Abstract
Purpose of Review
This paper covers confusion and challenges in the nomenclature of calcium pyrophosphate deposition disease. Clinicians, investigators, and patients are faced with a variety of terms that are used to describe CPPD and its phenotypes, and clarity is greatly needed to help advance research and patient care. Motivation for the upcoming development of CPPD classification criteria is reviewed.
Recent Findings
EULAR proposed recommended terminology for CPPD in 2011. International Classification of Diseases (ICD-9 and ICD-10) billing codes identify definite or probable CPPD with variable accuracy depending on the clinical setting and comparator group. READ diagnostic codes have been employed to identify pseudogout in UK datasets but their accuracy has not been evaluated. CPPD classification criteria will provide a system for identifying a relatively homogenous group of patients to be included in clinical studies, enabling comparison of outcomes across studies.
Summary
CPPD nomenclature remains challenging for clinicians, investigators, and patients. A lay-friendly definition of CPPD, using easily accessible terminology, would be welcome. CPPD classification criteria are a necessary step in moving forward CPPD clinical research and may involve a range of clinical, laboratory, and imaging modalities.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Abhishek A, Neogi T, Choi H, Doherty M, Rosenthal AK, Terkeltaub R. Review: unmet needs and the path forward in joint disease associated with calcium pyrophosphate crystal deposition. Arthritis & rheumatology. 2018;70:1182–91 This review highlights challenges to advancing the research agenda in CPPD, including the lack of classification criteria.
McCarty DJ, Kohn NN, Faires JS. The significance of calcium phosphate crystals in the synovial fluid of arthritic patients: the “pseudogout syndrome”: I. clinical aspects. Ann Intern Med. 1962;56:711–37.
Kohn NN, Hughes RE, McCarty DJ, Faires JS. The significance of calcium phosphate crystals in the synovial fluid of arthritic patients: the “pseudogout syndrome”. Ann Intern Med. 1962;56:738–45.
Rosenthal AK, Ryan LM. Calcium pyrophosphate deposition disease. N Engl J Med. 2016;374:2575–84.
Zhang W, Doherty M, Bardin T, Barskova V, Guerne PA, Jansen TL, et al. European League Against Rheumatism recommendations for calcium pyrophosphate deposition. Part I: terminology and diagnosis. Ann Rheum Dis. 2011;70:563–70.
Ryan L, McCarty D. Calcium pyrophosphate crystal deposition disease; pseudogout; articular chondrocalcinosis. In: McCarty D, editor. Arthritis and allied conditions. 10th ed. Philadelphia: Lea & Febiger; 1985. p. 1515–46.
McCarty DJ. Calcium pyrophosphate dihydrate crystal deposition disease: nomenclature and diagnostic criteria. Ann Intern Med. 1977;87:241–2.
Bursill D, Taylor WJ, Terkeltaub R, Kuwabara M, Merriman TR, Grainger R, et al. Gout, hyperuricemia, and crystal-associated disease network consensus statement regarding labels and definitions for disease elements in gout. Arthritis care & research. 2019;71:427–34.
van der Heijde D, Daikh DI, Betteridge N, et al. Common language description of the term rheumatic and musculoskeletal diseases (RMDs) for use in communication with the lay public, healthcare providers, and other stakeholders endorsed by the European League Against Rheumatism (EULAR) and the American College of Rheumatology (ACR). Arthritis & rheumatology. 2018;70:826–31.
Tanikawa H, Ogawa R, Okuma K, Harato K, Niki Y, Kobayashi S, et al. Detection of calcium pyrophosphate dihydrate crystals in knee meniscus by dual-energy computed tomography. J Orthop Surg Res. 2018;13:73.
Utsinger PD, Resnick D, Zvaifler NJ. Wrist arthropathy in calcium pyrophosphate dihydrate deposition disease. Arthritis Rheum. 1975;18:485–91.
Lee KA, Lee SH, Kim HR. Diagnostic value of ultrasound in calcium pyrophosphate deposition disease of the knee joint. Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society 2019;27:781–787.
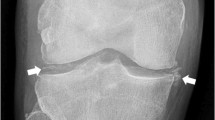
Barskova VG, Kudaeva FM, Bozhieva LA, Smirnov AV, Volkov AV, Nasonov EL. Comparison of three imaging techniques in diagnosis of chondrocalcinosis of the knees in calcium pyrophosphate deposition disease. Rheumatology. 2013;52:1090–4.
Filippou G, Adinolfi A, Iagnocco A, Filippucci E, Cimmino MA, Bertoldi I, et al. Ultrasound in the diagnosis of calcium pyrophosphate dihydrate deposition disease. A systematic literature review and a meta-analysis. Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society. 2016;24:973–81.
Gamon E, Combe B, Barnetche T, Mouterde G. Diagnostic value of ultrasound in calcium pyrophosphate deposition disease: a systematic review and meta-analysis. RMD Open. 2015;1:e000118.
Pascart T, Norberciak L, Legrand J, Becce F, Budzik JF. Dual-energy computed tomography in calcium pyrophosphate deposition: initial clinical experience. Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society. 2019.
Stamp LK, Anderson NG, Becce F, Rajeswari M, Polson M, Guyen O, et al. Clinical utility of multi-energy spectral photon-counting computed tomography in crystal arthritis. Arthritis & rheumatology. 2019.
O’Malley KJ, Cook KF, Price MD, Wildes KR, Hurdle JF, Ashton CM. Measuring diagnoses: ICD code accuracy. Health Serv Res. 2005;40:1620–39.
Nigwekar SU, Solid CA, Ankers E, et al. Quantifying a rare disease in administrative data: the example of calciphylaxis. J Gen Intern Med. 2014;29(Suppl 3):S724–31.
•• Bartels CM, Singh JA, Parperis K, Huber K, Rosenthal AK. Validation of administrative codes for calcium pyrophosphate deposition: a Veterans Administration study. Journal of clinical rheumatology : practical reports on rheumatic & musculoskeletal diseases. 2015;21:189–92 This is the first administrative claims–based algorithm for CPPD.
Kleiber Balderrama C, Rosenthal AK, Lans D, Singh JA, Bartels CM. Calcium pyrophosphate deposition disease and associated medical comorbidities: a National Cross-Sectional Study of US veterans. Arthritis Care & Research. 2017;69:1400–6.
Tedeschi SK, Solomon DH, Liao KP. Pseudogout among patients fulfilling a billing code algorithm for calcium pyrophosphate deposition disease. Rheumatol Int. 2018;38:1083–8.
Rho YH, Zhu Y, Zhang Y, Reginato AM, Choi HK. Risk factors for pseudogout in the general population. Rheumatology. 2012;51:2070–4.
Roddy E, Muller S, Paskins Z, Hider SL, Blagojevic-Bucknall M, Mallen CD. Incident acute pseudogout and prior bisphosphonate use: matched case-control study in the UK. Clinical Practice Research Datalink Medicine (Baltimore). 2017;96:e6177.
Herrett E, Thomas SL, Schoonen WM, Smeeth L, Hall AJ. Validation and validity of diagnoses in the general practice research database: a systematic review. Br J Clin Pharmacol. 2010;69:4–14.
Aggarwal R, Ringold S, Khanna D, Neogi T, Johnson SR, Miller A, et al. Distinctions between diagnostic and classification criteria? Arthritis care & Research. 2015;67:891–7.
Neogi T, Jansen TL, Dalbeth N, et al. Gout classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis & rheumatology. 2015;2015(67):2557–68.
Aletaha D, Neogi T, Silman AJ, et al. Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis and Rheumatism. 2010;2010(62):2569–81.
Tedeschi SK, Johnson SR, Boumpas DT, Daikh D, Dörner T, Diamond B, et al. Multicriteria decision analysis process to develop new classification criteria for systemic lupus erythematosus. Ann Rheum Dis. 2019;78:634–40.
Singh G, Lingala B, Mithal A. Gout and hyperuricaemia in the USA: prevalence and trends. Rheumatology. 2019.
Vargas-Santos AB, Taylor WJ, Neogi T. Gout classification criteria: update and Implications. Curr Rheumatol Rep. 2016;18:46.
• Berendsen D, Neogi T, Taylor WJ, Dalbeth N, Jansen TL. Crystal identification of synovial fluid aspiration by polarized light microscopy. An online test suggesting that our traditional rheumatologic competence needs renewed attention and training. Clinical Rheumatology. 2017;36:641–7 This study identified that CPP crystals were less accurately identified than monosodium urate crystals via images from polarized light microscopy.
Swan A, Amer H, Dieppe P. The value of synovial fluid assays in the diagnosis of joint disease: a literature survey. Ann Rheum Dis. 2002;61:493–8.
Andres M, Vela P, Jovani V, Pascual E. Most needle-shaped calcium pyrophosphate crystals lack birefringence. Rheumatology. 2019;58:1095–8.
Zell M, Zhang D, FitzGerald J. Diagnostic advances in synovial fluid analysis and radiographic identification for crystalline arthritis. Curr Opin Rheumatol. 2019;31:134–43.
McCarthy GM, Dunne A. Calcium crystal deposition diseases - beyond gout. Nat Rev Rheumatol. 2018;14:592–602.
•• Filippou G, Scire CA, Damjanov N, et al. Definition and reliability assessment of elementary ultrasonographic findings in calcium pyrophosphate deposition disease: a study by the OMERACT calcium pyrophosphate deposition disease ultrasound subtask force. J Rheumatol. 2017;44:1744–9 This manuscript presents the OMERACT ultrasound definitions for CPPD in the fibrocartilage, hyaline cartilage, tendon, and synovial fluid.
Filippou G, Scire CA, Adinolfi A, et al. Identification of calcium pyrophosphate deposition disease (CPPD) by ultrasound: reliability of the OMERACT definitions in an extended set of joints-an international multiobserver study by the OMERACT Calcium Pyrophosphate Deposition Disease Ultrasound Subtask Force. Ann Rheum Dis. 2018;77:1194–9.
Misra D, Guermazi A, Sieren JP, Lynch J, Torner J, Neogi T, et al. CT imaging for evaluation of calcium crystal deposition in the knee: initial experience from the Multicenter Osteoarthritis (MOST) study. Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society. 2015;23:244–8.
Diekhoff T, Kiefer T, Stroux A, Pilhofer I, Juran R, Mews J, et al. Detection and characterization of crystal suspensions using single-source dual-energy computed tomography: a phantom model of crystal arthropathies. Investig Radiol. 2015;50:255–60.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Sara K. Tedeschi is a member of the ACR/EULAR CPPD Classification Criteria team.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Crystal Arthritis
Rights and permissions
About this article
Cite this article
Tedeschi, S.K. Issues in CPPD Nomenclature and Classification. Curr Rheumatol Rep 21, 49 (2019). https://doi.org/10.1007/s11926-019-0847-4
Published:
DOI: https://doi.org/10.1007/s11926-019-0847-4