammatory CD4 T cells that infiltrate into the painful joints of individuals with rheumatoid arthritis [80,81,82] and osteoarthritis [83,84,85]. Thus, an overall increase in the proportion of Th1 T cells in individuals with COVID-19 could be a factor in the production of PASC-induced musculoskeletal pain.
The genes and GO terms from our interactome analysis demonstrate that ligands from CD4 T cells activate cytokine-mediated signaling, the complement system, and antigen processing and presentation through MHC-I, all of which are implicated in the production of pain (Fig. 1). Pro-inflammatory cytokines such as IL-6, IL-1β, and TNFα can bind to their receptors on nociceptors to cause excitation and sensitization [86, 87]. The complement system is part of the innate immune system, its activation can lead to immune cell recruitment and inflammation, and it is linked to the production of persistent pain through its ability to sensitize nociceptors [88, 89]. Antigen processing and presentation involves immune system communication through either MHC class I or class II signaling [90]. MHC-I is responsible for alerting the immune system that a cell is virally infected so that it can be tagged for destruction [91]. B2M and HLA-C, both of which are genes encoding components of the MHC-I protein, were the ligands for two of the top predicted interactions between CD4 T cells and DRGs (Fig. 2). Genetic variants in B2M are associated with neuropathic pain [92], while variants in HLA-C are linked with painful conditions including rheumatoid arthritis [93], psoriatic arthritis [94], and endometriosis [95]. Although not extensively studied in the context of pain, increased signaling of MHC-I is implicated in an animal model of cancer-induced bone pain through increased neuronal apoptosis, and siRNA knockdown of B2M attenuates this hyperalgesia [96]. Again, cellular apoptosis can lead to DRG sensitization due to release of intracellular components, such as ATP and S100 proteins, and could be responsible for the production of prolonged PASC-induced musculoskeletal pain.
CD8 T Cells
As seen with CD4 T cells, there is a decrease in the number of circulating CD8 T cells following COVID-19 infection, with further decreases reported as severity of symptoms increase [47,48,49]. CD8 T cells are part of the adaptive immune system and can be classified into a cytotoxic or regulatory phenotype [97]. CD8 T cells recognize antigens displayed by MHC-I and cytotoxic CD8 T cells are programmed to destroy virally infected cells [90]. In the context of chronic pain, changes in circulating levels of CD8 T cells are not routinely found; however, a higher CD4/CD8 ratio has been demonstrated in those with chronic headache [98], another common pain complaint in PASC patients [9]. In animal models of pain, CD8 T cells have exhibited both pain-promoting and pain-resolving effects. In a model of chemotherapy-induced peripheral neuropathy, intrathecal administration of CD8 T cells increases pain hypersensitivity in mice [99]. However, in mice lacking T cells, the resolution of hypersensitivity produced by chemotherapy-induced neuropathies is delayed, and reconstitution of these animals with CD8 T cells restores the alleviation of pain, suggesting CD8 T cells have pain-resolving effects [100]. In fact, CD8 T cells were shown to promote the resolution of cisplatin-induced neuropathies by stimulating the release of IL-10 from macrophages [101]. Similarly in an animal model of arthritic pain, CD8 T cell depletion enhances pain hypersensitivity [102], and CD8 T cells play a pivotal role in both endogenous and exogenous opioid induced-analgesia [102, 103]. This data suggests the loss of circulating CD8 T cells could play a role in the development of musculoskeletal pain in individuals with PASC due to a loss of pain-resolving and analgesic mechanisms.
Our interactome analysis revealed that ligands from CD8 T cells could bind to receptors on DRGs to activate pathways causing inflammation and the recruitment of immune cells, including neutrophils (Fig. 1). Activation of inflammatory pathways will cause an increase in the number of immune cells, cytokines, and chemokines that if left unresolved can cause sensitization of nociceptors and DRGs leading to hypersensitivity and prolonged pain [86, 104]. Our interactome also displayed similar biological processes and molecular functions for pathways activated by CD8 effector and memory T cells, and CD8 T cells showed upregulation of ligand genes HLA-C and S100A8/9 similar to other immune cells in our analysis (Fig. 2). Of note, one of the top hits for CD8 effector T cells was the ligand gene HMGB1 (Fig. 2). The protein HMGB1 is an alarmin that can be released by immune cells; plays a role in mediating immune cell migration, proliferation, and differentiation; and is implicated in the production of chronic pain through neuroinflammation [54]. In rodents, intrathecal, sciatic nerve, and intraplanar administration of HMGB1 produces mechanical hypersensitivity [105,106,107]. Furthermore, increases in HMGB1 are found in nociceptors, DRG, and spinal cord following induction of neuropathic pain [108,109,110], and pharmacological blockade of HMGB1 alleviates neuropathic pain [110,111,112,113]. In individuals with rheumatoid arthritis, increases in HMGB1 are found in the synovial fluid of joints, suggesting a role in the pathophysiology of this painful disease [114,115,116]. A top hit for CD8 memory T cells was the ligand gene FLT3LG that encodes for the cytokine FMS-like tyrosine kinase 3 ligand (FLT3) which has recently been implicated in the production of pain (Fig. 2). In mice, intrathecal injection of FLT3 alone produces paw hypersensitivity, genetic knockdown and pharmacological inhibition of FLT3 protects against and alleviates neuropathic and post-incisional pain, and FLT3 produces sensitization of cultured DRG neurons [117, 118]. Thus, CD8 T cells could also produce PASC-induced musculoskeletal pain through induction of prolonged neuroinflammation through mechanisms involving HMGB1 and FLT3LG.
B Cells
B cells are part of the adaptive immune system and produce antibodies to protect the host against specific pathogens [119]. Upon activation, naïve B cells can differentiate into memory B cells or antibody producing plasma cells which are increased in individuals with COVID-19 [49, 119]. Although not studied as in depth as monocytes and T cells, there is emerging evidence illustrating the potential role of B cells in the production of pain. Pharmacological depletion of B cells in individuals with rheumatoid arthritis results in improvement of rheumatological symptoms, which include pain [120]. In an animal model of complex regional pain syndrome, B cell-deficient mice and depletion of B cells results in prevention or alleviation of mechanical hypersensitivity [121]. However, reducing B cells in mice does not protect against neuropathic or postoperative incisional pain suggesting B cells may play a role in the etiology of only specific pain producing conditions [121, 122].
The interactome analysis demonstrates that as a whole, B cells activate pathways associated with MHC-I and type I interferon (IFN) signaling and show increases in the ligand genes S100A8/9 (Figs. 1 and 2), which were common across cell types. IFNs are a class of cytokines that play a role in interfering with virus replication and are classified as either type I, type II, or type III [123]. The major classes of type I IFNs are IFNα and IFNβ, which have recently been shown to act directly on nociceptors. In animals, virally induced pain is driven by a pathway mediated by type I IFN-stimulated increases in indoleamine-2,3-dioxygenase [124, 125], and intraplantar administration of type I IFNs alone produces mechanical hypersensitivity [126]. Type I IFNs bind and sensitize DRG neurons through the phosphorylation of eIF4E [126]. Our interactome analysis also revealed that ligands from different B cells activate unique biological pathways. Ligands from naïve B cells activate pathways involving neutrophil activation while memory B cells initiate pathways mediating cellular apoptosis (Fig. 1). One of the top interactions for all B cells involved the ligand gene RPS19 which encodes a ribosomal protein that binds to the complement receptor C5AR1 and is responsible for immune cell activation and monocyte recruitment [127, 128] (Fig. 2). Activation of C5AR1 mediates the production of pain in several animal models including neuropathic, complex regional pain syndrome, and postsurgical pain models through its ability to sensitize DRG nociceptors [129,130,131,132]. Thus, B cells could produce prolonged PASC-induced musculoskeletal pain through activation of MHC-I, type I IFNs, and complement system signaling.
Natural Killer Cells
Natural killer (NK) cells are a member of the innate immune system that release cytokines and possess cytotoxic capabilities tasked with killing virally infected and tumor cells [133]. It has been reported that circulating NK cells are decreased in individuals with COVID-19 [49]. Little attention has been given to NK cells in terms of their role in producing persistent pain. Levels of circulating NK cells have been measured in individuals with fibromyalgia, neuropathic pain, complex regional pain syndrome, and low back pain without a clear consensus on alterations in NK cell levels, as some articles show slight decreases in the NK cell population and activity while others show no change [134,135,136,137,138,139]. However, a recent assessment in individuals with neuropathic pain demonstrated that decreases in the frequency of NK cells in the cerebrospinal fluid is correlated with increased mechanical pain sensitivity assessed via quantitative sensory testing, suggesting a protective role of NK cells in neuropathic pain [139]. Thus, decreased circulating levels of NK cells in individuals with COVID-19 could be involved with the generation of PASC-induced musculoskeletal pain. Our interactome analysis revealed that ligands from NK cells activate pathways involved in T cell and neutrophil chemotaxis and several of the top ligand genes from NK cells are involved in MHC-I signaling including HLA-A,B,C (Figs. 1 and 2). Thus, NK cells could be producing PASC-induced musculoskeletal pain through T cell activation and MHC-I-induced cellular apoptosis.
Overview, Limitations, and Future Directions
Overall, results from our interactome analysis revealed the enrichment of pathways including immune cell activation and chemotaxis, response to cytokines, complement system activation, and type I IFN signaling that could be driving the production of musculoskeletal pain in individuals with PASC. The most consistent finding across all immune cell subtypes that were analyzed was increases in the genes encoding the alarmins S100A8/9 and ligands involved in the activation of MHC-I; thus, they serve as great targets for future research in the mechanisms producing PASC-induced musculoskeletal pain. The interactome also revealed similarities across adaptive immune cells (T and B cells) in their ligand gene molecular function GO terms. First, adaptive immune cells showed activation of pathways involving arachidonic acid binding which is driven by the upregulation of the alarmins S100A8/9 [140] (Fig. 1). Arachidonic acid is a fatty acid that is a precursor to the synthesis of many eicosanoids including prostaglandin, which is implicated in the production of pain [141]. Increases in prostaglandins are found in the DRGs of rodents following induction of neuropathic, low back, and post-incisional pain [142,143,144], and cultured DRGs produce prostaglandin upon stimulation with pro-inflammatory cytokines [145]. Prostaglandin signaling increases nociceptor excitability and expression of several ion channels and receptors including sodium channels, calcium channels, purinergic receptors, and TRPV1 receptors, to drive peripheral sensitization leading to the production of persistent pain [141]. Secondly, the adaptive immune cells showed activation of receptor for advanced glycation end products (RAGE), which is also driven by the upregulation of S100A8/9 [54] (Fig. 1). RAGE can bind with several ligands including S100 proteins and HMGB1 [146]. Activation of RAGE by S100A8/9 and HMGB1 produces pro-inflammatory signaling and immune cell migration [147, 148] which could lead to a sensitization of DRG neurons to produce long-term musculoskeletal pain associated with PASC.
There are several limitations to this work. First, we utilized single-cell RNA sequencing data sets from individuals who were recently diagnosed with COVID-19. While our analysis can be useful about making predictions about PASC-induced musculoskeletal pain mechanisms, future research should focus on collecting tissues from individuals with PASC to further determine molecular mechanisms underlying symptomology. Secondly, as only 30% of individuals with COVID-19 go on to develop PASC, the majority of individuals included in the data sets used in this analysis likely did not develop PASC. If possible, future work should follow up with the individuals whose PBMCs were collected acutely after COVID-19 diagnosis so that further comparisons can be made between individuals that did and did not develop PASC. Lastly, due to the heterogeneity of the patient characteristics used in each study, we were unable to draw any conclusions regarding potential impact of sex or disease severity on the ligand-receptor interactome. Future work aimed at underpinning the molecular mechanisms of PASC associated pain should power their studies to be able to explore for sex differences as the immune system’s mechanistic role in producing pain has been demonstrated to be sex dimorphic [149,150,151,152,153,154].
Studies on individuals with PASC have consistently shown pain as a major feature of the disorder [8, 9]. Our work suggests interactions between circulating immune cells and nociceptors could drive the production of PASC-induced pain. We recommend targeted prospective studies on individuals with PASC with specific pain symptoms, such as musculoskeletal pain, to examine changes in transcriptomes of the immune cell types highlighted here to better understand how these cells are altered in this patient population. Integrating that data with the interactome platform described here can help to hone in targets that might have the greatest value for alleviation of pain in PASC patients. These types of prospective experiments could also potentially confirm targets described here in patients that are in a later stage of the disease. Such targets would likely have the greatest value for moving ahead into clinical trials for patients suffering from persistent pain post-COVID-19.
Conclusion
Our interactome analysis revealed that PBMC populations express several ligands that are upregulated in COVID-19 and could bind to receptors on DRG neurons to activate several pro-nociceptive pathways, including immune cell activation and migration. The ligands most consistently upregulated across monocyte and lymphocyte cell types involved the alarmins S100A8/9 and MHC-I signaling. We hope that this interactome analysis will provide data for the generation of future hypotheses and research regarding the mechanisms underlying PASC-induced musculoskeletal pain.
References
Menges D, Ballouz T, Anagnostopoulos A, Aschmann HE, Domenghino A, Fehr JS, et al. Burden of post-COVID-19 syndrome and implications for healthcare service planning: a population-based cohort study. PLoS One. 2021;16(7):e0254523.
Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, Stevens JS, et al. Post-acute COVID-19 syndrome. Nat Med. 2021;27(4):601–15. https://doi.org/10.1038/s41591-021-01283-z.
Nguyen NN, Hoang VT, Dao TL, Dudouet P, Eldin C, Gautret P. Clinical patterns of somatic symptoms in patients suffering from post-acute long COVID: a systematic review. Eur J Clin Microbiol Infect Dis. 2022;41(4):515–45. https://doi.org/10.1007/s10096-022-04417-4.
Xie Y, Xu E, Bowe B, Al-Aly Z. Long-term cardiovascular outcomes of COVID-19. Nat Med. 2022;28(3):583–90. https://doi.org/10.1038/s41591-022-01689-3.
Moreno-Pérez O, Merino E, Leon-Ramirez J-M, Andres M, Ramos JM, Arenas-Jiménez J, et al. Post-acute COVID-19 syndrome. Incidence and risk factors: a Mediterranean cohort study. J Infect. 2021;82(3):378–83. https://doi.org/10.1016/j.jinf.2021.01.004.
Meringer H, Mehandru S. Gastrointestinal post-acute COVID-19 syndrome. Nat Rev Gastroenterol Hepatol. 2022;19(6):345–6. https://doi.org/10.1038/s41575-022-00611-z.
Xie Y, Al-Aly Z. Risks and burdens of incident diabetes in long COVID: a cohort study. Lancet Diabetes Endocrinol. 2022;10(5):311–21. https://doi.org/10.1016/s2213-8587(22)00044-4.
Haider S, Janowski AJ, Lesnak JB, Hayashi K, Dailey DL, Chimenti R, et al. A comparison of pain, fatigue, and function between post-COVID-19 condition, fibromyalgia, and chronic fatigue syndrome: a survey study. Pain. 2023;164(2):385–401. https://doi.org/10.1097/j.pain.0000000000002711.
Zhang H, Zang C, Xu Z, Zhang Y, Xu J, Bian J, et al. Data-driven identification of post-acute SARS-CoV-2 infection subphenotypes. Nat Med. 2023;29(1):226–35. https://doi.org/10.1038/s41591-022-02116-3.
Gong WY, Abdelhamid RE, Carvalho CS, Sluka KA. Resident macrophages in muscle contribute to development of hyperalgesia in a mouse model of noninflammatory muscle pain. J Pain. 2016;17(10):1081–94. https://doi.org/10.1016/j.jpain.2016.06.010.
Gregory NS, Brito RG, Fusaro MC, Sluka KA. ASIC3 is required for development of fatigue-induced hyperalgesia. Mol Neurobiol. 2016;53(2):1020–30. https://doi.org/10.1007/s12035-014-9055-4.
de Azambuja G, Jorge CO, Gomes BB, Lourenço HR, Simabuco FM, Oliveira-Fusaro MCG. Regular swimming exercise prevented the acute and persistent mechanical muscle hyperalgesia by modulation of macrophages phenotypes and inflammatory cytokines via PPARγ receptors. Brain Behav Immun. 2021;95:462–76. https://doi.org/10.1016/j.bbi.2021.05.002.
Hayashi K, Lesnak JB, Plumb AN, Rasmussen LA, Sluka KA. P2X7-NLRP3-Caspase-1 signaling mediates activity-induced muscle pain in male but not female mice. Pain. 2023. https://doi.org/10.1097/j.pain.0000000000002887.
Laumet G, Ma J, Robison AJ, Kumari S, Heijnen CJ, Kavelaars A. T Cells as an emerging target for chronic pain therapy. Front Mol Neurosci. 2019;12:216. https://doi.org/10.3389/fnmol.2019.00216.
Yap HY, Tee SZ, Wong MM, Chow SK, Peh SC, Teow SY. Pathogenic role of immune cells in rheumatoid arthritis: implications in clinical treatment and biomarker development. Cells. 2018;7(10). https://doi.org/10.3390/cells7100161.
Firestein GS, McInnes IB. Immunopathogenesis of rheumatoid arthritis. Immunity. 2017;46(2):183–96. https://doi.org/10.1016/j.immuni.2017.02.006.
Zhu W, Zhang X, Jiang Y, Liu X, Huang L, Wei Q, et al. Alterations in peripheral T cell and B cell subsets in patients with osteoarthritis. Clin Rheumatol. 2020;39(2):523–32. https://doi.org/10.1007/s10067-019-04768-y.
Kapoor M, Martel-Pelletier J, Lajeunesse D, Pelletier JP, Fahmi H. Role of proinflammatory cytokines in the pathophysiology of osteoarthritis. Nat Rev Rheumatol. 2011;7(1):33–42. https://doi.org/10.1038/nrrheum.2010.196.
Teodorczyk-Injeyan JA, McGregor M, Triano JJ, Injeyan SH. Elevated production of nociceptive CC chemokines and sE-selectin in patients with low back pain and the effects of spinal manipulation: a nonrandomized clinical trial. Clin J Pain. 2018;34(1):68–75. https://doi.org/10.1097/ajp.0000000000000507.
Merriwether EN, Agalave NM, Dailey DL, Rakel BA, Kolker SJ, Lenert ME, et al. IL-5 mediates monocyte phenotype and pain outcomes in fibromyalgia. Pain. 2021;162(5):1468–82. https://doi.org/10.1097/j.pain.0000000000002089.
Uçeyler N, Häuser W, Sommer C. Systematic review with meta-analysis: cytokines in fibromyalgia syndrome. BMC Musculoskelet Disord. 2011;12:245. https://doi.org/10.1186/1471-2474-12-245.
Bäckryd E, Tanum L, Lind AL, Larsson A, Gordh T. Evidence of both systemic inflammation and neuroinflammation in fibromyalgia patients, as assessed by a multiplex protein panel applied to the cerebrospinal fluid and to plasma. J Pain Res. 2017;10:515–25. https://doi.org/10.2147/jpr.S128508.
Imamura M, Targino RA, Hsing WT, Imamura S, Azevedo RS, Boas LS, et al. Concentration of cytokines in patients with osteoarthritis of the knee and fibromyalgia. Clin Interv Aging. 2014;9:939–44. https://doi.org/10.2147/cia.S60330.
Ji RR, Chamessian A, Zhang YQ. Pain regulation by non-neuronal cells and inflammation. Science (New York, NY). 2016;354(6312):572–7. https://doi.org/10.1126/science.aaf8924.
Wangzhou A, Paige C, Neerukonda SV, Naik DK, Kume M, David ET, et al. A ligand-receptor interactome platform for discovery of pain mechanisms and therapeutic targets. Sci Signal. 2021;14(674). https://doi.org/10.1126/scisignal.abe1648.
Arunachalam PS, Wimmers F, Mok CKP, Perera R, Scott M, Hagan T, et al. Systems biological assessment of immunity to mild versus severe COVID-19 infection in humans. Science (New York, NY). 2020;369(6508):1210–20. https://doi.org/10.1126/science.abc6261.
Krämer B, Knoll R, Bonaguro L, ToVinh M, Raabe J, Astaburuaga-García R, et al. Early IFN-α signatures and persistent dysfunction are distinguishing features of NK cells in severe COVID-19. Immunity. 2021;54(11):2650-69.e14. https://doi.org/10.1016/j.immuni.2021.09.002.
Qi F, Zhang W, Huang J, Fu L, Zhao J. Single-cell RNA sequencing analysis of the immunometabolic rewiring and immunopathogenesis of coronavirus disease 2019. Front Immunol. 2021;12:651656. https://doi.org/10.3389/fimmu.2021.651656.
Silvin A, Chapuis N, Dunsmore G, Goubet AG, Dubuisson A, Derosa L, et al. Elevated calprotectin and abnormal myeloid cell subsets discriminate severe from mild COVID-19. Cell. 2020;182(6):1401-18.e18. https://doi.org/10.1016/j.cell.2020.08.002.
Xu G, Qi F, Li H, Yang Q, Wang H, Wang X, et al. The differential immune responses to COVID-19 in peripheral and lung revealed by single-cell RNA sequencing. Cell Discov. 2020;6:73. https://doi.org/10.1038/s41421-020-00225-2.
Tavares-Ferreira D, Shiers S, Ray PR, Wangzhou A, Jeevakumar V, Sankaranarayanan I, et al. Spatial transcriptomics of dorsal root ganglia identifies molecular signatures of human nociceptors. Sci Transl Med. 2022;14(632):eabj8186. https://doi.org/10.1126/scitranslmed.abj8186.
McKemy DD, Neuhausser WM, Julius D. Identification of a cold receptor reveals a general role for TRP channels in thermosensation. Nature. 2002;416(6876):52–8. https://doi.org/10.1038/nature719.
Chen EY, Tan CM, Kou Y, Duan Q, Wang Z, Meirelles GV, et al. Enrichr: interactive and collaborative HTML5 gene list enrichment analysis tool. BMC Bioinformatics. 2013;14(1):128. https://doi.org/10.1186/1471-2105-14-128.
Kuleshov MV, Jones MR, Rouillard AD, Fernandez NF, Duan Q, Wang Z, et al. Enrichr: a comprehensive gene set enrichment analysis web server 2016 update. Nucleic Acids Res. 2016;44(W1):W90–7. https://doi.org/10.1093/nar/gkw377.
Thomas PD, Ebert D, Muruganujan A, Mushayahama T, Albou LP, Mi H. PANTHER: making genome-scale phylogenetics accessible to all. Protein Sci. 2022;31(1):8–22. https://doi.org/10.1002/pro.4218.
Coulthard LR, Geiler J, Mathews RJ, Church LD, Dickie LJ, Cooper DL, et al. Differential effects of infliximab on absolute circulating blood leucocyte counts of innate immune cells in early and late rheumatoid arthritis patients. Clin Exp Immunol. 2012;170(1):36–46. https://doi.org/10.1111/j.1365-2249.2012.04626.x.
Lioté F, Boval-Boizard B, Weill D, Kuntz D, Wautier JL. Blood monocyte activation in rheumatoid arthritis: increased monocyte adhesiveness, integrin expression, and cytokine release. Clin Exp Immunol. 1996;106(1):13–9. https://doi.org/10.1046/j.1365-2249.1996.d01-820.x.
Mulherin D, Fitzgerald O, Bresnihan B. Synovial tissue macrophage populations and articular damage in rheumatoid arthritis. Arthritis Rheum. 1996;39(1):115–24. https://doi.org/10.1002/art.1780390116.
Torsteinsdóttir I, Arvidson NG, Hällgren R, Håkansson L. Monocyte activation in rheumatoid arthritis (RA): increased integrin, Fc gamma and complement receptor expression and the effect of glucocorticoids. Clin Exp Immunol. 1999;115(3):554–60. https://doi.org/10.1046/j.1365-2249.1999.00817.x.
Gómez-Aristizábal A, Gandhi R, Mahomed NN, Marshall KW, Viswanathan S. Synovial fluid monocyte/macrophage subsets and their correlation to patient-reported outcomes in osteoarthritic patients: a cohort study. Arthritis Res Ther. 2019;21(1):26. https://doi.org/10.1186/s13075-018-1798-2.
Loukov D, Karampatos S, Maly MR, Bowdish DME. Monocyte activation is elevated in women with knee-osteoarthritis and associated with inflammation, BMI and pain. Osteoarthr Cartil. 2018;26(2):255–63. https://doi.org/10.1016/j.joca.2017.10.018.
Haubruck P, Pinto MM, Moradi B, Little CB, Gentek R. Monocytes, macrophages, and their potential niches in synovial joints - therapeutic targets in post-traumatic osteoarthritis? Front Immunol. 2021;12:763702. https://doi.org/10.3389/fimmu.2021.763702.
Taylor AG, Fischer-White TG, Anderson JG, Adelstein KE, Murugesan M, Lewis JE, et al. Stress, inflammation and pain: a potential role for monocytes in fibromyalgia-related symptom severity. Stress Health. 2016;32(5):503–13. https://doi.org/10.1002/smi.2648.
Li Y, Liu J, Liu ZZ, Duan DP. Inflammation in low back pain may be detected from the peripheral blood: suggestions for biomarker. Biosci Rep. 2016;36(4). https://doi.org/10.1042/bsr20160187.
Wilk AJ, Rustagi A, Zhao NQ, Roque J, Martínez-Colón GJ, McKechnie JL, et al. A single-cell atlas of the peripheral immune response in patients with severe COVID-19. Nat Med. 2020;26(7):1070–6. https://doi.org/10.1038/s41591-020-0944-y.
Szabo PA, Dogra P, Gray JI, Wells SB, Connors TJ, Weisberg SP, et al. Longitudinal profiling of respiratory and systemic immune responses reveals myeloid cell-driven lung inflammation in severe COVID-19. Immunity. 2021;54(4):797-814.e6. https://doi.org/10.1016/j.immuni.2021.03.005.
Wen W, Su W, Tang H, Le W, Zhang X, Zheng Y, et al. Immune cell profiling of COVID-19 patients in the recovery stage by single-cell sequencing. Cell Discov. 2020;6:31. https://doi.org/10.1038/s41421-020-0168-9.
Hasan MZ, Islam S, Matsumoto K, Kawai T. Meta-analysis of single-cell RNA-seq data reveals phenotypic switching of immune cells in severe COVID-19 patients. Comput Biol Med. 2021;137:104792. https://doi.org/10.1016/j.compbiomed.2021.104792.
Liu W, Jia J, Dai Y, Chen W, Pei G, Yan Q, et al. Delineating COVID-19 immunological features using single-cell RNA sequencing. Innovation. 2022;3(5):100289. https://doi.org/10.1016/j.xinn.2022.100289.
Carreira EU, Carregaro V, Teixeira MM, Moriconi A, Aramini A, Verri WA Jr, et al. Neutrophils recruited by CXCR1/2 signalling mediate post-incisional pain. Eur J Pain. 2013;17(5):654–63. https://doi.org/10.1002/j.1532-2149.2012.00240.x.
Cunha TM, Verri WA Jr, Schivo IR, Napimoga MH, Parada CA, Poole S, et al. Crucial role of neutrophils in the development of mechanical inflammatory hypernociception. J Leukoc Biol. 2008;83(4):824–32. https://doi.org/10.1189/jlb.0907654.
Parisien M, Lima LV, Dagostino C, El-Hachem N, Drury GL, Grant AV, et al. Acute inflammatory response via neutrophil activation protects against the development of chronic pain. Sci Transl Med. 2022;14(644):eabj9954. https://doi.org/10.1126/scitranslmed.abj9954.
Wang S, Song R, Wang Z, Jing Z, Wang S, Ma J. S100A8/A9 in inflammation. Frontiers in Immunology. 2018;9. https://doi.org/10.3389/fimmu.2018.01298.
Bertheloot D, Latz E. HMGB1, IL-1α, IL-33 and S100 proteins: dual-function alarmins. Cell Mol Immunol. 2017;14(1):43–64. https://doi.org/10.1038/cmi.2016.34.
Zheng J, Wang J, Liu H, Chen F, Wang H, Chen S, et al. Alarmins S100A8/A9 promote intervertebral disc degeneration and inflammation-related pain in a rat model through toll-like receptor-4 and activation of the NF-κB signaling pathway. Osteoarthr Cartilage. 2022;30(7):998–1011. https://doi.org/10.1016/j.joca.2022.03.011.
van Lent PL, Blom AB, Schelbergen RF, Slöetjes A, Lafeber FP, Lems WF, et al. Active involvement of alarmins S100A8 and S100A9 in the regulation of synovial activation and joint destruction during mouse and human osteoarthritis. Arthritis Rheum. 2012;64(5):1466–76. https://doi.org/10.1002/art.34315.
van Lent PL, Grevers L, Blom AB, Sloetjes A, Mort JS, Vogl T, et al. Myeloid-related proteins S100A8/S100A9 regulate joint inflammation and cartilage destruction during antigen-induced arthritis. Ann Rheum Dis. 2008;67(12):1750–8. https://doi.org/10.1136/ard.2007.077800.
Miller RE, Belmadani A, Ishihara S, Tran PB, Ren D, Miller RJ, et al. Damage-associated molecular patterns generated in osteoarthritis directly excite murine nociceptive neurons through Toll-like receptor 4. Arthritis Rheumatol (Hoboken, NJ). 2015;67(11):2933–43. https://doi.org/10.1002/art.39291.
Chen M, Liu H, Li Z, Ming AL, Chen H. Mechanism of PKM2 affecting cancer immunity and metabolism in Tumor Microenvironment. J Cancer. 2021;12(12):3566–74. https://doi.org/10.7150/jca.54430.
Palsson-McDermott EM, Dyck L, Zasłona Z, Menon D, McGettrick AF, Mills KHG, et al. Pyruvate kinase M2 is required for the expression of the immune checkpoint PD-L1 in immune cells and tumors. Front Immunol. 2017;8:1300. https://doi.org/10.3389/fimmu.2017.01300.
Chizh BA, Illes P. P2X receptors and nociception. Pharmacol Rev. 2001;53(4):553–68.
Audrito V, Messana VG, Deaglio S. NAMPT and NAPRT: two metabolic enzymes with key roles in inflammation. Frontiers in Oncology. 2020;10. https://doi.org/10.3389/fonc.2020.00358.
Huffaker TB, Ekiz HA, Barba C, Lee S-H, Runtsch MC, Nelson MC, et al. A Stat1 bound enhancer promotes Nampt expression and function within tumor associated macrophages. Nat Commun. 2021;12(1):2620. https://doi.org/10.1038/s41467-021-22923-5.
Ray PR, Shiers S, Caruso JP, Tavares-Ferreira D, Sankaranarayanan I, Uhelski ML, et al. RNA profiling of human dorsal root ganglia reveals sex-differences in mechanisms promoting neuropathic pain. Brain : a journal of neurology. 2022. https://doi.org/10.1093/brain/awac266.
Zhang LQ, Heruth DP, Ye SQ. Nicotinamide phosphoribosyltransferase in human diseases. J Bioanal Biomed. 2011;3:13–25. https://doi.org/10.4172/1948-593x.1000038.
Jian J, Konopka J, Liu C. Insights into the role of progranulin in immunity, infection, and inflammation. J Leukoc Biol. 2013;93(2):199–208. https://doi.org/10.1189/jlb.0812429.
Sun R, Wang D, Song Y, Li Q, Su P, Pang Y. Granulin as an important immune molecule involved in lamprey tissue repair and regeneration by promoting cell proliferation and migration. Cell Mol Biol Lett. 2022;27(1):64. https://doi.org/10.1186/s11658-022-00360-6.
Lim HY, Albuquerque B, Häussler A, Myrczek T, Ding A, Tegeder I. Progranulin contributes to endogenous mechanisms of pain defense after nerve injury in mice. J Cell Mol Med. 2012;16(4):708–21. https://doi.org/10.1111/j.1582-4934.2011.01350.x.
Tang W, Lu Y, Tian QY, Zhang Y, Guo FJ, Liu GY, et al. The growth factor progranulin binds to TNF receptors and is therapeutic against inflammatory arthritis in mice. Science (New York, NY). 2011;332(6028):478–84. https://doi.org/10.1126/science.1199214.
Aschman T, Wyler E, Baum O, Hentschel A, Legler F, Preusse C, et al. Post-COVID syndrome is associated with capillary alterations, macrophage infiltration and distinct transcriptomic signatures in skeletal muscles. medRxiv. 2023:2023.02.15.23285584. https://doi.org/10.1101/2023.02.15.23285584.
Zhou Y, Fu B, Zheng X, Wang D, Zhao C, Qi Y, et al. Pathogenic T-cells and inflammatory monocytes incite inflammatory storms in severe COVID-19 patients. Natl Sci Rev. 2020;7(6):998–1002. https://doi.org/10.1093/nsr/nwaa041.
Gil-Etayo FJ, Suàrez-Fernández P, Cabrera-Marante O, Arroyo D, Garcinuño S, Naranjo L, et al. T-Helper cell subset response is a determining factor in COVID-19 progression. Front Cell Infect Microbiol. 2021;11:624483. https://doi.org/10.3389/fcimb.2021.624483.
Neidleman J, Luo X, Frouard J, Xie G, Gill G, Stein ES, et al. SARS-CoV-2-specific T cells exhibit phenotypic features of helper function, lack of terminal differentiation, and high proliferation potential. Cell Rep Med. 2020;1(6):100081. https://doi.org/10.1016/j.xcrm.2020.100081.
Roncati L, Nasillo V, Lusenti B, Riva G. Signals of T(h)2 immune response from COVID-19 patients requiring intensive care. Ann Hematol. 2020;99(6):1419–20. https://doi.org/10.1007/s00277-020-04066-7.
Hu P, McLachlan EM. Macrophage and lymphocyte invasion of dorsal root ganglia after peripheral nerve lesions in the rat. Neuroscience. 2002;112(1):23–38. https://doi.org/10.1016/s0306-4522(02)00065-9.
McLachlan EM, Hu P. Inflammation in dorsal root ganglia after peripheral nerve injury: effects of the sympathetic innervation. Auton Neurosci. 2014;182:108–17. https://doi.org/10.1016/j.autneu.2013.12.009.
Du B, Ding YQ, Xiao X, Ren HY, Su BY, Qi JG. CD4+ αβ T cell infiltration into the leptomeninges of lumbar dorsal roots contributes to the transition from acute to chronic mechanical allodynia after adult rat tibial nerve injuries. J Neuroinflammation. 2018;15(1):81. https://doi.org/10.1186/s12974-018-1115-7.
Kobayashi Y, Kiguchi N, Fukazawa Y, Saika F, Maeda T, Kishioka S. Macrophage-T cell interactions mediate neuropathic pain through the glucocorticoid-induced tumor necrosis factor ligand system. J Biol Chem. 2015;290(20):12603–13. https://doi.org/10.1074/jbc.M115.636506.
Moalem G, Xu K, Yu L. T lymphocytes play a role in neuropathic pain following peripheral nerve injury in rats. Neuroscience. 2004;129(3):767–77. https://doi.org/10.1016/j.neuroscience.2004.08.035.
van Loosdregt J, Rossetti M, Spreafico R, Moshref M, Olmer M, Williams GW, et al. Increased autophagy in CD4(+) T cells of rheumatoid arthritis patients results in T-cell hyperactivation and apoptosis resistance. Eur J Immunol. 2016;46(12):2862–70. https://doi.org/10.1002/eji.201646375.
Chemin K, Gerstner C, Malmström V. Effector functions of CD4+ T cells at the site of local autoimmune inflammation—lessons from rheumatoid arthritis. Frontiers in Immunology. 2019;10. https://doi.org/10.3389/fimmu.2019.00353.
Mellado M, Martínez-Muñoz L, Cascio G, Lucas P, Pablos JL, Rodríguez-Frade JM. T cell migration in rheumatoid arthritis. Front Immunol. 2015;6:384. https://doi.org/10.3389/fimmu.2015.00384.
Penatti A, Facciotti F, De Matteis R, Larghi P, Paroni M, Murgo A, et al. Differences in serum and synovial CD4+ T cells and cytokine profiles to stratify patients with inflammatory osteoarthritis and rheumatoid arthritis. Arthritis Res Ther. 2017;19(1):103. https://doi.org/10.1186/s13075-017-1305-1.
Rosshirt N, Trauth R, Platzer H, Tripel E, Nees TA, Lorenz H-M, et al. Proinflammatory T cell polarization is already present in patients with early knee osteoarthritis. Arthritis Res Ther. 2021;23(1):37. https://doi.org/10.1186/s13075-020-02410-w.
Li YS, Luo W, Zhu SA, Lei GH. T cells in osteoarthritis: alterations and beyond. Front Immunol. 2017;8:356. https://doi.org/10.3389/fimmu.2017.00356.
Zhang JM, An J. Cytokines, inflammation, and pain. Int Anesthesiol Clin. 2007;45(2):27–37. https://doi.org/10.1097/AIA.0b013e318034194e.
Kalpachidou T, Riehl L, Schöpf CL, Ucar B, Kress M. Proinflammatory cytokines and their receptors as druggable targets to alleviate pathological pain. Pain. 2022;163(S1):S79–98. https://doi.org/10.1097/j.pain.0000000000002737.
Fritzinger DC, Benjamin DE. The complement system in neuropathic and postoperative pain. Open Pain J. 2016;9:26–37. https://doi.org/10.2174/1876386301609010026.
Warwick CA, Keyes AL, Woodruff TM, Usachev YM. The complement cascade in the regulation of neuroinflammation, nociceptive sensitization, and pain. J Biol Chem. 2021;297(3):101085. https://doi.org/10.1016/j.jbc.2021.101085.
Pishesha N, Harmand TJ, Ploegh HL. A guide to antigen processing and presentation. Nat Rev Immunol. 2022. https://doi.org/10.1038/s41577-022-00707-2.
Hewitt EW. The MHC class I antigen presentation pathway: strategies for viral immune evasion. Immunology. 2003;110(2):163–9. https://doi.org/10.1046/j.1365-2567.2003.01738.x.
Kallianpur AR, Jia P, Ellis RJ, Zhao Z, Bloss C, Wen W, et al. Genetic variation in iron metabolism is associated with neuropathic pain and pain severity in HIV-infected patients on antiretroviral therapy. PloS One. 2014;9(8):e103123. https://doi.org/10.1371/journal.pone.0103123.
Siegel RJ, Bridges SL Jr, Ahmed S. HLA-C: an accomplice in rheumatic diseases. ACR Open Rheumatol. 2019;1(9):571–9. https://doi.org/10.1002/acr2.11065.
Queiro R, Gonzalez S, López-Larrea C, Alperi M, Sarasqueta C, Riestra JL, et al. HLA-C locus alleles may modulate the clinical expression of psoriatic arthritis. Arthritis Res Ther. 2006;8(6):R185. https://doi.org/10.1186/ar2097.
Chou Y-C, Chen C-H, Chen M-J, Chang C-W, Chen P-H, Yu M-H, et al. Killer cell immunoglobulin-like receptors (KIR) and human leukocyte antigen-C (HLA-C) allorecognition patterns in women with endometriosis. Sci Rep. 2020;10(1):4897. https://doi.org/10.1038/s41598-020-61702-y.
Fu Q, Shi D, Zhou Y, Zheng H, Xiang H, Tian X, et al. MHC-I promotes apoptosis of GABAergic interneurons in the spinal dorsal horn and contributes to cancer induced bone pain. Exp Neurol. 2016;286:12–20. https://doi.org/10.1016/j.expneurol.2016.09.002.
Mousset CM, Hobo W, Woestenenk R, Preijers F, Dolstra H, van der Waart AB. Comprehensive phenotyping of T cells using flow cytometry. Cytometry A. 2019;95(6):647–54. https://doi.org/10.1002/cyto.a.23724.
Gilman-Sachs A, Robbins L, Baum L. Flow cytometric analysis of lymphocyte subsets in peripheral blood of chronic headache patients. Headache. 1989;29(5):290–4. https://doi.org/10.1111/j.1526-4610.1989.hed2905290.x.
Liu XJ, Zhang Y, Liu T, Xu ZZ, Park CK, Berta T, et al. Nociceptive neurons regulate innate and adaptive immunity and neuropathic pain through MyD88 adapter. Cell Res. 2014;24(11):1374–7. https://doi.org/10.1038/cr.2014.106.
Krukowski K, Eijkelkamp N, Laumet G, Hack CE, Li Y, Dougherty PM, et al. CD8+ T cells and endogenous IL-10 are required for resolution of chemotherapy-induced neuropathic pain. J Neurosci. 2016;36(43):11074–83. https://doi.org/10.1523/jneurosci.3708-15.2016.
Singh SK, Krukowski K, Laumet GO, Weis D, Alexander JF, Heijnen CJ, et al. CD8+ T cell–derived IL-13 increases macrophage IL-10 to resolve neuropathic pain. JCI Insight. 2022;7(5). https://doi.org/10.1172/jci.insight.154194.
Baddack-Werncke U, Busch-Dienstfertig M, González-Rodríguez S, Maddila SC, Grobe J, Lipp M, et al. Cytotoxic T cells modulate inflammation and endogenous opioid analgesia in chronic arthritis. J Neuroinflammation. 2017;14(1):30. https://doi.org/10.1186/s12974-017-0804-y.
Rosen SF, Ham B, Haichin M, Walters IC, Tohyama S, Sotocinal SG, et al. Increased pain sensitivity and decreased opioid analgesia in T-cell-deficient mice and implications for sex differences. Pain. 2019;160(2):358–66. https://doi.org/10.1097/j.pain.0000000000001420.
Ji RR, Nackley A, Huh Y, Terrando N, Maixner W. Neuroinflammation and central sensitization in chronic and widespread pain. Anesthesiology. 2018;129(2):343–66. https://doi.org/10.1097/aln.0000000000002130.
Agalave NM, Rudjito R, Farinotti AB, Khoonsari PE, Sandor K, Nomura Y, et al. Sex-dependent role of microglia in disulfide high mobility group box 1 protein-mediated mechanical hypersensitivity. Pain. 2021;162(2):446–58. https://doi.org/10.1097/j.pain.0000000000002033.
Chacur M, Milligan ED, Gazda LS, Armstrong C, Wang H, Tracey KJ, et al. A new model of sciatic inflammatory neuritis (SIN): induction of unilateral and bilateral mechanical allodynia following acute unilateral peri-sciatic immune activation in rats. Pain. 2001;94(3):231–44. https://doi.org/10.1016/s0304-3959(01)00354-2.
Tanaka J, Seki Y, Ishikura H, Tsubota M, Sekiguchi F, Yamaguchi K, et al. Recombinant human soluble thrombomodulin prevents peripheral HMGB1-dependent hyperalgesia in rats. Br J Pharmacol. 2013;170(6):1233–41. https://doi.org/10.1111/bph.12396.
Shibasaki M, Sasaki M, Miura M, Mizukoshi K, Ueno H, Hashimoto S, et al. Induction of high mobility group box-1 in dorsal root ganglion contributes to pain hypersensitivity after peripheral nerve injury. Pain. 2010;149(3):514–21. https://doi.org/10.1016/j.pain.2010.03.023.
Zhang FF, Morioka N, Harano S, Nakamura Y, Liu K, Nishibori M, et al. Perineural expression of high-mobility group box-1 contributes to long-lasting mechanical hypersensitivity via matrix metalloprotease-9 up-regulation in mice with painful peripheral neuropathy. J Neurochem. 2016;136(4):837–50. https://doi.org/10.1111/jnc.13434.
Ren PC, Zhang Y, Zhang XD, An LJ, Lv HG, He J, et al. High-mobility group box 1 contributes to mechanical allodynia and spinal astrocytic activation in a mouse model of type 2 diabetes. Brain Res Bull. 2012;88(4):332–7. https://doi.org/10.1016/j.brainresbull.2012.03.002.
Feldman P, Due MR, Ripsch MS, Khanna R, White FA. The persistent release of HMGB1 contributes to tactile hyperalgesia in a rodent model of neuropathic pain. J Neuroinflammation. 2012;9(1):180. https://doi.org/10.1186/1742-2094-9-180.
Otoshi K, Kikuchi S, Kato K, Sekiguchi M, Konno S. Anti-HMGB1 neutralization antibody improves pain-related behavior induced by application of autologous nucleus pulposus onto nerve roots in rats. Spine. 2011;36(11):E692–8. https://doi.org/10.1097/BRS.0b013e3181ecd675.
Nakamura Y, Morioka N, Abe H, Zhang FF, Hisaoka-Nakashima K, Liu K, et al. Neuropathic pain in rats with a partial sciatic nerve ligation is alleviated by intravenous injection of monoclonal antibody to high mobility group box-1. PloS one. 2013;8(8):e73640. https://doi.org/10.1371/journal.pone.0073640.
Kokkola R, Sundberg E, Ulfgren AK, Palmblad K, Li J, Wang H, et al. High mobility group box chromosomal protein 1: a novel proinflammatory mediator in synovitis. Arthritis Rheum. 2002;46(10):2598–603. https://doi.org/10.1002/art.10540.
Taniguchi N, Kawahara K, Yone K, Hashiguchi T, Yamakuchi M, Goto M, et al. High mobility group box chromosomal protein 1 plays a role in the pathogenesis of rheumatoid arthritis as a novel cytokine. Arthritis Rheum. 2003;48(4):971–81. https://doi.org/10.1002/art.10859.
Hamada T, Torikai M, Kuwazuru A, Tanaka M, Horai N, Fukuda T, et al. Extracellular high mobility group box chromosomal protein 1 is a coupling factor for hypoxia and inflammation in arthritis. Arthritis Rheum. 2008;58(9):2675–85. https://doi.org/10.1002/art.23729.
Tassou A, Thouaye M, Gilabert D, Jouvenel A, Leyris JP, Sonrier C, et al. Activation of neuronal FLT3 promotes exaggerated sensorial and emotional pain-related behaviors facilitating the transition from acute to chronic pain. Progress in neurobiology. 2023;222:102405. https://doi.org/10.1016/j.pneurobio.2023.102405.
Rivat C, Sar C, Mechaly I, Leyris JP, Diouloufet L, Sonrier C, et al. Inhibition of neuronal FLT3 receptor tyrosine kinase alleviates peripheral neuropathic pain in mice. Nat Commun. 2018;9(1):1042. https://doi.org/10.1038/s41467-018-03496-2.
Kurosaki T, Kometani K, Ise W. Memory B cells. Nat Rev Immunol. 2015;15(3):149–59. https://doi.org/10.1038/nri3802.
Edwards JCW, Szczepański L, Szechiński J, Filipowicz-Sosnowska A, Emery P, Close DR, et al. Efficacy of B-cell–targeted therapy with rituximab in patients with rheumatoid arthritis. N Engl J Med. 2004;350(25):2572–81. https://doi.org/10.1056/NEJMoa032534.
Li WW, Guo TZ, Shi X, Czirr E, Stan T, Sahbaie P, et al. Autoimmunity contributes to nociceptive sensitization in a mouse model of complex regional pain syndrome. Pain. 2014;155(11):2377–89. https://doi.org/10.1016/j.pain.2014.09.007.
Costigan M, Moss A, Latremoliere A, Johnston C, Verma-Gandhu M, Herbert TA, et al. T-cell infiltration and signaling in the adult dorsal spinal cord is a major contributor to neuropathic pain-like hypersensitivity. J Neurosci. 2009;29(46):14415–22. https://doi.org/10.1523/jneurosci.4569-09.2009.
Schoggins JW, Rice CM. Interferon-stimulated genes and their antiviral effector functions. Curr Opin Virol. 2011;1(6):519–25. https://doi.org/10.1016/j.coviro.2011.10.008.
Huang L, Ou R, Rabelo de Souza G, Cunha TM, Lemos H, Mohamed E, et al. Virus Infections Incite Pain Hypersensitivity by Inducing Indoleamine 2,3 Dioxygenase. PLoS Pathog. 2016;12(5):e1005615. https://doi.org/10.1371/journal.ppat.1005615.
Gaelings L, Söderholm S, Bugai A, Fu Y, Nandania J, Schepens B, et al. Regulation of kynurenine biosynthesis during influenza virus infection. FEBS J. 2017;284(2):222–36. https://doi.org/10.1111/febs.13966.
Barragán-Iglesias P, Franco-Enzástiga Ú, Jeevakumar V, Shiers S, Wangzhou A, Granados-Soto V, et al. Type I interferons act directly on nociceptors to produce pain sensitization: implications for viral infection-induced pain. J Neurosci. 2020;40(18):3517. https://doi.org/10.1523/JNEUROSCI.3055-19.2020.
Nishimura T, Horino K, Nishiura H, Shibuya Y, Hiraoka T, Tanase S, et al. Apoptotic cells of an epithelial cell line, AsPC-1, release monocyte chemotactic S19 ribosomal protein dimer. J Biochem. 2001;129(3):445–54. https://doi.org/10.1093/oxfordjournals.jbchem.a002876.
Yamamoto T. Roles of the ribosomal protein S19 dimer and the C5a receptor in pathophysiological functions of phagocytic leukocytes. Pathol Int. 2007;57(1):1–11. https://doi.org/10.1111/j.1440-1827.2007.02049.x.
Shi X, Guo TZ, Li WW, Birklein F, Escolano FL, Herrnberger M, et al. C5a complement and cytokine signaling mediate the pronociceptive effects of complex regional pain syndrome patient IgM in fracture mice. Pain. 2021;162(5):1400–15. https://doi.org/10.1097/j.pain.0000000000002150.
Jang JH, Clark DJ, Li X, Yorek MS, Usachev YM, Brennan TJ. Nociceptive sensitization by complement C5a and C3a in mouse. Pain. 2010;148(2):343–52. https://doi.org/10.1016/j.pain.2009.11.021.
Clark JD, Qiao Y, Li X, Shi X, Angst MS, Yeomans DC. Blockade of the complement C5a receptor reduces incisional allodynia, edema, and cytokine expression. Anesthesiology. 2006;104(6):1274–82. https://doi.org/10.1097/00000542-200606000-00024.
Griffin RS, Costigan M, Brenner GJ, Ma CH, Scholz J, Moss A, et al. Complement induction in spinal cord microglia results in anaphylatoxin C5a-mediated pain hypersensitivity. J Neurosci. 2007;27(32):8699–708. https://doi.org/10.1523/jneurosci.2018-07.2007.
Wu SY, Fu T, Jiang YZ, Shao ZM. Natural killer cells in cancer biology and therapy. Mol Cancer. 2020;19(1):120. https://doi.org/10.1186/s12943-020-01238-x.
Ritz BW, Alexander GM, Nogusa S, Perreault MJ, Peterlin BL, Grothusen JR, et al. Elevated blood levels of inflammatory monocytes (CD14+ CD16+ ) in patients with complex regional pain syndrome. Clin Exp Immunol. 2011;164(1):108–17. https://doi.org/10.1111/j.1365-2249.2010.04308.x.
Brennan PC, Graham MA, Triano JJ, Hondras MA, Anderson RJ. Lymphocyte profiles in patients with chronic low back pain enrolled in a clinical trial. J Manipulative Physiol Ther. 1994;17(4):219–27.
Landis CA, Lentz MJ, Tsuji J, Buchwald D, Shaver JL. Pain, psychological variables, sleep quality, and natural killer cell activity in midlife women with and without fibromyalgia. Brain Behav Immun. 2004;18(4):304–13. https://doi.org/10.1016/j.bbi.2003.11.001.
Sato N, Kikuchi S, Sato K. Quantifying the stress induced by distress in patients with lumbar disc herniation in terms of natural killer cell activity measurements: chromium release assay versus multiparameter flow cytometric assay. Spine. 2002;27(19):2095–100. https://doi.org/10.1097/00007632-200210010-00004.
Yoon JJ, Song JA, Park SY, Choi JI. Cytotoxic activity and subset populations of peripheral blood natural killer cells in patients with chronic pain. Korean J Pain. 2018;31(1):43–9. https://doi.org/10.3344/kjp.2018.31.1.43.
Lassen J, Stürner KH, Gierthmühlen J, Dargvainiene J, Kixmüller D, Leypoldt F, et al. Protective role of natural killer cells in neuropathic pain conditions. Pain. 2021;162(9):2366–75. https://doi.org/10.1097/j.pain.0000000000002274.
Kerkhoff C, Klempt M, Kaever V, Sorg C. The two calcium-binding proteins, S100A8 and S100A9, are involved in the metabolism of arachidonic acid in human neutrophils. J Biol Chem. 1999;274(46):32672–9. https://doi.org/10.1074/jbc.274.46.32672.
Jang Y, Kim M, Hwang SW. Molecular mechanisms underlying the actions of arachidonic acid-derived prostaglandins on peripheral nociception. J Neuroinflammation. 2020;17(1):30. https://doi.org/10.1186/s12974-020-1703-1.
Schäfers M, Marziniak M, Sorkin LS, Yaksh TL, Sommer C. Cyclooxygenase inhibition in nerve-injury- and TNF-induced hyperalgesia in the rat. Exp Neurol. 2004;185(1):160–8. https://doi.org/10.1016/j.expneurol.2003.09.015.
Sekiguchi M, Otoshi K, Kikuchi S, Konno S. Analgesic effects of prostaglandin E2 receptor subtype EP1 receptor antagonist: experimental study of application of nucleus pulposus. Spine. 2011;36(22):1829–34. https://doi.org/10.1097/BRS.0b013e3181fa1fca.
Ma K, Zhou Q-h, Chen J, Du D-p, Ji Y, Jiang W. TTX-R Na+ current-reduction by celecoxib correlates with changes in PGE2 and CGRP within rat DRG neurons during acute incisional pain. Brain Res. 2008;1209:57–64. https://doi.org/10.1016/j.brainres.2008.02.096.
Amaya F, Samad TA, Barrett L, Broom DC, Woolf CJ. Periganglionic inflammation elicits a distally radiating pain hypersensitivity by promoting COX-2 induction in the dorsal root ganglion. Pain. 2009;142(1–2):59–67. https://doi.org/10.1016/j.pain.2008.11.013.
Fritz G. RAGE: a single receptor fits multiple ligands. Trends Biochem Sci. 2011;36(12):625–32. https://doi.org/10.1016/j.tibs.2011.08.008.
Hofmann MA, Drury S, Fu C, Qu W, Taguchi A, Lu Y, et al. RAGE mediates a novel proinflammatory axis: a central cell surface receptor for S100/calgranulin polypeptides. Cell. 1999;97(7):889–901. https://doi.org/10.1016/S0092-8674(00)80801-6.
Kokkola R, Andersson A, Mullins G, Ostberg T, Treutiger CJ, Arnold B, et al. RAGE is the major receptor for the proinflammatory activity of HMGB1 in rodent macrophages. Scand J Immunol. 2005;61(1):1–9. https://doi.org/10.1111/j.0300-9475.2005.01534.x.
Mogil JS. Qualitative sex differences in pain processing: emerging evidence of a biased literature. Nat Rev Neurosci. 2020;21(7):353–65. https://doi.org/10.1038/s41583-020-0310-6.
Cowie AM, Menzel AD, O’Hara C, Lawlor MW, Stucky CL. NOD-like receptor protein 3 inflammasome drives postoperative mechanical pain in a sex-dependent manner. Pain. 2019;160(8):1794–816. https://doi.org/10.1097/j.pain.0000000000001555.
Baskozos G, Dawes JM, Austin JS, Antunes-Martins A, McDermott L, Clark AJ, et al. Comprehensive analysis of long noncoding RNA expression in dorsal root ganglion reveals cell-type specificity and dysregulation after nerve injury. Pain. 2019;160(2):463–85. https://doi.org/10.1097/j.pain.0000000000001416.
Mecklenburg J, Wangzhou A, Hovhannisyan AH, Barba-Escobedo P, Shein SA, Zou Y, et al. Sex-dependent pain trajectories induced by prolactin require an inflammatory response for pain resolution. Brain Behav Immun. 2022;101:246–63. https://doi.org/10.1016/j.bbi.2022.01.016.
Sorge RE, Mapplebeck JCS, Rosen S, Beggs S, Taves S, Alexander JK, et al. Different immune cells mediate mechanical pain hypersensitivity in male and female mice. Nat Neurosci. 2015;18(8):1081–3. https://doi.org/10.1038/nn.4053.
Plumb AN, Lesnak JB, Berardi G, Hayashi K, Janowski AJ, Smith AF, et al. Standing on the shoulders of bias: lack of transparency and reporting of critical rigor characteristics in pain research. Pain. 2023. https://doi.org/10.1097/j.pain.0000000000002874.
Funding
This work was supported by NIH grant U19NS130608.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lesnak, J.B., Mazhar, K. & Price, T.J. Neuroimmune Mechanisms Underlying Post-acute Sequelae of SARS-CoV-2 (PASC) Pain, Predictions from a Ligand-Receptor Interactome. Curr Rheumatol Rep 25, 169–181 (2023). https://doi.org/10.1007/s11926-023-01107-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11926-023-01107-8